Abstract
Objective
The present study tested the feasibility of training peers with spinal cord injury (SCI) to learn brief action planning (BAP), an application of motivational interviewing principles, to promote physical activity to mentees with SCI.
Method
Thirteen peers with SCI attended a half-day BAP workshop. Using a one-arm, pre-, post-test design, feasibility to learn BAP was assessed in terms of peers' (1) BAP and motivational interviewing spirit competence; (2) training satisfaction; and (3) motivations to use BAP as assessed by measures of the theory of planned behavior constructs. Measures were taken at baseline, immediately post-training, and 1 month follow up.
Results
Following the training, participants' BAP and motivational interviewing competence significantly increased (P's < 0.05, d's > 2.27). Training satisfaction was very positive with all means falling above the scale midpoint. Participants' perceived behavioral control to use BAP increased from baseline to post (P < 0.05, d = 0.91) but was not maintained at follow up (P > 0.05).
Conclusion
Training peers with a SCI to learn to use BAP is feasible.
Practical implications
BAP is a tool that can be feasibly learned by peers to promote physical activity to their mentees.
Keywords: Spinal cord injury, Peers, Motivational interviewing, Brief action planning, Physical activity
Introduction
Despite the physical, psychological and social benefits of physical activity for people with spinal cord injury (SCI), physical activity promotion initiatives are sparse and physical activity participation rates are low among the SCI population.1–3 In recent years, physical activity guidelines for people with SCI were released and intervention studies have successfully identified behaviour change techniques (e.g. goal setting and action planning) to promote physical activity to people with SCI.4–7 Initial attempts to disseminate these guidelines and interventions have focused on event-based initiatives and passive mass media-based communication; however, evaluations of these initiatives indicate further efforts are needed to disseminate evidence-based physical activity promotion information and interventions to people with SCI.8
Peers promoting physical activity
Peers with a SCI have been identified as ideal individuals to promote physical activity within the SCI population. In general, peers are described as mentors with a SCI who provide encouragement and information to help individuals with SCI throughout their rehabilitation.9 These individuals may be volunteers or paid employees. Individuals with SCI perceive peers as credible messengers of physical activity information because peers can tailor information to an individual's specific needs.10,11
Despite the worldwide use of peers as information sources among organizations supporting individuals with SCI (e.g. Australia: Spinal Cord Injuries Association; Canada: Spinal Cord Injury Canada; UK: Spinal Injuries Association; USA: National Spinal Cord Injuries Association), research investigating the effectiveness of peer interactions for mobilizing evidence-based physical activity promotion materials to people with SCI had not been conducted. A systematic review of physical activity interventions found that peer-based interventions have a positive effect on physical activity behavior across a variety of populations.12 To gain further understanding of the role of peers for impacting physical activity behavior, research is needed to determine effective and feasible methods for peers to promote physical activity information to the SCI population.
Motivational interviewing
Motivational interviewing is an evidence-based approach that has potential utility for promoting physical activity to people with SCI through peer interactions. This style of behavior change counseling is a “client-centered, directive method for enhancing intrinsic motivation to change by exploring and resolving ambivalence”.13 Motivational interviewing and adaptations of motivational interviewing have been shown to promote physical activity among several populations.14–16 Likewise, a recent pilot study by Latimer-Cheung et al.17 found that a single motivational interviewing telecounseling session delivered by trained counselors strengthened social cognitions associated with physical activity among people with SCI who intended to become active. Research examining the effectiveness of peers promoting physical activity using motivational interviewing has not been conducted in any population.
A crucial first step determining the potential of peer-based motivational interviewing interventions to promote physical activity to people with SCI is to determine the feasibility of peers learning and implementing motivational interviewing-based skills in their practice. In the general population, Castro et al.18 have demonstrated that trained peers can effectively promote physical activity through telephone-based advice as effectively as professional staff. However, the feasibility of peers with a SCI to learn and implement motivational interviewing sessions has not been tested.
