Background:
Young breast cancer survivors have specific needs related to age. Clarifying the relationships between unmet information needs and quality of life (QOL) in young breast cancer survivors can contribute to constructing a support system to enhance QOL in patients.
Objective:
This study aimed to identify the unmet information needs and examine the relationships between unmet information needs and QOL in young breast cancer survivors in Japan.
Methods:
Participants completed an information needs questionnaire containing 26 items, the World Health Organization Quality of Life Instrument–Short Form (WHOQOL-BREF), and a demographic and medical information questionnaire.
Results:
Fifty participants (30.7%) were unsatisfied with “overall communication with medical professionals.” The mean scores on all subscales of the WHOQOL-BREF of the participants who were satisfied with “overall communication with medical professionals” were significantly higher than those of the unsatisfied group. “follow-up tests,” “treatment for recurrence of breast cancer,” “strategies about communication with medical staff,” and “nutrition” were significantly related with all subscales in the WHOQOL-BREF. “Secondary menopause caused by hormonal therapy” was significantly related with physical and psychological health.
Conclusions:
Japanese young breast cancer survivors have unmet information needs, including age-specific issues. These unmet information needs are related to QOL. In particular, “overall communication with medical professionals,” which is the most unmet information need, is related to QOL.
Implications for Practice:
Oncology nurses should teach patients communication skills, provide adequate information, and provide education and emotional support to medical professionals to improve QOL in young breast cancer survivors.
KEY WORDS: Breast cancer, Quality of life, Unmet information needs, Young survivors
Breast cancer is the most commonly diagnosed cancer in women younger than 50 years in the United States.1 In Japan, breast cancer is the most common malignancy among women.2 The Center for Cancer Control and Information Services at the National Cancer Center Japan estimated that 1 of every 14 women will be diagnosed with breast cancer during their lifetime.3 In 2010, 14.8% of all newly diagnosed breast cancer patients were younger than 45 years.3 With the increasing number of younger women with breast cancer and higher survival rate, the ranks of young breast cancer survivors are growing.
Breast tumors in young breast cancer patients tend to be more aggressive and at a higher stage at diagnosis.4 A retrospective study using the Japanese Breast Cancer Society database indicated that young women with breast cancer tend to be diagnosed with larger tumors and at a more advanced stage than nonyoung patients are.5
Medical professionals have recognized quality of life (QOL) as a primary outcome in cancer patients. Information on QOL is critically important for several stages of the cancer trajectory, including the therapeutic phase, long-term survivorship, palliative care, and end-of-life care. Breast cancer in young patients has a greater negative effect on QOL.6–9 In young breast cancer survivors, QOL is lower compared with older women with breast cancer and same-age women without breast cancer, and the age-related factors associated with QOL were sexual or body image problems and vaginal dryness associated with impaired QOL.9
Young breast cancer survivors, who are generally of reproductive age, have specific issues related to age. Because adjuvant therapy for breast cancer, including chemotherapy and/or hormonal therapy, causes premature menopause, fertility is a very crucial issue.10 A previous study has predicted that the risk of menopause caused by chemotherapy and/or hormonal therapy in 40-year-old women is from less than 5% to more than 40%.11 Young breast cancer patients must decide on whether to receive adjuvant therapy and need accurate and timely information.6 As to the follow-up phase, particular issues in young breast cancer patients at follow-up clinics are fertility and pregnancy, hot flashes, premature menopause, and psychological problems.12 In focus group discussions, the following key concerns of young women with breast cancer have been identified: anxiety about not being able to see their children grow up, feeling that they are too young to have developed breast cancer, feeling different from other women their age, and loss of choice about having children.13
Information is helpful for cancer survivors to cope with their physical and psychological problems; thus, it is important to assess whether the information meets the needs of young breast cancer survivors. Research findings on young adult cancer survivors have indicated that the needs of more than 50% of the respondents had been unmet despite the desire for age-appropriate cancer information, as well as information on diet, exercise, infertility, mental health counseling, and camp or retreat programs, suggesting a need to promote provision of supportive care.14 In a previous study, women younger than 50 years with breast cancer were more concerned about finances, work, and self-esteem than were women older than 50 years.15 Furthermore, in a study that investigated the needs and recommendations of Canadian young breast cancer survivors, accessible information, support, and services were not age appropriate, and they recommended support that matched their stage of life and workshops about sexuality and lymph edema.16 It is necessary to identify unmet information needs in detail to provide information that addresses the various issues pertinent to young breast cancer survivors.
Although there have been several studies that have investigated the unmet information needs of cancer survivors,17 there has not been quantitative research that has surveyed the unmet information needs in young breast cancer survivors in Japan. Clarifying the relationships between the unmet information needs and QOL in young breast cancer survivors can contribute to constructing a support system to enhance QOL in patients. The purposes of this study were to identify unmet information needs and examine the relationships between unmet information needs and QOL in young breast cancer survivors in Japan.
Unmet Information Needs
Needs assessments directly assess and identify specific issues of need for patients,18 thereby contributing to the provision of high-quality nursing care for patients with cancer. Research on needs assessments for patients with cancer evaluates unmet supportive care needs (unmet needs) that require some kind of desired service or support to achieve optimal well-being.18–20 We posit that unmet information needs can be defined as the requirement of desirable or necessary information whose provision is essential to achieve optimal well-being.21,22
There are several measurements to assess unmet needs, such as the Supportive Care Needs Survey–Short Form23 and the Cancer Survivors’ Unmet Needs measure.20 The Supportive Care Needs Survey–Short Form has good reliability, with Cronbach’s α coefficients ranging from .86 to .96, and good convergent validity (r = 0.48–0.56).23 The Cancer Survivors’ Unmet Needs measure was found to have a Cronbach’s α coefficient of .96 and the construct validity was acceptable.20 However, specific unmet information needs in young breast cancer survivors have not been evaluated by these measurements. It is important to assess unmet information needs based on patient perceptions of necessary information.
Conceptual Framework
According to stress and coping theory, information is a resource that aids adjustment.24 As we mentioned above, unmet information needs are identified based on patient satisfaction with the information to implement nursing practices that meet specific unmet needs in young breast cancer survivors.
