Abstract
AIM: To evaluate the clinical value of various imageological methods in diagnosing the pancreato-biliary diseases and to seek the optimal procedure.
METHODS: Eighty-two cases of pancreato-biliary diseases confirmed by surgery and pathology were analyzed. There were 38 cases of cholelithiasis, 34 cases of pancreato-biliary tumors and 10 other cases. The imageological methods included B-US, CT, ERCP, PTC, cross-sectional MRI and MR cholangiopancreatography (MRCP).
RESULTS: The accuracy rate of MRCP in detecting the location of pancreato-biliary obstruction was 100%. In differentiating malignant from benign obstruction, the sensitivity of the combination of MRCP and cross-sectional MRI was 82.3%, the specificity was 93.8%, and the accuracy rate was 89.0%. The accuracy rate for determining the nature of obstruction was 87.8%, which was superior to that of B-US (P = 0.0000) and CT (P = 0.0330), but there was no significant difference between direct cholangiopancreatography and the combination of MRCP and conventional MRI (P = 0.6666).
CONCLUSION: In most cases, MRCP can substitute direct cholangiopancreatography for diagnosis. The combination of MRCP and cross-sectional MRI should be considered as an important means in diagnosing the pancreato-biliary diseases, pre-operative assessment and post-operative follow-ups.
INTRODUCTION
Pancreato-biliary disorders are common diseases that often involve the biliary system to produce the symptom of obstructive jaundice. It is the precondition to investigate the obstructive location and causes of pancreato-biliary diseases. In this study, 82 cases of pancreato-biliary diseases confirmed by surgery and pathology were analyzed. The aims of the prospective study were to evaluate the clinical value of various imageological methods in diagnosing the pancreato-biliary diseases and to seek the optimal examination procedure.
MATERIALS AND METHODS
Patients
The study subjects included 82 patients (54 men and 28 women, mean age 60.0 years, range 11-82 years), 67 (81.7%) cases had the symptom of obstructive jaundice. All patients underwent B-US, MR cholangiopancreatography (MRCP) and cross-sectional MRI examination. Fifty-seven patients underwent enhanced or un-enhanced CT scan. In addition, 48 patients had undergone direct cholangiopancreatography (41 ERCP and 7 PTC). However, direct cholangiopancreatography was unsuccessful in 4 cases due to difficult cannulation (2 ERCP), post-gastroenterostomy (1 ERCP) and sick patient (1 PTC). ERCP was incomplete in another 4 cases because only the pancreatic duct could be demonstrated and the biliary tree was not opacified. Therefore, 40 direct cholangiopancreatographies (34 ERCP and 6 PTC) were performed in all 82 cases, 1 patient had complication of acute pancreatitis after ERCP. All patients with pancreat-biliary diseases were confirmed by surgical findings and pathology, including 12 by laparoscopic cholecystectomy (LC), 6 by endoscopic sphincter tenotomy (EST) and 1 by PTC drainage (PTCD). Among the 82 cases, 38 were diagnosed as cholelithiasis, 34 as pancreato-biliary tumors and 10 as other diseases (Table 1).
Table 1.
Pancreato-biliary diseases (n = 82)
| Pancreato-biliary diseases | No. of cases |
| Cholelithiasisa | 38 |
| Gallbladder stone | 14 |
| Intrahepatic bile duct stone | 7 |
| Choledocholithiasis | 17 |
| Pancreato-biliary tumorb | 34 |
| Gallbladder carcinoma | 6 |
| Cholangiocarcinoma | 9 |
| Ampullary carcinoma | 3 |
| Pancreatic head carcinoma | 11 |
| Bile papilla carcinoma | 5 |
| Other diseases | 10 |
| Bile duct injury | 2 |
| Choledochal cyst | 2 |
| Sclerosing cholangitis | 2 |
| Chronic pancreatitis | 4 |
Gallbladder stone mixed with intra-or extra-hepatic stone 15, Mirizzi syndrome 2;
Hepatic invasion or metastasis 5, lymphadenectasis 3.
