Abstract
Oral squamous cell carcinoma (OSCC) is the most common epithelial malignant neoplasm affecting the oral cavity; early detection is an important criterion for achieving high cure rate. Occasionally, it may be misdiagnosed because of its variable and innocuous clinical appearance. Carcinomas of the gingiva are a unique subset of OSCC, constituting approximately 10% of OSCCs and can mimic a multitude of oral lesions especially those of inflammatory origin with benign features, often leading to delay in the diagnosis and hence delayed treatment. This article reports a rare case of gingival OSCC in a 62-year-old female patient mimicking an inflammatory gingival mass.
Keywords: Early detection, gingival mass, oral cancer, squamous cell carcinoma
INTRODUCTION
Oral squamous cell carcinoma (OSCC) is one of the most aggressive malignancies worldwide and accounts for more than 90% of all oral cancers. It is ranked as the sixth leading cause of cancer mortality worldwide and the second leading cause of cancer mortality in India.[1] The most common sites of OSCC are the lateral ventral surface of the tongue, the floor of the mouth and buccal mucosa. A less frequent site to be affected is the gingiva which comprises of about 10% of all OSCCs and affects 91% of patients with gingival carcinoma aged above 66 years.[2,3]
Of all the intraoral carcinomas, gingival OSCC is least associated with tobacco abuse and has the greatest predilection for females. However, few other authors have reported a male predominance. After these contradictory reports, it was suggested to analyze the cause of the male dominant tendency of gingival squamous cell carcinoma (SCC) in Asian patients.[4]
These tumors commonly arise in the edentulous areas, although they may also develop at dentate areas. It is generally agreed that carcinomas of the mandibular gingiva are more common than those of the maxillary gingiva and 60% of those are located posterior to the premolars. Although generally classified as a subset of OSCC, gingival SCC is a unique malignancy and can mimic a multitude of other lesions, especially those of inflammatory origin. Clinical presentations of SCCs of the gingiva can be quite variable and hence are misdiagnosed as benign tumors or other inflammatory responses. The 5-year survival rate of gingival SCC is considerably less as compared to SCC developing at other sites, suggesting a poor prognosis.[5]
Hence, SCC of the gingiva should be considered in the differential diagnosis while dealing with gingival lesions particularly in elderly individuals and is of paramount importance that the lesion be diagnosed early to initiate treatment and thereby improve prognosis.
CASE REPORT
A 62-year-old female patient reported to a private dental clinic with pain in the right lower back tooth region for the past 2 weeks. Intraoral examination revealed the presence of reddish buccal gingival growth in relation to mesial aspect of tooth no. 47 measuring approximately 0.5 cm × 0.5 cm. Grade III mobility was evident in 47. The rest of the dentition exhibited generalized chronic periodontitis. The patient gave no history of tobacco usage in any form. Extraoral examination revealed a single palpable, nontender, mobile and firm submandibular lymph node on the right side. On the basis of above findings, the buccal growth was provisionally diagnosed as an inflammatory/reactive gingival growth and apical periodontitis in relation to 47. Since the patient insisted only on symptomatic medical management, she was prescribed antibiotics, analgesics and chlorhexidine mouthwash for 3 days. A complete hemogram and biochemical assay for blood sugar was requested and the patient was asked to report after a week. One week recall visit revealed unsatisfactory healing and blood investigation reports were all within normal limits, excepting a slightly elevated erythrocyte sedimentation rate. Due to the persistence of the lesion and poor response to medical therapy a likelihood of noninfectious and noninflammatory pathology was strongly suspected. Since the patient did not want any further conservative management and insisted on an extraction, the dentist decided to extract the tooth. Considering the innocuous appearance of the lesion, perceived lack of risk factors and the patients’ insistence of symptomatic management and unwillingness of the patient to undergo any radiographic examination, the dentist requested for an expert opinion from the speciality services. Considering the age of the patient, ambiguous clinical presentation and the refractory nature of the lesion, a differential diagnosis of OSCC and metastatic carcinoma to the gingiva was considered. Only after the expert opinion and counselling by the specialist, did the patient agree for immediate biopsy along with extraction and the radiograph was taken only on follow-up.