Rollnick and Miller13 have stressed that motivational interviewing is not a set of specific techniques but a skilled style of counseling that requires careful training. Typically, motivational interviewing interventions are delivered by individuals with extensive training in psychology or counseling.19 Resnicow et al. suggest that individuals without trained expertise in these fields (i.e. peers) are likely to find motivational interviewing to be a dramatic shift in their skill set and may be unable to apply motivational interviewing without extensive training.19 As community members, who in many cases volunteer their time, it is unlikely that peers have the time or resources to undertake extensive training in motivational interviewing. Furthermore, a systematic review has found that motivational interviewing counseling sessions take an extended period of time to deliver (∼104 minutes per session).16 This prolonged interaction is likely too lengthy for opportunistic interventions to occur in peer settings. To increase the implementation of motivational interviewing in settings with limited time for training and delivery, several researchers have called for examinations of extremely brief adaptations of motivational interviewing that use only a few motivational interviewing techniques with a focus on the spirit of motivational interviewing (i.e. evocation, collaboration, and acceptance of autonomy).16,20
Brief action planning (BAP)
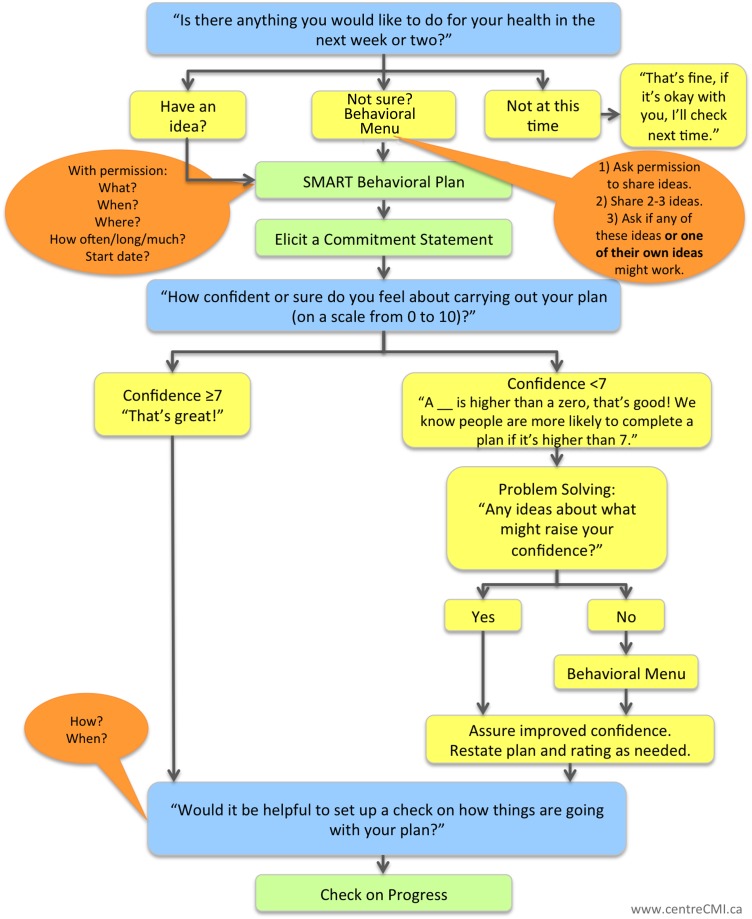
One brief adaption of motivational interviewing style worthy of investigation is BAP. Based on the spirit of motivational interviewing, BAP is a structured, patient centered, self-management support tool.21 It is evidence informed and applies a stepped-care approach to support clients in forming action plans for behavior change (Fig. 1).21 BAP is especially relevant to the SCI population as creating action plans is an effective approach for promoting physical activity to people with SCI.5,6
Figure 1 .
Brief action planning flow chart.
Purpose
The present study aimed to test the feasibility of training peers with SCI to learn BAP. Given that feasibility studies aim to assess parameters preceding the main study (e.g. the impact of BAP on mentees behavior),22 feasibility was assessed in terms of peers' (1) BAP and motivational interviewing spirit competence; (2) training satisfaction; and (3) motivations to use BAP as assessed by measures of the theory of planned behavior constructs.23 Evaluating the impact of the training on mentees, physical activity behavior was beyond the scope of the pilot study. Given the exploratory nature of this pilot study, hypotheses were not put forth.
Method
Participants
Participants were identified and recruited by staff at a community-based organization that offers a volunteer-based peer support program to people with SCI. At the time of the study, there were 278 volunteers in the peer support program; however, peers were only recruited from three of the seven regional offices that have a formal peer support program. Prior to the training, the community-based organization had not offered training in BAP or motivational interviewing to peer volunteers. Participants were required to be at least 18 years old and a volunteer within the organization's peer support program. Due to potential ceiling effects of initial training in motivational interviewing24 and to ensure the training could be tailored to peers who could benefit the most, participants were also required to be perceived by staff as individuals who may be less confident in their skills to promote physical activity to people with SCI. All participants received the training without charge. At the training, participants were provided with lunch and were paid $50 for attending. To limit transportation barriers, participants were reimbursed for the cost of their transportation. The study was approved by Queen's University General Research Ethics Board.
