Abstract
Numb chin syndrome (NCS), also known as mental nerve neuropathy, is characterized by facial and oral numbness restricted to the distribution of the mental nerve. Although not a common neuropathy, the clinical importance of this syndrome is its frequent association with malignancies. A 56-year-old Indian female reported with a complaint of numbness on the left side of chin. She had undergone a radical mastectomy with axillary lymph node dissection for invasive ductal carcinoma of the right breast 4 years ago. Biopsy revealed tumor cells showing pleomorphic hyperchromatic nuclei arranged in cord and nests leading to a diagnosis of metastatic carcinoma of breast origin. Bone scan showed increased uptake in multiple areas in skull, left hemimandible, multiple vertebrae, multiple ribs on either sides, right clavicle both scapulae and sternum, both humeri, multiple pelvic bones and trochanteric region of left femur. The patient was referred to a tertiary cancer institute where she received palliative hormonal and chemotherapy, which helped with her pain and halted the progression of the metastatic disease for past 22 months. The present case depicts the importance of proper recognition of NCS as it may often be the only symptom of an underlying malignancy or the first evidence of dissemination from a primary site as evident in this case.
Keywords: Invasive ductal carcinoma, mental nerve neuropathy, metastatic breast carcinoma, numb chin syndrome
INTRODUCTION
Numb chin syndrome (NCS), also known as mental nerve neuropathy, is characterized by facial and oral numbness restricted to the distribution of the mental nerve.[1] Although not a common neuropathy, the clinical importance of this syndrome lies in its frequent association with various malignancies occurring in the human body. While many of these malignancies are associated with other physical signs or symptoms, numb chin often presents as the initial symptom and awareness of this physical finding should raise suspicion for an underlying malignancy and may even contribute to earlier detection. Thus, NCS may be the first presentation of an underlying malignancy and may also be the first sign of recurrence or metastasis in patients with a history of malignancy.
CASE REPORT
A 56-year-old Indian female presented with numbness of the lower lip and chin on the left side to the Department of Oral Medicine and Radiology. She also complained of pain of left side of the lower jaw during the lateral excursion. Her symptoms started 10 days back for which she underwent extraction of mandibular second molar on the left side. This failed to improve her symptoms and then she reported to our institution for further investigation. She was not on any medication and there was no history of any recent trauma to the jaws. Her medical history revealed that the patient had undergone a radical mastectomy with axillary lymph node dissection 4 years back along with radiotherapy for invasive ductal carcinoma of the right breast. The patient had no complaints thereafter for the past 4 years. No relevant intraoral findings were detected. Regional lymph nodes were not palpable.
The radiographic examination with panoramic radiograph revealed radiolucency with ill-defined borders measuring 15 mm × 10 mm apical and distal to 37 area [Figure 1]. An incisional biopsy was taken under local anesthesia. Sections from the biopsied material, stained with hematoxylin and eosin, revealed a delicate to moderately collagenous stromal tissue showing the presence of cords of tumor cells with pleomorphic hyperchromatic nuclei and moderate amount of cytoplasm [Figure 2]. Cells were also arranged in irregular nests and glandular islands [Figure 3]. These histological results supported evidence of metastatic invasive ductal carcinoma.
Figure 1.

Panoramic radiograph revealing radiolucency with ill-defined borders measuring 15 mm × 10 mm apical and distal to 37
Figure 2.