Techniques
MR imaging was performed with a 1.0T superconductive unit (Philips Gyroscan T10-NT, software version 4.6.2) containing a body coil. The patients were examined in the supine position, quiet breathing and abdominal band compression. The routine upper abdominal axial T1WI, T2WI and coronal T2WI MR examinations with Turbo Spin-Echo (TSE) sequence were performed first, and followed by the additional axial T2WI and/or T1WI fat-suppressed sequence (spectral saturation inversion recovery, SPIR). The routine axial images served as guides to locate the MR cholangiopancreatography (MRCP). MRCP was performed with coronal, multislices, heavily T2-weighted TSE sequence (TR = 2000 ms, TE = 700 ms). A non-breath-hold, respiratory-triggering technique was used to decrease the respiratory motion artifact. The MRCP source images were three-dimensionally (3D) reconstructed using a maximum-intensity-projection (MIP) algorithm. The total imaging time was approximately 30 min.
Computed tomography (CT) used a whole body CT scan unit (Picker PQ-2000). All CT examinations were performed after the patients had fasted for 4-8 hours and took 500-1000 ml oral contrast (0.5%-1% Meglumine Diatrizoate) before CT scanning. Enhanced CT examination used 80-100 ml non-ion intravenous contrast agents injected through anecubital vein in a bolus at the rate of 2-3 ml/s.
Direct cholangiopancreatography (ERCP and PTC) was performed with a digital imaging unit (Philips Diagnost 93).
Imaging analysis
All image data of 82 cases were carefully reviewed to observe the enlargement or stricture of pancreato-biliary tract. The study protocol included detecting the obstructive locations, distinguishing the malignant from benign causes and evaluating the clinical value of various imaging methods (including B-US, CT, MRCP, ERCP/PTC) in diagnosing the pancreato-biliary diseases. SAS software was used for all statistical analyses.
The diagnostic principles and evaluating criteria for direct cholangiopancreatography and MRCP were identical, but in MRCP it was more important to carefully review both the source images and the MIP reconstructed images. According to the findings of the dilatation or stricture of pancreato-biliary tree and gallbladder, the obstructive locations of pancreato-biliary duct were divided into three parts: intra-hepatic or extra-hepatic bile duct and main pancreatic duct. Normal gallbladder was 7-10 cm in length and 3-4 cm in width. Dilatation of the common bile duct was defined as larger than 8 mm in maximal diameter in patients without histories of cholecystectomy and 10 mm in patients with prior cholecystectomy. Dilatation of the intra-hepatic bile duct and main pancreatic duct was defined as larger than 3 mm in maximal diameter[1-4].
The cause of pancreato-biliary abnormality was evaluated using a five-point scale to assign a confidence level: 1. definitely benign, 2. probably benign, 3. indeterminate, 4. probably malignant, and 5. definitely malignant[5]. If the cause of pancreato-biliary abnormality was assumed to be malignant, the reasons were chosen from the following findings: visualization of tumor, double duct sign, abrupt obstruction of bile duct, irregularity of obstructed margin, or asymmetric obstruction of the distal margin of the dilated bile duct. Receiver operating characteristic (ROC) curve analysis was performed to compare the results of readings of MRCP images versus the results of readings of the combination of MRCP images and routine MR images and versus the results of readings of ERCP images. Binormal ROC curves were fitted using ROCKIT 0.9B software. The diagnostic capability was determined by calculating the area under the ROC curve (Az). Ratings of 1 or 2 indicated a reading of a benign lesion, ratings of 4 or 5 indicated a rating of a malignant lesion. Ratings of 3 were considered to indicate an indeterminate diagnosis. Sensitivity, specificity and accuracy of ERCP, MRCP and the combination of MRCP and routine MR imaging in differentiating malignant from benign causes of pancreato-biliary tract obstruction were calculated.