Procedure and design
A one-arm, pre-test, post-test design was used with three assessment periods at baseline (T1), immediately post-training (T2) and follow up (T3). Baseline (T1) and follow up (T3) measures each were completed in two phases. Phase 1 of baseline was completed by phone (∼20–30 minutes) 1–2 weeks before the training and Phase 2 was completed in-person immediately before the training (∼10 minutes). The post-training assessment was completed in person (∼10 minutes). Phase 1 of follow up was completed by phone 1–2 weeks after the training (∼20–30 minutes) and Phase 2 was completed online or by phone 1 month following the training (∼10 minutes). Table 1 describes the measures administered at each time point.
Table 1 .
Measures at each time point
| Time points and measures | Timing | Format |
|---|---|---|
| Baseline: Phase 1 (Time 1) | ||
|
1–2 weeks before the training | Telephone |
| Baseline: Phase 2 (time 1) | ||
|
Immediately before the training | In person |
| Post-training (Time 2) | ||
|
Immediately after the training | In person |
| Follow up: Phase 1 (Time 3) | ||
|
1–2 weeks after the training | Telephone |
| Follow up: Phase 2 (Time 3) | ||
|
1-month following the training | Online/telephone |
A process evaluation was conducted to assess training context and to ensure that the training was delivered as intended. Using audio recordings of the trainings, training time, and the trainers' adherence (yes/no) to each aspect of the protocol were assessed. Table 2 depicts the topics covered by the trainer and the results of the process evaluation. Overall, results of the process evaluation indicated that the training was delivered consistently across the three regional areas of the community-based organization.
Table 2 .
Results of process evaluation
| Theoretical construct | Service area 1 |
Service area 2 |
Service area 3 |
||||
|---|---|---|---|---|---|---|---|
| Number of participants | 8 | 2 | 3 | ||||
| Total time | 3 hours, 46 minutes | 3 hours, 33 minutes | 3 hours, 24 minutes | ||||
| Didactic presentation | |||||||
| Time | 44 minutes | 41 minutes | 45 minutes | ||||
| Training objectives | Knowledge | ✓ | ✓ | ✓ | |||
| Benefits of physical activity for people with SCI | Attitudes | ✓ | ✓ | ✓ | |||
| Physical activity guidelines for people with SCI | Attitudes | ✓ | ✓ | ✓ | |||
| The importance of planning | Attitudes | ✓ | ✓ | ✓ | |||
| Introduction to BAP | Knowledge | ✓ | ✓ | ✓ | |||
| BAP definition | Knowledge | ✓ | ✓ | ✓ | |||
| Spirit of motivational interviewing | Knowledge | ✓ | ✓ | ✓ | |||
| Introduction of core skills | Knowledge | ✓ | ✓ | ✓ | |||
| Benefits of BAP | Attitudes | ✓ | ✓ | ✓ | |||
| Recommendations for BAP | Subjective norms | ✓ | ✓ | ✓ | |||
| Practice and feedback | |||||||
| Time | 3 hours 2 minutes | 2 hours, 52 minutes | 2 hours, 39 minutes | ||||
| Audio | Practice | Audio | Practice | Audio | Practice | ||
| Question 1 | PBC | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Skill 1: Behavioral menu | PBC | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Skill 2: SMART goals | PBC | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Skill 3: Elicit commitment | PBC | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Question 2 | PBC | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Question 3 | PBC | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Skill 4: Problem solving | PBC | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Skill 5: Follow up | PBC | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ |
| Full practice (twice) | PBC | ✓✓ | ✓✓ | ✓✓ | ✓✓ | ✓✓ | ✓✓ |
Note. PBC, perceived behavioral control; ✓, the trainer completed the task; ✗, the trainer demonstrated the skill rather than playing the audio recording.
Intervention: BAP training
The training was developed through a partnership between three groups: (1) a group of researchers and community members who aim to promote physical activity to people with SCI (SCI Action Canada); (2) the developers of BAP (Centre for Collaboration, Motivation and Innovation); and (3) a community-based organization that offers the volunteer-based peer support program for people with SCI (SCI Ontario). The aim of the training was to teach peers BAP. This entailed teaching peers the three core questions of BAP; the five skills of BAP; and the spirit of motivational interviewing.