One of the indicators of adjustment in patients with cancer is QOL. Because the concept of QOL is a multidimensional construct, it is a useful parameter in predicting outcomes in oncology nursing.25 In previous studies that described QOL in breast cancer patients, the concepts of QOL were defined in the context of cancer patients’ specific or general outcomes.26–30 We applied the concept of generic health-related QOL to make comparisons with people without cancer. Hence, we have adopted the following definition of QOL proposed by the World Health Organization: “an individual’s perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards, and concerns.”31
The relationship between unmet information needs and QOL has been described in a few studies. In previous studies of breast cancer patients who had no evidence of systemic metastasis, unmet needs, including unmet information needs, were significantly associated with QOL.32 Research findings on advanced breast cancer patients have also indicated that unmet information needs are significantly related to QOL.33 However, to our knowledge, no studies have investigated the relationship between unmet information needs and QOL in young breast cancer survivors. Furthermore, detailed information about unmet information needs influencing QOL have not been described in most studies that have comprehensively assessed unmet information needs.
Methods
Design
A cross-sectional descriptive research design was used to survey unmet information needs and QOL.
Participants and Procedure
Participants were recruited at Hiroshima University Hospital and National Hospital Organization Kyushu Cancer Center. These hospitals have been designated as regional cancer centers and hospitals in Japan, in an effort by the Japanese Ministry of Health, Labour, and Welfare to fight against cancer. Before the survey, this study was approved by the institutional review boards at both hospitals.
Study participants were recruited by consecutive sampling. Inclusion criteria for study participants were Japanese women who had been diagnosed with breast cancer at 45 years old or younger. All Japanese women with breast cancer, regardless of stage, time since diagnosis, or treatment status, were included. Exclusion criteria were patients who could not write Japanese or had severe physical or psychological problems.
All eligible women were introduced by physicians to research assistants, who were nurses. Five research assistants explained the details of the study to eligible women at breast cancer outpatient clinics at the 2 hospitals. After the participants signed a consent form, they were handed a self-report questionnaire. They completed the questionnaire at home by themselves and sent it to the authors by mail.
Measures
QUALITY OF LIFE
The Japanese version of the World Health Organization Quality of Life Instrument–Short Form (WHOQOL-BREF), consisting of 26 items, was used to measure QOL.34 A diversity of health-related QOL measurements are available, some of which are generic and some disease specific. In this study, we applied a generic health-related QOL measurement so that we could make comparisons with people without cancer. The WHOQOL-BREF,35,36 which is a 26-item version of the WHOQOL-100,37 is a generic health-related QOL measurement. Internal consistency of the Japanese version was fairly good, with Cronbach’s α coefficients ranging from .66 to .84.34 Each item was scored on a 5-point Likert scale. Four domains were assessed: physical health (eg, pain and discomfort, vigor, and fatigue), psychological health (eg, positive feelings and negative feelings), social relationships (eg, social support and sexual activities), and environment (eg, opportunity for leisure activities and safety in daily life). The scores on each domain were transformed on a scale of a hundred. Higher scores indicated better QOL.
UNMET INFORMATION NEEDS
Unmet information needs were assessed by a questionnaire constructed of 26 questions on a 4-point Likert-scale that asked about satisfaction with information received from medical professionals. The questionnaire also included 1 question that asked about satisfaction with overall communication with medical professionals. The questions were created on the basis of results of a focus group discussion aimed at identifying what difficulties young breast cancer survivors had and what information they expected to receive. Each question could be answered by selecting “very satisfied,” “moderately satisfied,” “little unsatisfied,” or “unsatisfied.” If study participants did not receive the information, they could answer “not received.” The contents of our questionnaire are consistent with a previous study that developed measurements of satisfaction with information in breast cancer survivors. Although the measurements assessed diagnosis and treatment-related issues, as well as survivorship issues, they did not evaluate specific issues in young breast cancer survivors.38 In this study, the questions included specific issues pertinent to young breast cancer survivors, such as secondary menopause caused by chemotherapy or hormonal therapy and fertility after the therapies. Because this survey focused on necessary or desirable information, the term medical professionals included physician, nurse, and other medical staff.
DEMOGRAPHIC AND CLINICAL VARIABLES
We asked participants about cancer stage, months since diagnosis, type of surgery, adjuvant therapy, symptoms, education, and satisfaction with their income. Age, marital status, number of children, employment status, and menopausal status at diagnosis (ie, when they were diagnosed with breast cancer) and at the time of the survey (ie, when they responded to this survey) were obtained.
Data Analysis
Data were analyzed using SPSS version 20.0. Descriptive statistics were calculated for all variables. Participants were classified in a satisfied group (ie, very satisfied or moderately satisfied) or an unsatisfied group (little unsatisfied or unsatisfied) based on their answers for the unmet needs questionnaire. Normality was tested by the Kolmogorov-Smirnov test for scores on the WHOQOL-BREF. Mann-Whitney U test was performed to determine whether there were differences in mean scores on the WHOQOL-BREF between participants who were satisfied with the information and those who were unsatisfied.