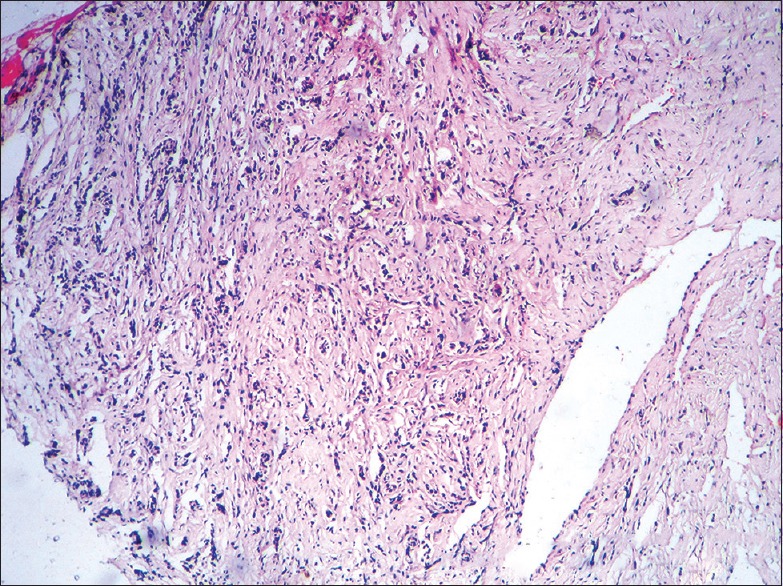
Photomicrograph showing cords of tumor cells showing pleomorphic hyperchromatic nuclei (H&E stain, x100)
Figure 3.
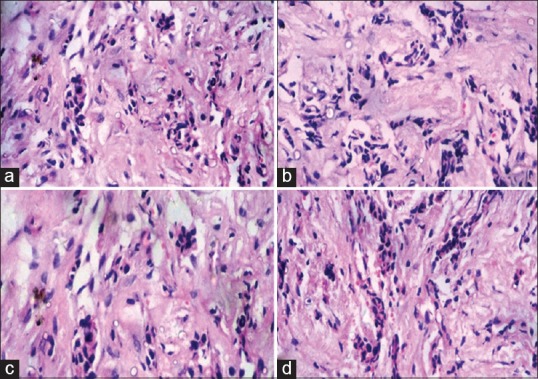
(a-d) Photomicrographs showing cells arranged in irregular nests and islands. (H&E stain, x400)
Subsequently, a bone scintigraphic image of the whole body was obtained. Technetium bone scintigraphy showed increased uptake in multiple areas in skull, left hemimandible, multiple vertebrae, multiple ribs on either sides, right clavicle both scapulae and sternum, both humeri, multiple pelvic bones and trochanteric region of left femur [Figure 4]. The patient was referred to a tertiary cancer institute where she received palliative hormonal therapy and chemotherapy, which helped with her pain and halted progression of the metastatic disease for past 22 months.
Figure 4.
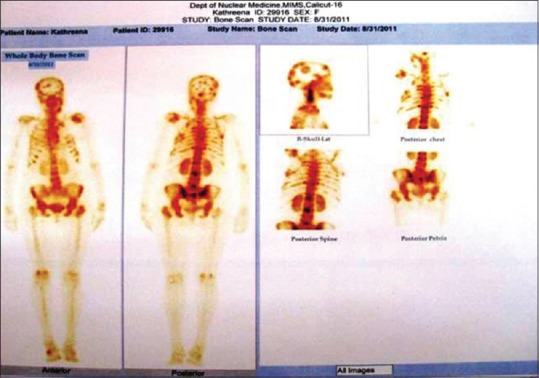
Bone scan showing widespread disseminated skeletal metastatic state
DISCUSSION
Mental neuropathy associated with malignancy was first referred to as NCS in 1963 by Calverley and Mohnac, who reported five patients with metastatic malignant disease initially presented with NCS. This syndrome has since been reported in various malignant diseases, including lymphoma, acute leukemia, Burkitt lymphoma/leukemia, multiple myeloma, Ewing sarcoma, melanoma, breast cancer, prostate cancer, lung cancer, colon cancer and esophageal cancer.[1] NCS has been also linked with immune-mediated systemic conditions such as temporal arteritis, vasculitis, multiple sclerosis, Sjogren's syndrome and sickle cell crisis.[2]
NCS is thought to be mainly due to the involvement of the mandibular nerve either intra or extracranially. In cases with extracranial involvement, the most common etiology is the involvement of the inferior alveolar nerve within the mandible. This can result from mechanical nerve compression caused by osseous involvement of mandible or from nerve damage caused by tumor infiltration along the nerve sheath. In cases depicting intracranial involvement, the pathogenesis of NCS can be either involvement of the trigeminal nerve root by meningeal carcinomatosis or direct infiltration of malignant cells into the trigeminal nerve.[3]
NCS may be the first presentation of malignancy in up to 47% of patients.[4] It may also be the first symptom of metastatic disease. Lossos and Siegal reported that in 67% of their 42 patients, NCS was associated with disease progression and in 31% NCS was the first symptom of tumor relapse.[4] It is important to remember that lack of radiographic changes cannot exclude the possibility of small metastatic lesions in the jaw.[4] Microscopic infiltration of a nerve can elicit symptoms much before the tumor becomes clinically detectable.