Three trainings were offered within three regional areas of the community-based organization. All trainings were conducted by the first author who is trained in both motivational interviewing and certified as a BAP trainer. The training entailed a half-day (4 hours) workshop. It began with a 1-hour didactic presentation about BAP and was followed by 3 hours of practice with coaching/instruction as well as audio recordings of a peer with SCI using BAP to promote physical activity to a mentee. The training was structured according to Miller and Rollnick's13 motivational interviewing training recommendations and was tailored to the needs of peers with SCI. It also was designed to present information in a way that would motivate peers to use BAP by targeting the constructs of the theory of planned behavior (Table 2).23 The theory of planned behavior was chosen as the guiding theoretical framework as it has been shown to be a determinant of health professionals' behavior in a variety of contexts including counseling.25
All participants were given a BAP manual. The manual included a copy of the BAP flowchart, a BAP step-by-step guide, transcripts of the BAP audio recordings, and copies of the slides used in the didactic presentations.
Measures
Demographics
Participants indicated their sex; age; date, cause and level of SCI; primary mode of mobility outside their home; whether or not they had a cognitive or memory impairment; and their physical activity behavior. The Leisure Time Physical Activity Questionnaire for People with Spinal Cord Injury (LTPAQ-SCI) was modified to assess participation and aerobic and strengthening physical activity during the last 7 days (minutes/week).26 The LTPAQ-SCI is reliable and valid.26
BAP and motivational interviewing spirit competence
Audio recordings
Participants completed a 15-minute audio-taped sample of their physical activity counseling style with a standardized simulated actor who played an individual with a SCI. The actor was certified in BAP and was trained to portray a person with SCI who was interested in adopting the physical activity guidelines for people with SCI by becoming more physically active. The same actor was used in each simulation. Audio recordings were coded using an adapted version of the treatment integrity measure used to certify practitioners in BAP. This measure is informed by the Motivational Interviewing Treatment Integrity scale which has been shown to be reliable and sensitive to detecting improvement in clinical practice as a result of training.27
Coders listened to the audio recordings once and scored participants on three components: spirit of motivational interviewing, BAP skills, and overall call quality. To evaluate adherence to the spirit of motivational interviewing, the coder assigned a single rating from a five-point scale (1 = not present; 2 = inadequate; 3 = adequate; 4 = good; and 5 = excellent) to characterize the entire interaction for each of three spirits of motivational interviewing (i.e. evocation, collaboration, and acceptance of autonomy). To determine the BAP skills score, the coder assigned a single rating to (1 = not present to 5 = excellent) to characterize each of the BAP skills: (1) question 1; (2) presentation of behavioral menu; (3) SMART behavioral plan; (4) elicitation of commitment statement; (5) question 2; (6) problem solving; and (7) follow up. Call quality assessed the peers overall ability to follow the structure of BAP and was assessed using one item rated on a five-point scale (1 = poor; 2 = inadequate; 3 = adequate; 4 = good; and 5 = excellent). Certification standards for BAP require participants to score a three or higher on all items. Coders were blinded to whether audio recordings were completed pre- or post-training.
To achieve inter-rater reliability, both coders assessed 21% of the recordings (n = 6) using the treatment integrity measure. The initial inter-rater reliability was κ = 0.50. Coders discussed their discrepancies, clarified definitions and then coded six additional recordings. Acceptable inter-rater reliability was achieved (κ = 0.77). The remainder of the recordings was divided among each coder and was assessed independently.
Training satisfaction
Participants rated their satisfaction with the training (six items) on a seven-point Likert scale (Table 2).
Listening and motivational interviewing skills
Participants' proficiency in listening skills and motivational interviewing was assessed using an eight-item self-report questionnaire adapted from Miller and Mount.28 Items are rated on a 10-point scale. Specific items and end points are described in Table 3.
Table 3 .