RESULTS
MRCP image quality
MR cholangiopancreatography was successfully performed in all 82 patients and the images of MRCP were similar to those of direct cholangiopancreatography. MRCP studies of diagnostic quality were obtained in 79 (96.3%) subjects with fine contrast between the pancreato-biliary structure and the surrounding background. In the remaining 3 patients with pancreato-biliary tumor, the presence of ascitic fluid in the upper abdomen and the fluid-containing organs due to gastrointestinal obstruction obscured visualization of the pancreato-biliary tree and degraded the quality of the MRCP image. In 8 (16.7%) patients in whom direct cholangiopancreatography was unsuccessful or incomplete, MRCP examinations all succeeded and the MRCP images were satisfactory.
Diagnosis of obstructive location
Among the 82 patients with pancreato-biliary diseases, 8, 60 and 21 cases had pancreato-biliary obstructive locations in intra-hepatic, extra-hepatic bile duct and main pancreatic duct, respectively (totally 89 locations). MRCP could clearly visualize the dilation of pancreato-biliary ducts above the obstructive level in their native state, thus being more suitable for demonstrating the extra-hepatic bile duct obstruction. The total accuracy of MRCP in detecting the location of pancreato-biliary obstruction was 100%, which was superior to that of B-US (P = 0.0002) and CT (P = 0.0422), but there was no sign ifican t d ifference b etween MRCP an d d irect cholangiopancreatography (P = 0.1487) (Table 2).
Table 2.
Accuracy of pancreato-biliary obstruction level (%) by different imageological methods
| Level | Intra-hepatic | Extra-hepatic | Main pancreatic | Total |
| B-US | 100.0 (8/8) | 81.7 (49/60) | 90.5 (19/21) | 85.4 (76/89) |
| CT | 100.0 (4/4) | 93.0 (40/43) | 100.0 (19/19) | 95.5 (63/66) |
| ERCP/PTC | 100.0 (5/5) | 96.7 (29/30) | 100.0 (8/8) | 97.7 (42/43) |
| MRCP | 100.0 (8/8) | 100.0 (60/60) | 100.0 (21/21) | 100.0 (89/89) |
Differentiation of malignant from benign obstruction
The sensitivity, specificity and accuracy of MRCP in distinguishing malignant from benign causes of pancreato-biliary obstruction were 64.7%, 81.2% and 74.4%, respectively, while those of ERCP/PTC were 77.8%, 86.4% and 82.5%, respectively. The difference was not significant between MRCP and ERCP/PTC in Az area under the ROC curve (P = 0.4590). The combination of MRCP and routine MR imaging could obviously improve the diagnostic capability of differentiating the causes of pancreato-biliary obstruction with a sensitivity of 82.3%, a specificity of 93.8% and an accuracy of 89.0%. The difference was significant between MRCP and the combination of MRCP and routine MR imaging (P = 0.0489) (Table 3 and Figure 1).
Table 3.
ROC analysis of pancreato-biliary obstruction
| ERCP/PTC (n = 40) | MRCP (n = 82) | MRCP + MRI (n = 82) | |
| True-positive | 14 | 22 | 28 |
| True-negative | 19 | 39 | 45 |
| False-positive | 3 | 9 | 3 |
| False-negative | 4 | 12 | 6 |
| Sensitivity (%) | 77.8 | 64.7 | 82.3 |
| Specificity (%) | 86.4 | 81.2 | 93.8 |
| Accuracy (%) | 82.5 | 74.4 | 89.0 |
| AZ Values ± SD | 0.9281 ± 0.0455 | 0.8833 ± 0.0400 | 0.9687 ± 0.0168 |
Figure 1.