Results
Participants
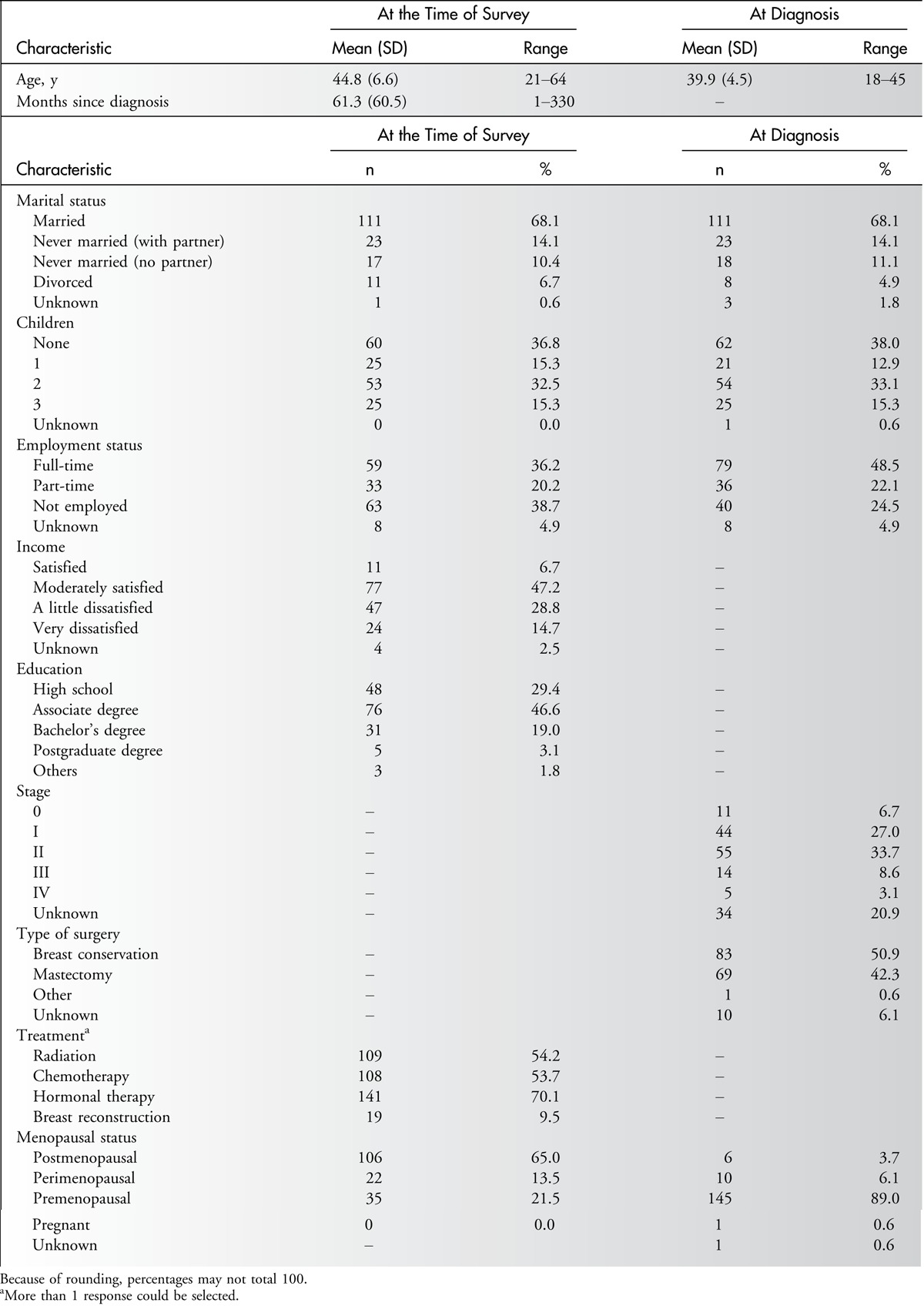
A total of 308 women signed the consent form of this survey, of whom 163 (52.9%) returned the questionnaire. The demographic and clinical characteristics of the 163 participants are presented in Table 1. The mean ages at diagnosis and at the time of the survey were 39.9 ± 4.5 years (range, 18–45 years) and 44.8 ± 6.6 years (range, 21–64 years), respectively. The average time since diagnosis of breast cancer was 61.3 ± 60.5 months. A total of 111 (68.1%) participants were married at diagnosis and at the time of the survey. Among the participants, 79 (48.5%) were employed full-time at diagnosis and 59 (36.2%) at the time of the survey. About half of the participants (50.9%) have undergone conservative surgery for breast cancer. At diagnosis, 145 (89.0%) participants were premenopausal women and 106 (65.0%) were in a state of amenorrhea at the time of the survey. About 70% of the participants have received hormonal therapy.
Table 1.
Demographic and Clinical Characteristics (N = 163)
Unmet Information Needs
The number and percentage of participants who received information from medical professionals, as well as those of participants satisfied or unsatisfied with the information, are shown in Table 2. Fifty participants (30.7%) were unsatisfied with “overall communication with medical professionals.” All participants received information on “results of diagnostic tests,” and 77.9% (n = 127) were satisfied with the information. Although most of the study participants received information on “follow-up tests” (n = 155, 95.1%), “possible symptoms after hospital discharge” (n = 142, 87.1%), and “lymphedema” (n = 129, 79.1%), more than a quarter of the participants were dissatisfied with the information (n = 39, 25.2%; n = 41, 28.9%; n = 37, 28.7%, respectively).
Table 2.
Number and Percentage of Participants Who Were Satisfied or Unsatisfied With the Information Received From Medical Professionals (N = 163)
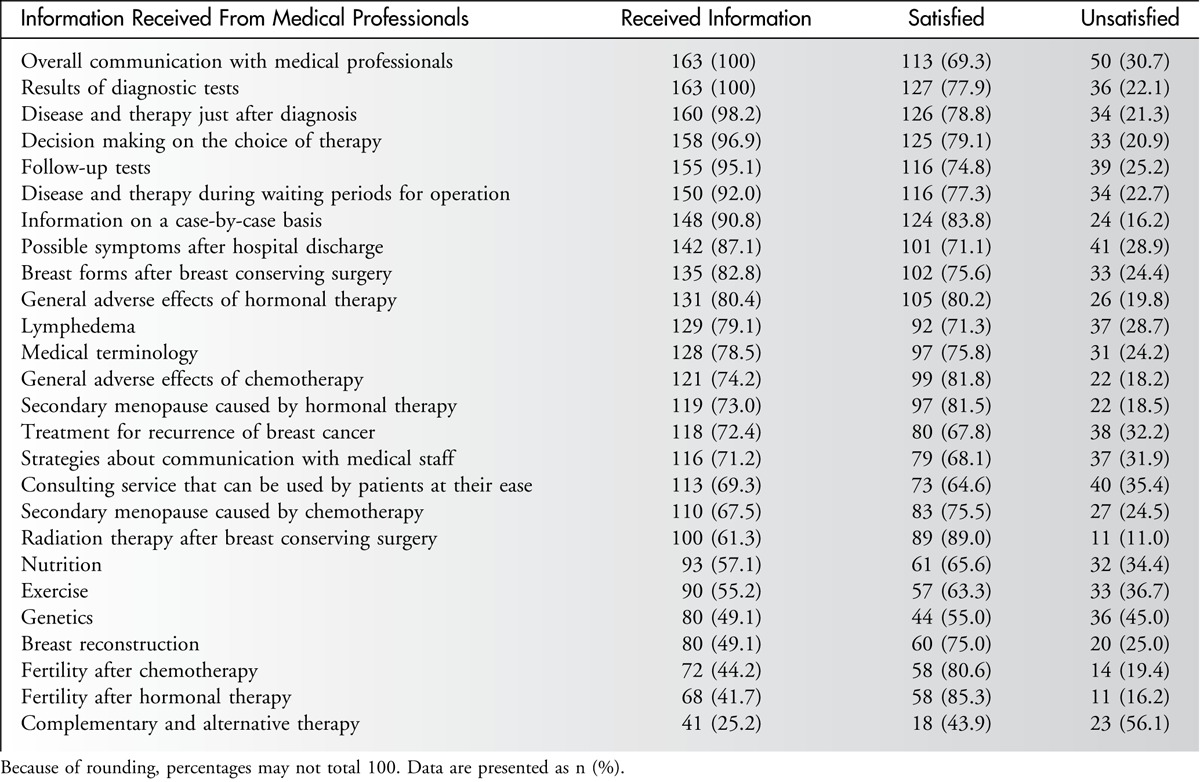
Around 70% of the participants received information on “treatment for recurrence of breast cancer” (n = 118, 72.4%), “strategies about communication with medical staff” (n = 116, 71.2%), and “consulting service that can be used by participants at their ease” (n = 113, 69.3%), and more than 30% of the participants were unsatisfied with the information (n = 38, 32.2%; n = 37, 31.9%; n = 40, 35.4%, respectively).