On the 2nd week recall, the patient reported with the panoramic radiograph and presented with a rapidly growing soft tissue mass in the extracted site. Clinical intraoral examination revealed an ovoid reddish, spongy mass measuring about 1 cm × 1 cm from the extracted site [Figure 1]. Orthopantomogram did not reveal any remarkable findings [Figure 2].
Figure 1.

Two weeks postextraction shows reddish, ovoid growth on the posterior alveolar ridge
Figure 2.

Orthopantomogram showing the extracted site (right mandible) with no osseous changes
Histopathological examination revealed islands and sheets of dysplastic epithelium invading into the underlying connective tissue stroma with keratin pearl formation. The overlying epithelium showed hyperkeratinized stratified squamous epithelium with dysplastic features suggesting a diagnosis of well-differentiated SCC [Figures 3–5].
Figure 3.
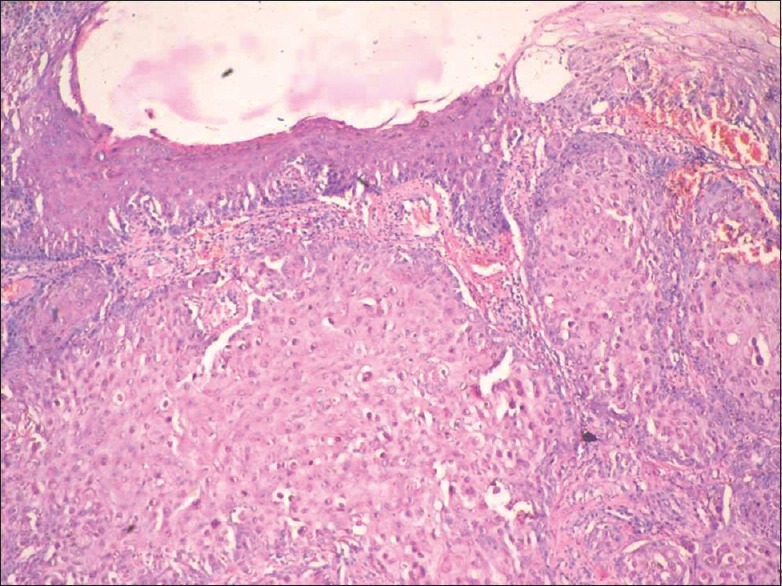
Photomicrograph showing squamous epithelium with islands of dysplastic cells infiltrating the connective tissue (H&E stain, x40)
Figure 5.
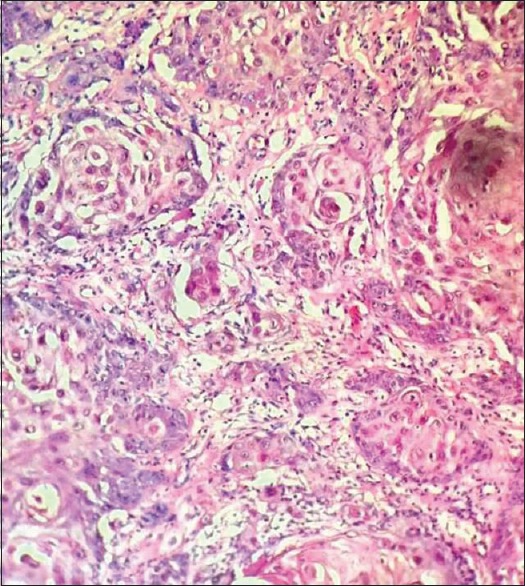
High power view showing island and nests of squamous epithelial cells within the connective tissue (H&E, x400)
Figure 4.