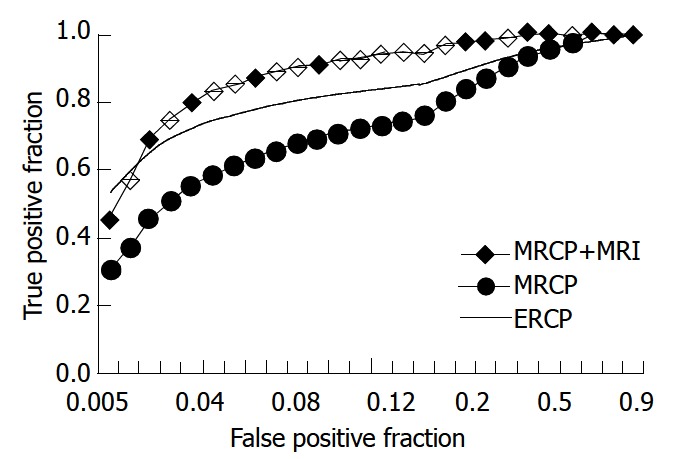
ROC curve analysis of differentiation between ma-lignant and benign causes of pancreato-biliary obstruction.
Diagnosis of obstructive causes
The total accuracy of MRCP in diagnosing the causes of pancreato-biliary obstruction was 75.6%, which was similar to that of direct cholangiopancreatography (ERCP/PTC) (P = 0.2345) and CT (P = 0.7970), but superior to that of B-US (P = 0.0131). The combination of MRCP and routine MR imaging significantly improved the clinical diagnostic ability with an accuracy of 87.8%, which was superior to that of CT (P = 0.0330) and US (P = 0.0000).
The diagnostic rate by the combination of MRCP and routine MR imaging was 92.1% and 94.1%, for cholelithasis and choledocholithiasis respectively, which was superior to that of CT (P = 0.0428) and US (P = 0.0049). But the difference between ERCP/PTC and the combined MRCP and routine MR imaging was not significant (P = 0.6445). The accuracy of CT, ERCP/PTC, MRCP and the combined MRCP and routine MR imaging in distinguishing the various pancreato-biliary tumors was significantly higher than that of US (P = 0.0002) (Table 4).
Table 4.
Accuracy of diagnosis of obstructive causes (%)
| B-US | CT | ERCP/PTC | MRCP | MRCP+MRI | |
| Cholelithiasis | |||||
| Gallbladder stone | 71.4 | 75.0 | 80.0 | 78.5 | 92.9 |
| Intrahepatic bile duct stone | 85.7 | 100.0 | 100.0 | 71.4 | 85.7 |
| Choledocholithiasis | 52.9 | 63.6 | 87.5 | 88.2 | 94.1 |
| Pancreato-biliary tumor | |||||
| Gallbladder carcinoma | 50.0 | 75.0 | 60.0 | 50.0 | 66.7 |
| Cholangiocarcinoma | 33.3 | 75.0 | 83.3 | 77.8 | 88.9 |
| Ampullary carcinoma | 33.3 | 50.0 | 100.0 | 66.7 | 66.7 |
| Pancreatic head carcinoma | 63.6 | 81.8 | 100.0 | 90.9 | 100.0 |
| Bile papilla carcinoma | 40.0 | 66.7 | 100.0 | 60.0 | 80.0 |
| Other diseases | |||||
| Bile duct injury | 50.0 | 100.0 | 100.0 | 100.0 | |
| Choledochal cyst | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Sclerosing cholangitis | 0 | 50.0 | 0 | 0 | 50.0 |
| Chronic pancreatitis | 75.0 | 75.0 | 100.0 | 50.0 | 75.0 |
| Total | 57.3 | 73.7 | 85.0 | 75.6 | 87.8 |
DISCUSSION
US or CT examination (including endoscopic US and spiral CT) has been the first choice in diagnosing the pancreato-biliary diseases[6-9]. Direct cholangiopancreatography obtained through ERCP or PTC has served as “golden standard” in pancreato-biliary imageology.
Magnetic resonance cholangiopancreatography (MRCP), advocated by German researcher Wallner BK and his group in 1991[10], has offered a new imaging modality for diagnosing pancreato-biliary system disorders[10-15]. In the present study, MRCP was successfully performed in all 82 patients and the images of MRCP were similar to those of direct cholangiopancreatography. MRCP studies of diagnostic quality were obtained in 79 cases (96.3%), including 8 (16.7%) in which direct cholangiopancreatography were unsuccessful or incomplete. Therefore, MRCP might provide an efficient alternative to direct cholangiopancreatography when diagnostic ERCP and PTC were unsuccessful or inadequate[1,16].