The percentages of participants who reported dissatisfaction with the information on “nutrition,” “exercise,” and “genetics,” which was received by only about a half of the participants, were relatively high (34.4%, 36.7%, and 45.0%, respectively). Only 41 participants (25.2%) received information on “complementary and alternative therapy,” and more than half of them (n = 23, 56.1%) were unsatisfied with the information.
As to specific information pertinent to young breast cancer survivors, around 70% of the participants received information on “secondary menopause caused by hormonal therapy” and “secondary menopause caused by chemotherapy.” The percentage of patients who were unsatisfied with the information on “secondary menopause caused by chemotherapy” was relatively high (n = 27, 24.5%). There were about 70 participants who received information on “fertility after chemotherapy” and “fertility after hormonal therapy,” and the percentage of participants who were dissatisfied with that information did not reach 20%.
Quality of Life
The mean scores on the WHOQOL-BREF subscales physical health, psychological health, social relationships, and environment were 71.6 ± 13.7, 69.8 ± 14.0, 69.7 ± 12.9, and 68.3 ± 11.9, respectively. In comparison with the mean scores of general Japanese women of the same age (69.4, 66.2, 65.6, and 63.6, respectively),34 the mean scores of the study participants were rather good.
Relationships Between Unmet Information Needs and QOL
Because the normality of the score of each subscale of the WHOQOL-BREF was not sustained, the Mann-Whitney U test was performed to examine the relationships between unmet information needs and QOL. For information in which more than 25% of the participants were dissatisfied with it, among the participants who received the information, the relationships between the satisfaction with the information and QOL were examined by comparing the mean scores on the WHOQOL-BREF subscales between the satisfied group and the unsatisfied group. In addition, the relationships between unmet information needs related to specific issues pertinent to young breast cancer survivors were examined.
Table 3 shows the mean scores on the WHOQOL-BREF subscales of the 2 groups among participants who received information. The mean scores on all subscales of the WHOQOL-BREF of the participants who were satisfied with “overall communication with medical professionals” were significantly higher than those of the unsatisfied group (U = 2246, P = .037; U = 1980, P = .002; U = 2254, P = .037; U = 2257, P = .040, respectively). “follow-up tests” (U = 1526, P = .002; U = 1456, P = .001; U = 1615, P = .007; U = 1712, P = .023), “treatment for recurrence of breast cancer” (U = 1148, P = .032; U = 1053, P = .007; U = 1061, P = .007; U = 903, P < .001), “strategies about communication with medical staff” (U = 827, P < .001; U = 927, P = .001; U = 1121, P = .040; U = 1054 P = .015), and “nutrition” (U = 634, P = .006; U = 661, P = .011; U = 689, P = .018; U = 639, P = .006) were significantly related with all subscales in the WHOQOL-BREF. The mean scores on all subscales of the WHOQOL-BREF, except environment, which was marginally related (U = 1141, P = .054), of participants who were satisfied with information on “consulting service that can be used by patients at their ease” were significantly higher than the scores of those in the unsatisfied group (U = 1115, P = .038; U = 1064, P = .017; U = 1068, P = .017). As to “lymphedema” (U = 1236, P = .015; U = 1323, P = .047) and “complementary and alternative therapy” (U = 107, P = .008; U = 99, P = .004), there were significant differences in the mean scores on psychological health and environment between the 2 groups. The mean scores on all subscales of the WHOQOL-BREF, except social relationships, of participants who were satisfied with information on “exercise” were significantly higher than the scores of those in the unsatisfied group (U = 649, P = .014; U = 672, P = .024; U = 641, P = .012).
Table 3.