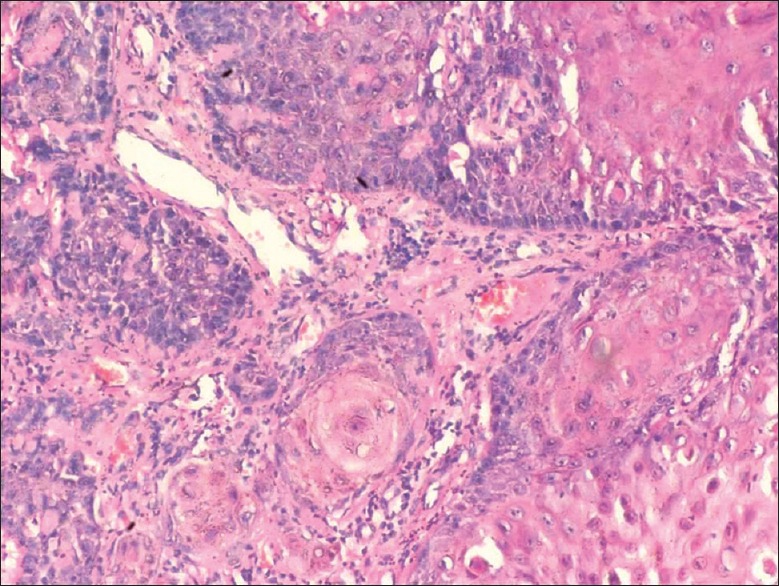
Photomicrograph showing well-differentiated squamous epithelial islands within the connective tissue (H&E stain, x100)
The patient was referred to cancer speciality hospital for further management. A whole body positron emission tomography scan was done to rule out secondaries. The patient was administered radiotherapy fractionated at 60 Gy each session for a period of 5 weeks. The patient is continuously under follow-up 6 months postradiation and does not show any signs of recurrence [Figure 6].
Figure 6.

One-month postradiation intra-oral image showing no evidence of the lesion
DISCUSSION
Oral cancer is a major global public health problem with 5,00,000 new cases diagnosed annually. According to the International Classification of Diseases, oral cancer refers to a subgroup of head and neck malignancies that develop on the lips, tongue, salivary glands, gingiva, floor of the mouth, oropharynx, buccal surfaces and other intraoral locations. Nevertheless, the term is synonymous to OSCC of oral mucosal origin.[6]
Despite rapid advances in treatment modalities, oral cancer still remains a life-threatening disease with no remarkable improvement in prognosis and survival. This is primarily attributed to delayed diagnosis or misdiagnosis.
The oral cavity is amenable to routine screening and clinical examination for malignant changes and therefore, in theory, these changes should be more easily detected and diagnosed at early stages leading to more effective treatment.[7] However, because of its varied site-related clinical presentation malignant oral disease is often difficult to distinguish from benign oral lesions.
Carcinoma of the gingiva is an insidious disease, does not have the clinical appearance of a malignant neoplasm and is often misdiagnosed as one of the many inflammatory lesions of the periodontium. Gingival carcinoma typically arises from keratinized mucosa, most often in the posterior mandible, where it destroys the underlying bone structure causing tooth mobility.[8]
The most common etiologic factors associated with OSCC are smoking and smokeless tobacco, which increases the general risk fourfold. Of all the intraoral carcinomas, gingival OSCC is least associated with tobacco abuse and has the greatest predilection for females. Other causes include phenol use, exposure to ultraviolet radiation, iron deficiency, candidal infections, oncogenic viruses and immunosuppression which may play much smaller roles.[9]
Gingival SCC more frequently involves mandible than maxilla and is predominantly observed in older females over 50 years. Gingival OSCC is more aggressive and in its early stage bears a resemblance to common mucosal infection and, therefore, has frequently led to a delay in diagnosis or misdiagnosis, leading to delay in treatment and making the prognosis grave. Gingival SCCs carry a higher risk of metastases owing to its proximity to the underlying periosteum and bone which invites early invasion of these structures.[2]
As such, gingival SCC is diagnosed late, due its similarity with other common inflammatory lesions of the gingiva, invasive procedures such as curettage and extraction of the tooth worsens the prognosis, a hypothesis first suggested by Peterson (1993) and it has been suggested that dissemination of cancer cells into the circulation during invasive procedures could increase the risks of distant metastases.[10]
Eun–Joo Choi et al. studied the prognosis of gingival OSCCs in dentate patients diagnosed after invasive procedures such as curettage and extraction and found that bone invasion was seen in 75.8% patients who underwent invasive procedures and in the remaining 24.2% patients bone invasion was not demonstrated probably because the procedure included removal of floating teeth without curettage. This result suggests that removal of floating teeth without curettage may not disseminate the cancer cells into the bone marrow.[4]
In this reported case, which was also initially misdiagnosed as an inflammatory mass, subsequently an atraumatic extraction was done for the mobile tooth based on the expert opinion. Such a cautious approach has to be exercised in the management of such suspicious lesions with an eye on prevention of untoward events. However, even in the current case the outcome of the treatment has to be viewed with caution, as the patient is only in the 6th month follow-up period.