In our study, the accuracy of MRCP in detecting the location of pancreato-biliary obstruction was 100%, which was superior to that of B-US and CT, but was not significantly different between MRCP and direct cholangiopancreatography. Compared with ERCP/PTC examination, the noninvasive MRCP could exhibit the whole pancreato-biliary duct system and demonstrate the level, degree and range of obstruction as well as morphological characteristics. In addition, MRCP could provide a plenty of valuable imageological information and help determine the best approach for palliative drainage and other interventional treatment for the patients with unresectable tumors[17,18].
In pancreato-biliary system imageology, it is very important in diagnosing and differentiating malignant from benign causes of pancreato-biliary obstruction. The combined MRCP and routine MR imaging could significantly improve the clinical diagnostic capability by exhibiting the pathological changes of the surrounding structures[19-22]. For pancreato-biliary tumors, MRCP could define the location and morphological characteristics of pancreato-biliary obstruction, and evaluate the range of tumors involvement and the surgical resectability. Furthermore, with the advantages of both CT and direct cholangiopancreatography examination, the combined routine MR imaging and MRCP might exhibit the pertinent surrounding structures and raise the clinical diagnostic accuracy[17,23,24].
US and CT techniques are most frequently used in the initial evaluation of patients with cholelithiasis and both have a high accuracy in diagnosing gallbladder and intrahepatic duct stones. The sensitivity of MRCP in diagnosing gallbladder and intrahepatic duct stones varied with the size, number and location of the stones and MRCP being more suitable for the diagnosis of choledocholithiasis. In summary, the MRCP could mainly detect the stones in common bile duct and exclude other pancreato-biliary obstructive diseases[25-27].
With the development of laparoscopic technique, laparoscopic cholecystectomy (LC) and endoscopic sphincter tenotomy (EST) have been widely used in the biliary surgery[28]. MRCP can depict the whole anatomic structure of biliary tree and help guarantee the success of laparoscopic cholecystectomy. Before surgical dissection, to identify the anatomic variants of the biliary tree with MRCP could result in a decreased risk of bile duct injury during laparoscopic cholecystectomy[29]. Now, ERCP is no longer the routine examination in patients with choledocholithiasis, and endoscopic sphincter tenotomy is chiefly used instead to remove stones in common bile duct.
As to the benign strictures, due to cholangitis, surgical injury or chronic pancreatitis, MRCP may have some difficulties in showing the mini-changes of pancreato-biliary duct. But the use of dynamic MRCP with secretin stimulation might be useful for diagnosing pancreatic papillary stenosis or dysfunction and for detecting reduced pancreatic exocrine reserve[30-32]. In addition, the literature indicates that MRCP could be used initially in evaluating choledochal cyst[33].
In conclusion, in recent optimal imageological procedures of diagnosing the pancreato-biliary diseases, B-US is still the first choice for evaluation. The combination of MRCP and routine MR imaging provides an efficient method to diagnose various pancreato-biliary obstructions, differentiate malignant from benign causes and carry out post-operative follow-ups. Cross-sectional MR imaging and CT are complementary modalities for pre-operative diagnosis and assessment of pancreato-biliary tumors. Direct diagnostic cholangiopancreatography (ERCP/PTC) is chiefly used for difficult cases and combined with other interventional treatment, including EST or PTCD (Figure 2).
Figure 2.
