Abstract
Calcifying epithelial odontogenic tumor (CEOT) is a locally aggressive, rare benign odontogenic neoplasm that accounts for <1% of all odontogenic tumors. It was first described by a Dutch pathologist Jens Jorgen Pindborg in 1955. It is most often located in the posterior mandible. The tumor usually appears between the second and sixth decade of life and has no gender predilection. It is slow-growing neoplasm with a recurrence rate of 10–15% and with rare malignant transformation. Early diagnosis is essential to avoid oro-maxillofacial deformation and destruction. CEOT is rarely reported in India. We, herewith present a rare case of CEOT with unusual features associated with an impacted right third molar in the posterior mandible of 35 years male, with an emphasis on clinical, radiographic, histopathology and immunohistochemical features.
Keywords: Amyloid, calcifying epithelial odontogenic tumor, driven snow pattern, Liesegang rings, Pindborg tumor
INTRODUCTION
Calcifying epithelial odontogenic tumor (CEOT), also known as a Pindborg tumor, is a locally aggressive, rare benign odontogenic neoplasm of epithelial origin that accounts for <1% of all odontogenic tumors.[1,2,3,4,5] It was first described by a Dutch pathologist Jens Jorgen Pindborg in 1955.[2] He, in 1958, grouped the tumor as a distinct histopathologic entity. Since then, nearly 200 cases of CEOT have been reported in the literature.[3] This tumor is also referred to as adenoid adamintoblastoma by Thoma, unusual ameloblastoma by Tuy and cystic odontoma by Stoppack.[2] The eponym Pindborg tumor was first introduced to the literature in 1963 by Shafer to describe this remarkable and unique odontogenic tumor which typically contains calcifying masses or homogeneous acellular material within the tumor epithelium and stroma.[4] The origin of this tumor is controversial and it is thought to be derived from the oral epithelium, reduced enamel epithelium, stratum intermedium or dental lamina remnants.[3] CEOT presents an extensive diversity in clinical, histopathological features and biological behavior.[6]
This paper illustrates a rare case of CEOT associated with an impacted right third molar in the posterior mandible in a middle-aged man. The clinical, radiological, histological pattern and immunohistochemical investigation with a variety of antibodies are discussed and a brief review of literature is presented.
CASE REPORT
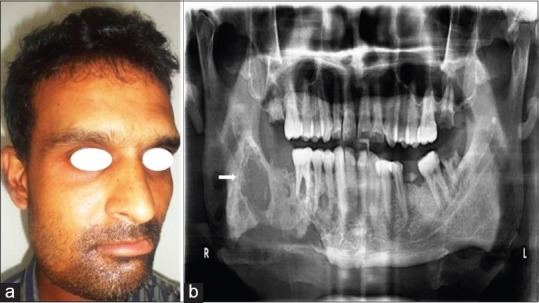
A 35-year-old male reported with a complaint of gradually increasing swelling with a mild intermittent pain on the right lower facial region since 6–7 months [Figure 1a]. The medical history was noncontributory. On extra oral examination, a single, smooth, slightly tender, hard and fixed swelling, measuring 07 cm × 05 cm, involving the complete right mandible was noted. Intraoral examination revealed presence of firm to hard oval shaped tender swelling, extending from mandibular right canine to second molar region, measuring 08 cm × 06 cm, causing extensive bucco-lingual cortical plate expansion but no mobility of teeth. The overlying mucosa of the swelling was intact but erythematous [Figure 1b]. The patient was subjected to various investigations.
Figure 1.

(a) An extra-oral photograph of the patient, having swelling on right side of the face. (b) An intraoral photograph showing lower right buccal vestibule obliteration. (c) Digital panoramic radiograph showing mixed radiolucent-radiopaque lesion involving the body of the mandible. Note the “driven snow” appearance and dislocated third molar
The panoramic radiograph [Figure 1c] revealed a large, well-demarcated mixed radiolucent-radiopaque lesion with a sclerotic border, involving the right mandible, extending from canine anteriorly to the angle of the mandible and mid ramus posteriorly. The lesion presented with scattered to dense areas of calcifications appearing like “driven snow” pattern. Cortical plate expansion and thinning were noted. The second molar was displaced posteriorly whereas the impacted third molar was dislocated to the inferior border of the mandible. The root resorption of right premolars and molars was distinctly observed. The inferior alveolar nerve canal was not traceable.