Mean Scores on the World Health Organization Quality of Life Instrument–Short Form (WHOQOL-BREF) Subscales of the Satisfied Group and Unsatisfied Group Among Patients Who Received Information
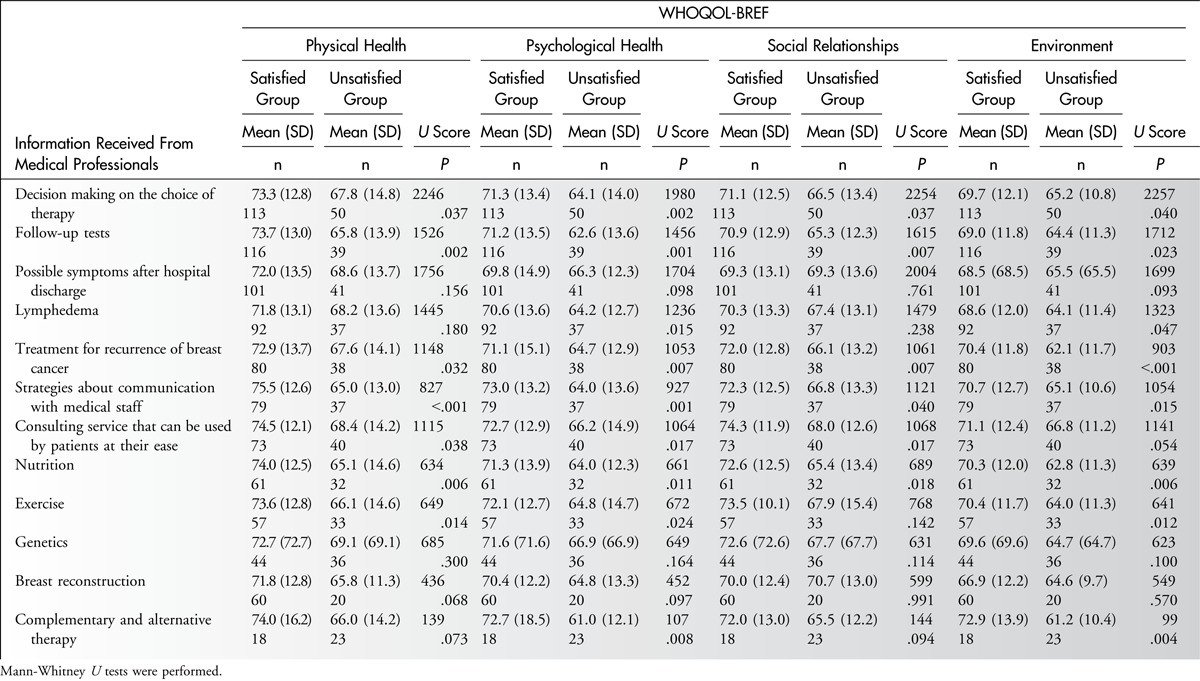
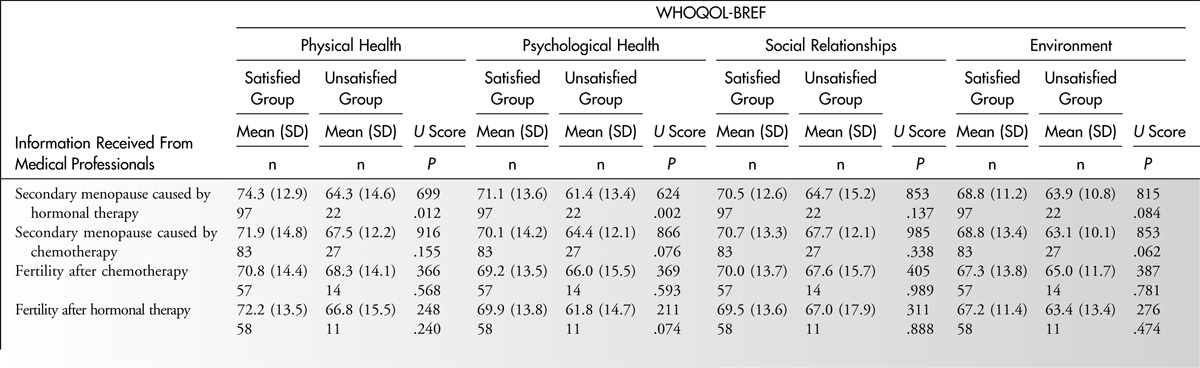
Table 4 shows the mean scores on the WHOQOL-BREF subscales of the satisfied group and unsatisfied group among participants who received information on specific issues pertinent to young breast cancer survivors. Only “secondary menopause caused by hormonal therapy” was significantly related with physical and psychological health (U = 669, P = .012; U = 624, P = .002).
Table 4.
Mean Scores on the World Health Organization Quality of Life Instrument–Short Form (WHOQOL-BREF) Subscales of the Satisfied Group and Unsatisfied Group Among Patients Who Received Information on Specific Issues Pertinent to Young Breast Cancer Survivors
Discussion
This study identified unmet information needs and explored the relationships between unmet information needs and QOL in young breast cancer survivors in Japan. The results of this study suggest that young breast cancer survivors have unmet information needs that are related to QOL.
Communication is an important way to collect information. In this study, more than 30% of the participants were unsatisfied with “overall communication with medical professionals.” In previous studies, younger breast cancer patients were less satisfied with the information they had received.39,40 Young breast cancer survivors tend to expect participation in decision making and have needs that are different from those of elderly patients.41 Patients of reproductive age often have to make a decision on adjuvant therapy. Although a previous study indicated that Japanese oncologists have, in general, a positive attitude toward discussing fertility issues with young breast cancer patients, it was suggested that a comprehensive and interdisciplinary program is needed to meet breast cancer patients’ needs.42 It was also suggested that multidisciplinary team approaches were insufficient in supporting young breast cancer patients in Japan. Furthermore, telling young children of breast cancer patients about their illness is a serious issue. A qualitative study of Japanese breast cancer patients who had school-age children described the decision-making process of telling their children about their illness and indicated that support from others is a special need of patients who consider that there are more negative aspects than positive aspects in telling their children about their illness.43 Younger patients may have specific needs in communication with medical professionals.
In this study, all participants received explanations on the “results of diagnostic tests,” and most of the participants were satisfied with the explanations. As physicians explain results of diagnostic tests based on objective data, they can provide certain information. However, it may be difficult to provide certain information about individual future events, including follow-up tests, possible symptoms, lymphedema, and cancer recurrence. Although around half of the participants in this study received information about “nutrition,” “exercise,” and “genetics,” the percentage of participants who reported dissatisfaction with the information was relatively high. Because medical professionals are not experts in nutrition or exercise, they may not have enough knowledge. Only 41 participants (25.2%) in this study received information on “complementary and alternative therapy.” As previous research has shown that the information sources of complementary and alternative therapy are outside the medical system,44 study participants might not prefer to seek information from medical professionals. However, in a previous study that described supportive care needs in disease-free breast cancer survivors, 1 in 4 survivors had reported an unmet need for access to complementary and/or alternative therapy services.45 It is necessary to provide useful information about complementary and alternative therapy to patients according to their needs.