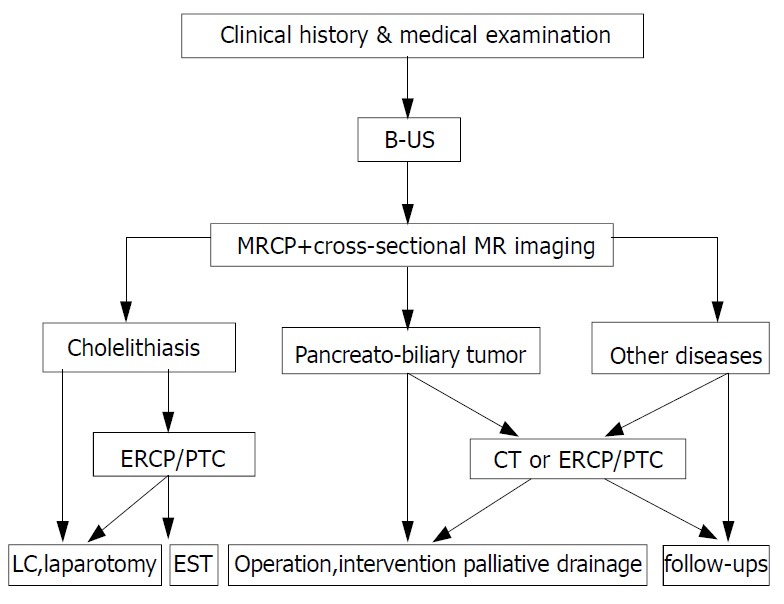
Optimal imageological examination procedure of pancreato-biliary diseases.
Footnotes
Edited by Ma JY
References
- 1.Soto JA, Yucel EK, Barish MA, Chuttani R, Ferrucci JT. MR cholangiopancreatography after unsuccessful or incomplete ERCP. Radiology. 1996;199:91–98. doi: 10.1148/radiology.199.1.8633178. [DOI] [PubMed] [Google Scholar]
- 2.Guibaud L, Bret PM, Reinhold C, Atri M, Barkun AN. Bile duct obstruction and choledocholithiasis: diagnosis with MR cholangiography. Radiology. 1995;197:109–115. doi: 10.1148/radiology.197.1.7568807. [DOI] [PubMed] [Google Scholar]
- 3.Reinhold C, Bret PM. Current status of MR cholangiopancreatography. AJR Am J Roentgenol. 1996;166:1285–1295. doi: 10.2214/ajr.166.6.8633434. [DOI] [PubMed] [Google Scholar]
- 4.Barish MA, Soto JA. MR cholangiopancreatography: techniques and clinical applications. AJR Am J Roentgenol. 1997;169:1295–1303. doi: 10.2214/ajr.169.5.9353445. [DOI] [PubMed] [Google Scholar]
- 5.Irie H, Honda H, Tajima T, Kuroiwa T, Yoshimitsu K, Makisumi K, Masuda K. Optimal MR cholangiopancreatographic sequence and its clinical application. Radiology. 1998;206:379–387. doi: 10.1148/radiology.206.2.9457189. [DOI] [PubMed] [Google Scholar]
- 6.Kanemaki N, Nakazawa S, Inui K, Yoshino J, Yamao J, Okushima K. Three-dimensional intraductal ultrasonography: preliminary results of a new technique for the diagnosis of diseases of the pancreatobiliary system. Endoscopy. 1997;29:726–731. doi: 10.1055/s-2007-1004297. [DOI] [PubMed] [Google Scholar]
- 7.de Lédinghen V, Lecesne R, Raymond JM, Gense V, Amouretti M, Drouillard J, Couzigou P, Silvain C. Diagnosis of choledocholithiasis: EUS or magnetic resonance cholangiography A prospective controlled study. Gastrointest Endosc. 1999;49:26–31. doi: 10.1016/s0016-5107(99)70441-4. [DOI] [PubMed] [Google Scholar]
- 8.Zeman RK, Fox SH, Silverman PM, Davros WJ, Carter LM, Griego D, Weltman DI, Ascher SM, Cooper CJ. Helical (spiral) CT of the abdomen. AJR Am J Roentgenol. 1993;160:719–725. doi: 10.2214/ajr.160.4.8456652. [DOI] [PubMed] [Google Scholar]
- 9.Stockberger SM, Sherman S, Kopecky KK. Helical CT cholangiography. Abdom Imaging. 1996;21:98–104. doi: 10.1007/s002619900024. [DOI] [PubMed] [Google Scholar]
- 10.Wallner BK, Schumacher KA, Weidenmaier W, Friedrich JM. Dilated biliary tract: evaluation with MR cholangiography with a T2-weighted contrast-enhanced fast sequence. Radiology. 1991;181:805–808. doi: 10.1148/radiology.181.3.1947101. [DOI] [PubMed] [Google Scholar]
- 11.Takehara Y. Fast MR imaging for evaluating the pancreaticobiliary system. Eur J Radiol. 1999;29:211–232. doi: 10.1016/s0720-048x(98)00177-6. [DOI] [PubMed] [Google Scholar]