The axial, coronal and sagittal view of computed tomography (CT) [Figure 2a–c] showed a large expansile well-circumscribed multiple isodense mass and few hypodense areas, involving the right body and ramus of the mandible. The cortical plates were expanded and had erosion on the lingual plate. The contrast enhancement attenuation was observed involving certain areas of the lesion. The multidimensional three-dimensional (3D) reconstruction using soft and hard tissue algorithms demonstrated the size and extent of the lesion [Figure 2d].
Figure 2.

(a) Axial view, (b) coronal view, and (c) sagittal view of computed tomography shows a large expansile well-circumscribed multiple isodense mass and few hypodense areas, involving the right body and ramus of mandible. Note the expansion of bucco-lingual cortical plates and erosion of lingual plate. (d) A 3-D reconstruction image demonstrating the size and extent of the lesion
The incisional biopsy of the lesion demonstrated the features of CEOT. Surgical enucleation along with curettage was carried out under general anesthesia [Figure 3a]. The excised specimen [Figure 3b] was subjected to radiography which showed scattered to dense areas of calcifications, extracted second molar tooth and an embedded third molar tooth in the mass [Figure 3c]. The histopathological examination [Figure 4a and b] revealed an epithelial odontogenic neoplasm composed of sheets of polyhedral epithelial cells with an abundant eosinophilic, granular cytoplasm. Also, nuclear polymorphism and intercellular bridges were noted. The extra-cellular amyloid-like substance and calcified concentric deposits called Liesegang rings were also identified. The eosinophilic amyloid material was stained positive for Congo red and appeared as an apple-green birefringence under polarized light [Figure 4c]. On immunohistochemical evaluation, the cocktail of cytokeratin 1, 5, 6, 13, 16, AE1 and AE3 was positive for the epithelial nature of tumor cells [Figure 5a]. The Ki-67 showed low proliferation activity of tumor cells suggestive of the benign condition [Figure 5b].
Figure 3.

(a) Surgical procedure. (b) Excised specimen with a mandibular second molar. (c) Reveals a radiographic image of an excised specimen showing scattered to dense areas of calcifications, second molar tooth and an embedded third molar tooth in the mass
Figure 4.

(a and b) Histopathological photomicrographs showing an epithelial odontogenic neoplasm composed of sheets of polyhedral epithelial cells (black arrow in fig 4a) with an abundant eosinophilic, granular cytoplasm, nuclear polymorphism and intercellular bridges. The extra-cellular amyloid-like substance (black arrow in fig 4b) and calcified concentric deposits are seen distinctly (H&E stain, a: x40, b: x200). (c) The eosinophilic amyloid material shows positive staining for Congo red and an apple-green birefringence appearance under polarized light (Congo red stain, x40)
Figure 5.

Immunohistochemical evaluation. (a) Positive immunoreactivity to a cocktail of cytokeratin 1, 5, 6, 13, 16, AE1 and AE3 (black arrow) for the epithelial nature of tumor cells (IHC stain, x100). (b) ki-67 showing low proliferation activity of tumor cells suggestive of benign condition (IHC stain, x100)
Based on all the above findings, the final diagnosis of intra osseous CEOT was made. Patient is on regular follow up from last 6 months and no recurrence is reported [Figure 6a and b].
Figure 6.