As to specific information pertinent to young breast cancer survivors, the percentage of participants in this study who received information about secondary menopause was around 70%, but less than half of the participants received information about fertility. Previous studies, in which the mean age of the participants was about 35 years, showed that about 70% of the study participants received information about fertility.46,47 Because the mean age of participants in this study was 44.8 ± 6.6 years (range, 21–64 years), there might have been a tendency to provide information about fertility to a relatively lower number of participants. The percentage of participants in this study who were unsatisfied with information on “secondary menopause caused by chemotherapy” was relatively high. A previous qualitative study of 20 young breast cancer patients (mean age, 40.2 ± 5.2 years) described that they had not received enough counseling.47 Medical professionals should provide information and counseling service by experts who are trained in the care of breast cancer patients, taking into consideration the age and preference of patients.
This study explored the relationships between unmet information needs and QOL in young breast cancer survivors. There was a significant relationship between “overall communication with medical professionals” and QOL. This finding is similar to that of a previous study that found that patients younger than 50 years were less satisfied with the information they had received.48 This study investigated the relationships between satisfaction with specific kinds of information and QOL. “Strategies about communication with medical staff” and “consulting service that can be used by patients at their ease” were significantly related to all subscales of the WHOQOL-BREF. An earlier study indicated that breast cancer survivors (mean age, 44.0 ± 4.8 years) had more than 1 problem communicating with physicians on average.49 Providing information about strategies of communication to patients may positively affect their QOL through promoting their coping skills. In addition, physicians, especially oncologists, have difficulties in handling their own feelings.50 It may be useful to provide education and emotional support to physicians to improve communication between medical professionals and cancer patients.
There are several unmet information needs related to QOL as well as communication issues. Information on “follow-up tests” and “treatment for recurrence of breast cancer,” which were both related to all QOL subscales, may enhance patients’ understanding of their future prospects and prepare them for serious events. Information about “lymphedema,” “nutrition,” and “exercise” was related to the WHOQOL-BREF subscales. The information may be provided by experts or therapists who specialize in these areas. Hence, it is important that oncology nurses coordinate care through an interdisciplinary team approach to provide useful information to patients. As to complementary and alternative therapy, which is not a standard therapy in Japan, a previous study indicated that about 45% of Japanese breast cancer patients used complementary and alternative therapy.51 Furthermore, in a previous study, most patients started using complementary and alternative therapy on the advice of their family or friends, and more than half of the patients used the therapy without receiving enough information about it.51 It is important to provide reliable information about complementary and alternative therapy and their safety.
Only satisfaction with information on “secondary menopause caused by hormonal therapy” was related to physical and psychological health on the WHOQOL-BREF subscales. Early menopause might be extremely distressing and have the potential for negative effects on QOL in younger women compared with women in their 50s.52 Because 145 (89.0%) of the 163 participants in this survey were premenopausal at diagnosis and 106 (65.0%) were in a state of amenorrhea at the time of the survey, information on secondary menopause had an influence on the physical and psychological health of participants in this study.
Limitations
This study has several limitations. The main limitation is that we asked only about satisfaction with information received from medical professionals. Unmet information needs should be assessed not only in terms of patient satisfaction with the information but also in terms of the necessity of the information for the patients. Another limitation is that participants were recruited from only 2 hospitals. The study participants may not be representative of young breast cancer survivors in Japan. In addition, QOL in the study participants was not any worse than in that in general women. Finally, the mean age of participants was not relatively low. It is possible that younger patients may have different issues from those in their 40s. The findings from this study have generalization limitations, and so a nationwide survey that considers patients’ perception of the necessity of information is required.
Implications for Nursing Practice
This study suggests that promoting communication between patients and medical professionals may ameliorate QOL in young breast cancer survivors. Oncology nurses should teach patients communication skills and provide adequate information with consideration of age to meet unmet needs. Oncology nurses should be aware of the unmet information needs and support patients so that they can communicate with medical professionals. It is necessary to develop a brief assessment tool to detect the needs of younger breast cancer survivors and to encourage oncology nurses to actively assess the information needs of patients. In addition, assisting and educating medical professionals may enhance communication with cancer patients. A previous study described that physicians have some barriers in communicating treatment plans.50 It may be helpful for physicians to receive assistance from oncology nurses in communicating with patients. Survivorship care plans that are effective in improving interaction between patients and medical professionals,53 reducing patients’ unmet needs,54 and improving quality of care55 have been developed in the United States. Developing a survivorship care plan focusing on age-specific needs may enhance QOL in young breast cancer survivors in Japan.
Conclusions
This study identified the unmet information needs that are related to QOL in young breast cancer survivors in Japan. Satisfaction with overall communication with medical professionals, which is related to QOL, is the most unmet need. Information on secondary menopause, which is an age-specific issue, is not being met, and that may impact QOL in young breast cancer survivors. Future research assessing patient perception of the need of information should provide more detailed knowledge about unmet information needs. In addition, a nationwide survey on younger breast cancer survivors is necessary to correctly identify specific unmet information needs. This study suggests that oncology nurses should teach patients communication skills and provide adequate information with consideration of age to meet the unmet information needs. It is necessary to develop a brief assessment tool to detect the needs of younger breast cancer survivors. Furthermore, it is important that oncology nurses provide education and emotional support to medical professionals to enhance communication between cancer patients and medical professionals. A survivorship care plan focusing on age-specific issues may be able to enhance QOL in young breast cancer survivors.
Footnotes
This research was supported by JSPS KAKENHI grant number 20592540 and by research fund from the Japanese Breast Cancer Society.
The authors have no conflicts of interest to disclose.
References
- 1. Siege R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014; 64 (1): 9– 29. [DOI] [PubMed] [Google Scholar]
- 2. Matsuda T, Marugame T, Kamo KI, Katanoda K, Ajiki W, Sobue T.The Japan Cancer Surveillance Research Group. Cancer incidence and incidence rates in Japan in 2005: based on data from 12 population-based Cancer registries in the Monitoring of Cancer Incidence in Japan (MCIJ) Project. Jpn J Clin Oncol. 2011; 41: 139– 147. [DOI] [PubMed] [Google Scholar]
- 3.Center for Cancer Control and Information Services. http://ganjoho.jp/public/statistics/pub/statistics01.html. Accessed May 24, 2014.