- 12.Jara H, Barish MA, Yucel EK, Melhem ER, Hussain S, Ferrucci JT. MR hydrography: theory and practice of static fluid imaging. AJR Am J Roentgenol. 1998;170:873–882. doi: 10.2214/ajr.170.4.9530026. [DOI] [PubMed] [Google Scholar]
- 13.Hirohashi S, Hirohashi R, Uchida H, Kitano S, Ono W, Ohishi H, Nakanishi S. MR cholangiopancreatography and MR urography: improved enhancement with a negative oral contrast agent. Radiology. 1997;203:281–285. doi: 10.1148/radiology.203.1.9122408. [DOI] [PubMed] [Google Scholar]
- 14.Papanikolaou N, Karantanas A, Maris T, Gourtsoyiannis N. MR cholangiopancreatography before and after oral blueberry juice administration. J Comput Assist Tomogr. 2000;24:229–234. doi: 10.1097/00004728-200003000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Fulcher AS, Turner MA. MR cholangiopancreatography. Radiol Clin North Am. 2002;40:1363–1376. doi: 10.1016/s0033-8389(02)00046-5. [DOI] [PubMed] [Google Scholar]
- 16.Owens GR, Shutz SM. Value of magnetic-resonance cholangiopancreatography (MRCP) after unsuccessful endoscopic-retrograde cholangiopancreatography (ERCP) Gastrointest Endosc. 1999;49:265–266. [PubMed] [Google Scholar]
- 17.Bret PM, Reinhold C. Magnetic resonance cholangiopancreatography. Endoscopy. 1997;29:472–486. doi: 10.1055/s-2007-1004252. [DOI] [PubMed] [Google Scholar]
- 18.Macaulay SE, Schulte SJ, Sekijima JH, Obregon RG, Simon HE, Rohrmann CA, Freeny PC, Schmiedl UP. Evaluation of a non-breath-hold MR cholangiography technique. Radiology. 1995;196:227–232. doi: 10.1148/radiology.196.1.7784572. [DOI] [PubMed] [Google Scholar]
- 19.Boraschi P, Braccini G, Gigoni R, Geloni M, Perri G. MR cholangiopancreatography: value of axial and coronal fast Spin-Echo fat-suppressed T2-weighted sequences. Eur J Radiol. 1999;32:171–181. doi: 10.1016/s0720-048x(99)00002-9. [DOI] [PubMed] [Google Scholar]
- 20.Lee MG, Lee HJ, Kim MH, Kang EM, Kim YH, Lee SG, Kim PN, Ha HK, Auh YH. Extrahepatic biliary diseases: 3D MR cholangiopancreatography compared with endoscopic retrograde cholangiopancreatography. Radiology. 1997;202:663–669. doi: 10.1148/radiology.202.3.9051013. [DOI] [PubMed] [Google Scholar]
- 21.Kim MJ, Mitchell DG, Ito K, Outwater EK. Biliary dilatation: differentiation of benign from malignant causes--value of adding conventional MR imaging to MR cholangiopancreatography. Radiology. 2000;214:173–181. doi: 10.1148/radiology.214.1.r00ja35173. [DOI] [PubMed] [Google Scholar]
- 22.Qin LX, Tang ZY. Hepatocellular carcinoma with obstructive jaundice: diagnosis, treatment and prognosis. World J Gastroenterol. 2003;9:385–391. doi: 10.3748/wjg.v9.i3.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pavone P, Laghi A, Catalano C, Panebianco V, Fabiano S, Passariello R. MRI of the biliary and pancreatic ducts. Eur Radiol. 1999;9:1513–1522. doi: 10.1007/s003300050877. [DOI] [PubMed] [Google Scholar]