The prognosis with gingival carcinomas depends on the histological subtype and clinical extent of the tumor. A well-differentiated type such as in our case is generally considered to have a favorable prognosis. However, the most important indicator of the prognosis is the clinical stage of the disease. If the neoplasm is small and localized, the 5-year cure rate is around 60%~70%; however if cervical nodal metastasis occurs, the survival rate drops to about 25% suggesting that early diagnosis is imperative.
Early detection of SCC is vital as the prognosis is directly related to the size of the lesion. Lesions measuring <1 cm are amenable to treatment and have a long-term prognosis. Thus, it is prudent to biopsy any unexplained lesion which remains after 2 weeks following removal of any suspected etiologic agent to avoid unnecessary delay in diagnosing such conditions.
CONCLUSION
The general dentist is frequently presented with oral lesions that are ambiguous in clinical presentation and behavior. Patients with OSCC have a varied etiology, some of which are established while a few of the cases do not elicit classical risk factors. Very often, the dentist is faced with the challenge of making a decision to commence treatment as desired by the patient or pursue further investigation to rule out more potentially morbid diagnosis. Such a cautious stance by the dentist can be possible only if the suspicion index for potentially life-threatening lesions is high on the differential list. Alternatively, these clinical situations necessitate the services of expert opinion that would obviate the chance of missing a diagnosis. A missed diagnosis is a lost opportunity in instituting timely and definitive care for such life-threatening lesions.
Gingival OSCC is more aggressive in behavior and in its early stage bears a resemblance to common mucosal infections. This report reiterates the importance of submitting all gingival biopsies for histopathological examination.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Warnakulasuriya S. Global epidemiology of oral and oropharyngeal cancer. Oral Oncol. 2009;45:309–16. doi: 10.1016/j.oraloncology.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 2.Yoon TY, Bhattacharyya I, Katz J, Towle HJ, Islam MN. Squamous cell carcinoma of the gingiva presenting as localized periodontal disease. Quintessence Int. 2007;38:97–102. [PubMed] [Google Scholar]
- 3.Seoane J, Varela-Centelles PI, Walsh TF, Lopez-Cedrun JL, Vazquez I. Gingival squamous cell carcinoma: Diagnostic delay or rapid invasion? J Periodontol. 2006;77:1229–33. doi: 10.1902/jop.2006.050408. [DOI] [PubMed] [Google Scholar]
- 4.Choi EJ, Zhang X, Kim HJ, Nam W, Cha IH. Prognosis of gingival squamous cell carcinoma diagnosed after invasive procedures. Asian Pac J Cancer Prev. 2011;12:2649–52. [PubMed] [Google Scholar]
- 5.O’sullivan B, Shah J. New TNM staging criteria for head and neck tumors. Semin Surg Oncol. 2003;21:30–42. doi: 10.1002/ssu.10019. [DOI] [PubMed] [Google Scholar]
- 6.Tsantoulis PK, Kastrinakis NG, Tourvas AD, Laskaris G, Gorgoulis VG. Advances in the biology of oral cancer. Oral Oncol. 2007;43:523–34. doi: 10.1016/j.oraloncology.2006.11.010. [DOI] [PubMed] [Google Scholar]
- 7.Saleh A, Kong YH, Vengu N, Badrudeen H, Zain RB, Cheong SC. Dentists’ perception of the role they play in early detection of oral cancer. Asian Pac J Cancer Prev. 2014;15:229–37. doi: 10.7314/apjcp.2014.15.1.229. [DOI] [PubMed] [Google Scholar]
- 8.Vishnudas B, Mahurkar V, Silva ID. Carcinoma of gingiva stimulating epulis – A case report. JIAOMR. 2003;2:49–52. [Google Scholar]
- 9.Neville BW, Damm DD, Allen CM, Bouquot JE. 2nd ed. Philadelphia: Saunders; 2002. Oral and Maxilloacial Pathology. [Google Scholar]
- 10.Kusukawa J, Suefuji Y, Ryu F, Noguchi R, Iwamoto O, Kameyama T. Dissemination of cancer cells into circulation occurs by incisional biopsy of oral squamous cell carcinoma. J Oral Pathol Med. 2000;29:303–7. doi: 10.1034/j.1600-0714.2000.290703.x. [DOI] [PubMed] [Google Scholar]