- 4. Freedman RA, Partridge AH. Adjuvant therapies for very young women with early stage breast cancer. The Breast. 2011; 20 (Suppl 3): S146– S149. [DOI] [PubMed] [Google Scholar]
- 5. Kataoka A, Tokunaga E, Masuda N, Shien T, Kawabata K, Miyashita M. Clinicopathological features of young patients (<35 years of age) with breast cancer in a Japanese Breast Cancer Society supported study [published online ahead of print] Breast Cancer. 2013. http://link.springer.com/article/10.1007%2Fs12282-013-0466-2/fulltext.html. Accessed June 1, 2014. [DOI] [PubMed] [Google Scholar]
- 6. Wenzel LB, Fairclough DL, Brady MJ, et al. Age-related differences in the quality of life of breast carcinoma patients after treatment. Cancer. 1999; 86 (9): 1768– 1774. [PubMed] [Google Scholar]
- 7. Kroenke CH, Rosner B, Chen WY, Kawachi I, Colditz GA, Holmes MD. Functional impact of breast cancer by age at diagnosis. J Clin Oncol. 2004; 22 (10): 1849– 1856. [DOI] [PubMed] [Google Scholar]
- 8. Rosen A, Rodriguez-Wallberg KA, Rosenzweig L. Psychosocial distress in young cancer survivors. Semin Oncol Nurs. 2009; 25 (4): 268– 277. [DOI] [PubMed] [Google Scholar]
- 9. Avis NE, Crawford S, Manuel J. Quality of life among younger women with breast cancer. J Clin Oncol. 2005; 23 (15): 3322– 3330. [DOI] [PubMed] [Google Scholar]
- 10. Camp-Sorrell D. Cancer and its treatment effect on young breast cancer survivors. Semin Oncol Nurs. 2009; 25 (4): 251– 258. [DOI] [PubMed] [Google Scholar]
- 11. Goodwin PJ, Ennis M, Pritchard KI, Trudeau M, Hood N. Risk of menopause during the first year after breast cancer diagnosis. J Clin Oncol. 1999; 8 (17): 2365– 2370. [DOI] [PubMed] [Google Scholar]
- 12. Roche N. Follow-up after treatment for breast cancer in young women. The Breast. 2006; 15 (52): 571– 575. [DOI] [PubMed] [Google Scholar]
- 13. Dunn J, Steginga SK. Young women’s experience of breast cancer: defining young and identifying concerns. Psychooncology. 2000; 9 (2): 137– 146. [DOI] [PubMed] [Google Scholar]
- 14. Zebrack B. Information and service needs for young adult cancer survivors. Support Care Cancer. 2009; 17 (4): 349– 357. [DOI] [PubMed] [Google Scholar]
- 15. Wang X, Cosby LG, Harris MG, Liu T. Major concerns and needs of breast cancer patients. Cancer Nurs. 1999; 22 (2): 157– 163. [DOI] [PubMed] [Google Scholar]
- 16. Gould J, Grassau P, Manthorne J, Gray RE, Fitch MI. ‘Nothing fit me’: nationwide consultations with young women with breast cancer. Health Expect. 2006; 9 (2): 158– 173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rutten LJ, Arora NK, Bakos AD, Aziz N, Rowland J. Information needs and sources of information among cancer patients: a systematic review of research (1980-2003). Patient Educ Couns. 2005; 57 (3): 250– 261. [DOI] [PubMed] [Google Scholar]
- 18. Sanson-Fisher R, Girgis A, Boyes A, Bonevski B, Burton L, Cook P. The unmet supportive care needs of patients with cancer. Cancer. 2000; 88 (1): 226– 237. [DOI] [PubMed] [Google Scholar]
- 19. Bonevski B, Sanson-Fisher R, Girgis A, Burton L, Cook P, Boyes A. Supportive Care Review Group. Evaluation of an instrument to assess the needs of patients with cancer. Cancer. 2000; 88 (1): 217– 225. [DOI] [PubMed] [Google Scholar]
- 20. Hodgkinson K, Butow P, Hunt GE, et al. The development and evaluation of a measure to assess cancer survivors’ unmet supportive care needs: the CaSUN (Cancer Survivors’ Unmet Needs measure). Psychooncology. 2007; 16 (9): 796– 804. [DOI] [PubMed] [Google Scholar]
- 21. Carey M, Lambert S, Smits R, Paul C, Sanson-Fisher R, Clinton-McHarg T. The unfulfilled promise: a systematic review of interventions to reduce the unmet supportive care needs of cancer patients. Support Care Cancer. 2012; 20 (2): 207– 219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Campbell HS, Sanson-Fisher R, Taylor-Brown J, Hayward L, Wang XS, Turner D. The cancer support person’s unmet needs survey: psychometric properties. Cancer. 2009; 115 (14): 3351– 3359. [DOI] [PubMed] [Google Scholar]
- 23. Boyes A, Girgis A, Lecathelinais C. Brief assessment of adult cancer patients’ perceived needs: development and validation of the 34-item Supportive Care Needs Survey (SCNS-SF34). J Eval Clin Pract. 2009; 15 (4): 602– 606. [DOI] [PubMed] [Google Scholar]
- 24. Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York, NY: Springer-Verlag; 1984. [Google Scholar]
- 25. Ferrans CE, Hacker ED. Quality of life as an outcome of cancer care. In Yarbro CH, Hansen-Frogge M, Goodman M, eds. Cancer Nursing: Principles and Practice. 7th ed Boston, MA: Jones & Bartlett Publishers; 2011: 201– 218. [Google Scholar]
- 26. Moreira H, Silva S, Canavarro MC. The role of appearance investment in the adjustment of women with breast cancer. Psychooncology. 2010; 19 (9): 959– 966. [DOI] [PubMed] [Google Scholar]
- 27. Hyphantis T, Almyroudi A, Paika V, Degner LF, Carvalho AF, Pavlidis N. Anxiety, depression and defense mechanisms associated with treatment decisional preferences and quality of life in non-metastatic breast cancer: a 1-year prospective study. Psychooncology. 2013; 22 (11): 2470– 2477. [DOI] [PubMed] [Google Scholar]
- 28. Ashing-Giwa KT, Lim JW. Examining emotional outcomes among a multiethnic cohort of breast cancer survivors. Oncol Nurs Forum. 2011; 38 (3): 279– 288. [DOI] [PubMed] [Google Scholar]
- 29. Howard-Anderson J, Ganz PA, Bower JE, Stanton AL. Quality of life, fertility concerns, and behavioral health outcomes in younger breast cancer survivors: a systematic review. J Natl Cancer Inst. 2012; 104 (5): 386– 405. [DOI] [PubMed] [Google Scholar]