(a) Post treatment 6 months follow up clinical photograph. (b) Panoramic radiograph taken during 6 months followup
DISCUSSION
According to WHO classification of 1992, CEOT is a “locally invasive epithelial neoplasm characterized by the development of intra-epithelial structures, probably of an amyloid-like nature, which may be calcified and which may be liberated as the cells breakdown.”[2,5,6] CEOT may present as an intra osseous (central) or extra osseous (peripheral) tumor. The intra osseous tumor is the most common type, usually seen in the posterior mandible, is more aggressive and accounts for more than 95% of the cases. Whereas the extra osseous tumor accounts for <6% and most commonly occurs on anterior gingiva as a sessile mass capable of destroying the underlying bone. The histological features are similar for both the types.[1,2,7]
CEOT usually appears between the second and sixth decade of life but mainly occurs in the fourth decade and has no gender predilection. It is most often located in the premolar-molar region of the mandible and associated mostly with one or more impacted tooth.[2,7,8] Kaplan et al. reported that the most prevalent impacted tooth were molars (62%) followed by premolars, canines, incisors and the least were the supernumerary or unidentified teeth (4%).[8] This article describes the unusual intra osseous tumor involving canine to the molar region with an impacted third molar, in a mid-30 aged male. Although CEOT is slow growing, it is locally invasive with a recurrence rate of 10–15% and with rare malignant transformation.[6,7,8,9] Various literatures have reported that intra osseous CEOT may manifest as asymptomatic swelling and grows by infiltration, causing cortical plate expansion, tooth movement and root resorption.[4,10,11,12,13] The present case also exhibited these features. Rarely, the tumor may be associated with paresthesia.[2,3] However, the present case reported with a swelling and mild intermittent pain that may be due to a large extension, associated infection and compression of the inferior alveolar nerve. CEOT when located in the maxilla, may present with nasal stuffiness, epistaxis and headache.[5] Although CEOT is a benign neoplasm, its biologic behavior is variable, ranging from very mild to moderately invasive behaviour.[5,10,14] However, in most cases, there is little information on tumor duration and hence the true growth rate of the tumor is questionable.[2,11]
The radiographic appearance of CEOT is variable and depends on the stage of development; either as well-defined radiolucency, mixed radiolucent-radiopaque or completely radioopaque mass. It also concurrently erodes bone and thus, the lesion often appears as mixed radiolucent-radiopaque mass with many small irregular trabeculae traversing the radiolucent area giving a characteristic “driven snow” appearance on the radiograph due to scattered flecks of calcification.[1,2,5,10,15] The present case seems to support this appearance. The tumor most commonly appears as either a diffuse or a well-circumscribed unilocular radiolucent area. In some cases, the lesion becomes multilocular with a honeycomb pattern.[9,10,12,15] The margins may be well defined or sclerotic and vague. The tumor may be associated with an impacted tooth, which is often obscured by tumor-associated calcification. Similar finding was distinctly seen in our case. Although root resorption is an unusual finding, it was evident in molar teeth of the present case and was in accordance with the studies of Kaplan et al. and Tanimoto et al.[8,10] The root resorption and displacement of teeth may occur due to the pressure exerted by the growing tumor. McGowan and Browne in 1982 found that the presence of calcification is approximately double on microscopic examination when compared to radiographic analysis.[11]
On CT, CEOT may appear as an expansile, unilocular or multilocular lesion containing radioopaque areas within the jaw. The multiplanar CT images and 3D reconstruction are helpful in delineating the extent of the lesion and visualization of the internal structure, which is essential for clinical diagnosis and treatment planning. CT imaging will streamline the process of interpretation, but the final diagnosis of CEOT is based on histological examination.[2,5,10,12,15]
The histologic pattern of CEOT is typical and well defined. The tumor consists of polyhedral cells arranged in masses, sheets, islands, cords, rows or strands in a scanty connective tissue stroma.[5,12] The cells are pleomorphic with well-defined borders, prominent nucleoli and abundant finely granular cytoplasm filled with an eosinophilic “ amyloid-like” material, which gradually becomes concentric calcified deposits, resembling psammoma bodies called the “Liesegang rings,” which is considered as pathognomonic for this tumor. The round shaped eosinophilic amyloid material will stain positive for Congo red and will appear as an apple-green birefringence under a polarized microscope.[2,5,12,14] All these features did exist in the reported case. Due to the similarity of cellular pattern with various lesions, immunohistochemistry shall be performed to differentiate CEOT from other benign odontogenic tumor (esp. ameloblastoma), minor salivary gland tumor and oral squamous carcinoma.[14]