- 24.Pavone P, Laghi A, Passariello R. MR cholangiopancreatography in malignant biliary obstruction. Semin Ultrasound CT MR. 1999;20:317–323. doi: 10.1016/s0887-2171(99)90063-x. [DOI] [PubMed] [Google Scholar]
- 25.Varghese JC, Liddell RP, Farrell MA, Murray FE, Osborne DH, Lee MJ. Diagnostic accuracy of magnetic resonance cholangiopancreatography and ultrasound compared with direct cholangiography in the detection of choledocholithiasis. Clin Radiol. 2000;55:25–35. doi: 10.1053/crad.1999.0319. [DOI] [PubMed] [Google Scholar]
- 26.Boraschi P, Neri E, Braccini G, Gigoni R, Caramella D, Perri G, Bartolozzi C. Choledocolithiasis: diagnostic accuracy of MR cholangiopancreatography. Three-year experience. Magn Reson Imaging. 1999;17:1245–1253. doi: 10.1016/s0730-725x(99)00075-2. [DOI] [PubMed] [Google Scholar]
- 27.Chan YL, Chan AC, Lam WW, Lee DW, Chung SS, Sung JJ, Cheung HS, Li AK, Metreweli C. Choledocholithiasis: comparison of MR cholangiography and endoscopic retrograde cholangiography. Radiology. 1996;200:85–89. doi: 10.1148/radiology.200.1.8657949. [DOI] [PubMed] [Google Scholar]
- 28.Fulcher AS, Turner MA, Capps GW, Zfass AM, Baker KM. Half-Fourier RARE MR cholangiopancreatography: experience in 300 subjects. Radiology. 1998;207:21–32. doi: 10.1148/radiology.207.1.9530295. [DOI] [PubMed] [Google Scholar]
- 29.Yeh TS, Jan YY, Tseng JH, Hwang TL, Jeng LB, Chen MF. Value of magnetic resonance cholangiopancreatography in demonstrating major bile duct injuries following laparoscopic cholecystectomy. Br J Surg. 1999;86:181–184. doi: 10.1046/j.1365-2168.1999.01029.x. [DOI] [PubMed] [Google Scholar]
- 30.Matos C, Metens T, Devière J, Nicaise N, Braudé P, Van Yperen G, Cremer M, Struyven J. Pancreatic duct: morphologic and functional evaluation with dynamic MR pancreatography after secretin stimulation. Radiology. 1997;203:435–441. doi: 10.1148/radiology.203.2.9114101. [DOI] [PubMed] [Google Scholar]
- 31.Takehara Y. MR pancreatography. Semin Ultrasound CT MR. 1999;20:324–339. doi: 10.1016/s0887-2171(99)90064-1. [DOI] [PubMed] [Google Scholar]
- 32.Manfredi R, Costamagna G, Brizi MG, Maresca G, Vecchioli A, Colagrande C, Marano P. Severe chronic pancreatitis versus suspected pancreatic disease: dynamic MR cholangiopancreatography after secretin stimulation. Radiology. 2000;214:849–855. doi: 10.1148/radiology.214.3.r00mr24849. [DOI] [PubMed] [Google Scholar]
- 33.Irie H, Honda H, Jimi M, Yokohata K, Chijiiwa K, Kuroiwa T, Hanada K, Yoshimitsu K, Tajima T, Matsuo S, et al. Value of MR cholangiopancreatography in evaluating choledochal cysts. AJR Am J Roentgenol. 1998;171:1381–1385. doi: 10.2214/ajr.171.5.9798883. [DOI] [PubMed] [Google Scholar]