- 30. Chopra I, Kamal KM. A systematic review of quality of life instruments in long-term breast cancer survivors. Health Qual Life Outcomes. 2012; 10: 14 http://www.hqlo.com/content/pdf/1477-7525-10-14.pdf. Accessed May 27, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.The WHOQOL Group. The World Health Organization Quality of Life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med. 1995; 41 (10): 1403– 1409. [DOI] [PubMed] [Google Scholar]
- 32. Park BW, Hwang SY. Unmet needs of breast cancer patients relative to survival duration. Yonsei Med J. 2012; 53 (1): 118– 125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Uchida M, Akechi T, Okuyama T, et al. Patients’ supportive care needs and psychological distress in advanced breast cancer patients in Japan. Jpn J Clin Oncol. 2011; 41 (4): 530– 536. [DOI] [PubMed] [Google Scholar]
- 34. Tazaki M, Nakane M. WHOQOL26 Guidance. Tokyo, Japan: Kaneko-Shobo; 2007. [Google Scholar]
- 35.The WHOQOL Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. 1998; 28 (3): 551– 558. [DOI] [PubMed] [Google Scholar]
- 36. Skevington SM, Lotfy M, O’Connell KAWHOQOL Group. The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res. 2004; 13: 299– 310. [DOI] [PubMed] [Google Scholar]
- 37.The WHOQOL-Group. The World Health Organization Quality of Life Assessment (WHOQOL): development and general psychometric properties. Soc Sci Med. 1998; 46 (12): 1569– 1585. [DOI] [PubMed] [Google Scholar]
- 38. Griggs JJ, Sorbero ME, Mallinger JB, et al. Vitality, mental health, and satisfaction with information after breast cancer. Patient Educ Couns. 2007; 66 (1): 58– 66. [DOI] [PubMed] [Google Scholar]
- 39. Kerr J, Engel J, Schlesinger-Raab A, Sauer H, Hölzel D. Communication, quality of life and age: results of a 5-year prospective study in breast cancer patients. Ann Oncol. 2003; 14 (3): 421– 427. [DOI] [PubMed] [Google Scholar]
- 40. Robinson JD, Hoover DR, Venetis MK, Kearney TJ, Street RL., Jr Consultations between patients with breast cancer and surgeons: a pathway from patient-centered communication to reduced hopelessness. J Clin Oncol. 2013; 31 (3): 351– 358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bilodeau BA, Degner LF. Information needs, sources of information, and decisional roles in women with breast cancer. Oncol Nurs Forum. 1997; 23 (4): 691– 696. [PubMed] [Google Scholar]
- 42. Shimizu C, Bando H, Kato T, Mizota Y, Yamamoto S, Fujiwara Y. Physicians’ knowledge, attitude, and behavior regarding fertility issues for young breast cancer patients: a national survey for breast care specialists. Breast Cancer. 2013; 20 (3): 230– 240. [DOI] [PubMed] [Google Scholar]
- 43. Yoshida S, Otani H, Hirai K, et al. A qualitative study of decision-making by breast cancer patients about telling their children about their illness. Support Care Cancer. 2010; 18 (4): 439– 447. [DOI] [PubMed] [Google Scholar]
- 44. Tautz E, Momm F, Hasenburg A, Guethlin C. Use of complementary and alternative medicine in breast cancer patients and their experiences: a cross-sectional study. Eur J Cancer. 2012; 48: 3133– 3139. [DOI] [PubMed] [Google Scholar]
- 45. Hodgkinson K, Butow P, Hobbs KM, Wain G. After cancer: the unmet supportive care needs of survivors and their partners. J Psychosoc Oncol. 2007; 25 (4): 89– 104. [DOI] [PubMed] [Google Scholar]
- 46. Partridge AH, Gelber S, Peppercorn J, et al. Web-based survey of fertility issues in young women with breast cancer. J Clin Oncol. 2004; 22 (20): 4174– 4183. [DOI] [PubMed] [Google Scholar]
- 47. Thewes B, Meiser B, Taylor A, et al. Fertility- and menopause-related information needs of younger women with a diagnosis of early breast cancer. J Clin Oncol. 2005; 23 (22): 5155– 5164. [DOI] [PubMed] [Google Scholar]
- 48. Karaöz B, Aksu H, Küçük M. A qualitative study of the information needs of premenopausal women with breast cancer in terms of contraception, sexuality, early menopause, and fertility. Int J Gynaecol Obstet. 2010; 109 (2): 118– 120. [DOI] [PubMed] [Google Scholar]
- 49. Fernandes-Taylor S, Bloom JR. Post-treatment regret among young breast cancer survivors. Psychooncology. 2011; 20 (5): 506– 516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hillyer GC, Hershman DL, Kushi LH, et al. A survey of breast cancer physicians regarding patient involvement in breast cancer treatment decisions. Breast. 2013; 22 (4): 548– 554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Hyodo I, Amano N, Eguchi K, et al. Nationwide survey on complementary and alternative medicine in cancer patients in Japan. J Clin Oncol. 2005; 23 (12): 2645– 2654. [DOI] [PubMed] [Google Scholar]
- 52. Rosenberg SM, Partridge AH. Premature menopause in young breast cancer: effects on quality of life and treatment interventions. J Thorac Dis. 2013; 5 (S1): S55– S61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Ganz PA, Hahn EE. Implementing a survivorship care plan for patients with breast cancer. J Clin Oncol. 2008; 12 (5): 412– 417. [DOI] [PubMed] [Google Scholar]
- 54. Jefford M, Lotfi-Jam K, Baravelli C, et al. Development and pilot testing of a nurse-led posttreatment support package for bowel cancer survivors. Cancer Nurs. 2011; 34 (3): E1– E10. [DOI] [PubMed] [Google Scholar]
- 55. Rowland JH, Hewitt M, Ganz PA. Cancer survivorship: a new challenge in delivering quality cancer care. J Clin Oncol. 2006; 24 (32): 101– 105. [DOI] [PubMed] [Google Scholar]