The differential diagnosis of CEOT will depend on radiographic appearance. In case of radiolucent lesion- dentigerous cyst, odontogenic keratocyst, ameloblastoma, odontogenic myxoma; whereas in mixed radiolucent radiopaque lesion- Calcifying odontogenic cyst, adenomatoid odontogenic tumor, complex odontoma, ameloblastic fibro-odontoma, fibro-osseous lesions, osteoblastoma should be considered.[2,3,15]
The treatment methods can range from simple enucleation or curettage to hemi-mandibulectomy or hemi-maxillectomy.[2,5,9,12] Enucleation with a margin of normal tissue is usually recommended for mandibular lesions. CEOT of the maxilla should be treated more aggressively as maxillary tumors grow more rapidly and are usually not well confined. Treatment, however, should be individualized for each case.[2,5] Our patient underwent enucleation and no recurrence is reported in 6 months of follow-up. Long-term follow-up, at least 5 years, is a must as there is high risk of recurrence if the tumor was incompletely resected, especially with clear cell variant, which is locally more aggressive. The recurrence rate may range from 14% to 20%. The malignant behavior is extremely rare.[2,5,12,14]
CONCLUSION
CEOT is a rare odontogenic tumor and does not have a pathognomonic clinical or radiographic presentation, thereby causing a diagnostic challenge. The classic histopathologic pattern will always confirm the diagnosis. A comprehensive immunohistochemical study will help in understanding the exact nature of the tumor. However, till date, the pathogenesis is obscure and needs further research.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kaushal S, Mathur SR, Vijay M, Rustagi A. Calcifying epithelial odontogenic tumor (Pindborg tumor) without calcification: A rare entity. J Oral Maxillofac Pathol. 2012;16:110–2. doi: 10.4103/0973-029X.92985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lim I, Mallari R, Lacsamana N, Paz D, Villafuerte A. Recurrent calcifying epithelial odontogenic tumor (Pindborg tumor): A case study. Oral Oncol Extra. 2005;41:259–66. [Google Scholar]
- 3.Deboni MC, Naclério-Homem Mda G, Pinto Junior DS, Traina AA, Cavalcanti MG. Clinical, radiological and histological features of calcifying epithelial odontogenic tumor: Case report. Braz Dent J. 2006;17:171–4. doi: 10.1590/s0103-64402006000200017. [DOI] [PubMed] [Google Scholar]
- 4.Misra SR, Lenka S, Sahoo SR, Mishra S. Giant Pindborg tumor (calcifying epithelial odontogenic tumor): An unusual case report with radiologic-pathologic correlation. J Clin Imaging Sci. 2013;3(Suppl 1):11. doi: 10.4103/2156-7514.124056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vinod V, Venkateswarlu M, Reddy G. Pindborg tumor: Review of literature and case reports. J Indian Acad Oral Med Radiol. 2011;23:660–3. [Google Scholar]
- 6.Malik S, Alam M, Shahina M, Siddique S, Prabhu V. Calcifying epithelial odontogenic tumor. Bangladesh J Med Sci. 2014;13:14–9. [Google Scholar]
- 7.Müller D, Manojlovic S, Luksic I, Grgurevic J. Calcifying epithelial odontogenic tumor of the maxilla (Pindborg tumor) Coll Antropol. 2012;36(Suppl 2):205–8. [PubMed] [Google Scholar]
- 8.Kaplan I, Buchner A, Calderon S, Kaffe I. Radiological and clinical features of calcifying epithelial odontogenic tumour. Dentomaxillofac Radiol. 2001;30:22–8. doi: 10.1038/sj/dmfr/4600566. [DOI] [PubMed] [Google Scholar]
- 9.Dabir A, Padhye M. Calcifying epithelial odontogenic tumor - A case report (Pindborg's tumor) Sci J. 2008;2:1–4. [Google Scholar]
- 10.Tanimoto K, Tomita S, Aoyama M, Furuki Y, Fujita M, Wada T. Radiographic characteristics of the calcifying odontogenic cyst. Int J Oral Maxillofac Surg. 1988;17:29–32. doi: 10.1016/s0901-5027(88)80225-x. [DOI] [PubMed] [Google Scholar]
- 11.McGowan RH, Browne RM. The calcifying odontogenic cyst: A problem of preoperative diagnosis. Br J Oral Surg. 1982;20:203–12. doi: 10.1016/s0007-117x(82)80040-1. [DOI] [PubMed] [Google Scholar]
- 12.Neville B, Damm D, Allen C, Bouquot J. 3rd ed. Philadelphia: W.B Saunders; 2008. Oral and Maxillofacial Pathology; pp. 716–8. [Google Scholar]
- 13.Sahni P, Nayak MT, Singhvi A, Sharma J. Clear cell calcifying epithelial odontogenic (Pindborg) tumor involving the maxillary sinus: A case report and review of literature. J Oral Maxillofac Pathol. 2012;16:454–9. doi: 10.4103/0973-029X.102520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lin J, Bianchi M, Popnikolov NK, Abaza NA. Calcifying epithelial odontogenic tumor: Case report with immunohistochemical and ultrastructural study and review of the literature. J Oral Maxillofac Surg. 2013;71:278–89. doi: 10.1016/j.joms.2012.06.171. [DOI] [PubMed] [Google Scholar]
- 15.Wood N, Goaz P. 5th ed. St. Louis: Mosby Yearbook; 1997. Differential Diagnosis of Oral and Maxillofacial Lesions; pp. 428–31. [Google Scholar]