It is still unclear how specific this clinical sign is for malignancy and whether the identification of malignancy based on diagnostic workup done because of this sign would affect the survival of the patient. Prognosis of patients with NCS as a result of malignancy is very poor with survival being measured in months.[5] Median survival following diagnosis can be as little as 5 months if NCS is caused by bone metastasis and 12 months if associated with leptomeningeal seeding.[4] Treatment of NCS is provided by treating the underlying cause and management of symptoms.
The management of metastatic carcinomas of the oral cavity which are mostly the prime cause of NCS is primarily palliative which includes radiotherapy, chemotherapy, hormone therapy and very rarely, surgical intervention. The major goals of the management should be proper pain relief and control of possible infections and fractures. The prognosis for patients with metastatic lesions to the oral cavity is generally poor, chiefly because of the delay in the detection of the lesions. The average survival time for patients with metastatic tumors in the oral cavity is 6–7 months; with approximately 70% of patients dying within 1-year of diagnosis.[6]
In summary, the present paper illustrates the importance of medical history and careful evaluation of unusual clinical and radiographic findings such as lip and chin paresthesia in the diagnosis of systemic condition. Even though the patient in the above-reported case had multiple metastases throughout the body, NCS was the initial and sole symptom leading to the diagnosis of metastatic stage. Thus, the discovery of NCS in a patient with a history of malignancy should alert the clinician with the possibility of a disseminated disease which would help to avoid unnecessary delay in the workup and management.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Sasaki M, Yamazaki H, Aoki T, Ota Y, Sekiya R, Kaneko A. Bilateral numb chin syndrome leading to a diagnosis of Burkitt's cell acute lymphocytic leukemia: A case report and literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:e11–6. doi: 10.1016/j.tripleo.2010.09.066. [DOI] [PubMed] [Google Scholar]
- 2.Abilleira S, Bowler JV. The numb chin syndrome as an early manifestation of giant-cell (temporal) arteritis: A case report. Headache. 2005;45:1411–3. doi: 10.1111/j.1526-4610.2005.00276_1.x. [DOI] [PubMed] [Google Scholar]
- 3.Kuroda Y, Fujiyama F, Ohyama T, Watanabe T, Endo C, Neshige R, et al. Numb chin syndrome secondary to Burkitt's cell acute leukemia. Neurology. 1991;41:453–4. doi: 10.1212/wnl.41.3.453. [DOI] [PubMed] [Google Scholar]
- 4.Lossos A, Siegal T. Numb chin syndrome in cancer patients: Etiology, response to treatment and prognostic significance. Neurology. 1992;42:1181–4. doi: 10.1212/wnl.42.6.1181. [DOI] [PubMed] [Google Scholar]
- 5.Baskaran RK, Krishnamoorthy, Smith M. Numb chin syndrome – A reflection of systemic malignancy. World J Surg Oncol. 2006;4:52. doi: 10.1186/1477-7819-4-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hirshberg A, Shnaiderman-Shapiro A, Kaplan I, Berger R. Hirshberg A, Shnaiderman-Shapiro A, Kaplan I, Berger R, editors. Metastatic tumours to the oral cavity: Pathogenesis and analysis of 673 cases. Oral Oncol 2008; 44. Metastatic tumours to the oral cavity – Pathogenesis and analysis of 673 cases. Oral Oncol. 2008;44:743–52. doi: 10.1016/j.oraloncology.2007.09.012. [DOI] [PubMed] [Google Scholar]