Training satisfaction
| Item | N | Min | Max | Mean | SD |
|---|---|---|---|---|---|
| 1. I am satisfied with the format of the BAP training session | 13 | 6.00 | 7.00 | 6.46 | 0.52 |
| 2. I found the BAP training session to be applicable to my role as a peer support volunteer | 13 | 6.00 | 7.00 | 6.69 | 0.48 |
| 3. I am satisfied with the trainer who conducted the BAP training session | 13 | 6.00 | 7.00 | 6.77 | 0.44 |
| 4. I am satisfied my overall experience at the BAP training session | 13 | 6.00 | 7.00 | 6.77 | 0.44 |
| 5. The balance between presentations, discussion and activities fit my style of learning | 13 | 5.00 | 7.00 | 6.69 | 0.63 |
| 6. I would recommend this training to other peer support volunteers | 13 | 5.00 | 7.00 | 6.62 | 0.65 |
Motivation to use of BAP
Theory of planned behavior questionnaire
Constructed according to recommendations by Francis et al.,29 the questionnaire consists of four scales assessing participants' attitudes, subjective norms, perceived behavioral control, and intentions toward using BAP to promote physical activity to mentees. All items are rated on a seven-point scale. The face validity of the questionnaire was assessed by a member of the CBO's administrative staff, a peer support volunteer, and a team of researchers with expertise in the theory of planned behavior. The attitude scale consisted of five items beginning with the stem, “Using BAP to promote physical activity to my mentees would be … ” and rated on a semantic differential scale (bad/good; harmful/beneficial; foolish/wise; worthless/useful; unpleasant/pleasant) (Chronbach's αT1 = 0.96; Chronbach's αT2 = 0.59; and Chronbach's αT3 = 0.87). The subjective norms scale consisted of three items rated on a Likert scale (Chronbach's αT1 = 0.99; Chronbach's αT2 = 0.57; and Chronbach's αT3 = 0.78): (1) “Most people who are important to me think that I should use BAP to promote physical activity to my mentee”, (2) “People who are important to me want me to use BAP to promote physical activity to my mentee”, and (3) “It is expected of me that I use BAP to promote physical activity to my mentee”. The perceived behavioral control scale consisted of five items (Chronbach's αT1 = 0.27; Chronbach's αT2 = 0.55; and Chronbach's αT3 = 0.73). Three items assessed participants' confidence to use BAP: (1) “Using BAP to promote physical activity to my mentee would be … (difficulty; easy)”, (2) “I am confident that I can use BAP to promote physical activity to my mentees (strongly disagree; strongly agree)”, and (3) “How confident are you in your ability to effectively use BAP to promote physical activity to your mentees if you wanted to do so?” (not confident at all; completely confident). Two items rated on a Likert scale assessed participants' belief in their control over their behavior: (1) “The decision to use BAP to promote physical activity to my mentees is beyond my control”, and (2) “Whether I use BAP to promote physical activity to my mentees is entirely up to me”. The intention scale consisted of three items rated on a Likert scale (Chronbach's αT1 = 0.93; Chronbach's αT2 = 0.65; and Chronbach's αT3 = 0.69): (1) “I intend to use BAP to promote physical activity to my mentees”, (2) “I expect to use BAP to promote physical activity to my mentees”, and (3) “I want to use BAP to promote physical activity to my mentees”. To assess behavior, participants indicated whether or not they had a peer interaction since the training. If participants had an interaction, they indicated whether or not they had used BAP to promote physical activity in the interaction.
Analysis
Internal consistency of the items used to assess the theory of planned behavior constructs was assessed by computing Cronbach's alphas at each time point. Results of Shapiro–Wilk tests of normality revealed that two listening and motivational interviewing skills items (i.e. items 2 and 8) as well as the attitudes, subjective norms, and intentions total scores were not normally distributed at baseline (P's < 0.05). Logarithmic and square-root transformations did not improve data distribution (Shapiro–Wilk tests of normality, P's < 0.05). Given the robustness of the ANOVA test to violations of normality, repeated measures analyses of variance (RM-ANOVAs) were conducted to analyze changes in participants' BAP and motivational interviewing spirit skills, and motivation to use BAP,30 significance was set at P < 0.05. Cohen's d was calculated to determine the size of effects. Effect sizes of 0.20, 0.50, and 0.80 were considered small, medium, and large effects respectively.31
Results
Study sample
In total, 16 participants were recruited to attend the training and completed the initial audio recording. Three participants were unable to attend the training due to illness and transportation barriers. In total, 13 participants (54% male; Mage = 52.77 ± 9.16 years) attended the training. Participants had been injured for an average of 18.46 ± 14.51 years, 54% were individuals with tetraplegia and the majority used a wheelchair as their primary mode of mobility (46% manual wheelchair; 30% power wheelchair; 15% cane; 8% walked independently). The majority of participants had completed a college degree (23% high school; 39% college; 15% university; 23% post-graduate degree) and 15% of participants indicated that they had a cognitive or memory impairment. Participants had been peer support volunteers for an average of 4.33 ± 3.16 years and had mentored an average of 6.08 ± 6.29 mentees. Two participants (15%) indicated having had experience using motivational interviewing or BAP. All participants who attended the training completed the measures at all time points. At baseline, participants engaged in 130.15 ± 165.26 minutes of aerobic LTPA and 44.80 ± 37.33 minutes of strengthening LTPA during the last 7 days.
BAP and motivational interviewing spirit competence
Audio recordings
Ratings of participants' BAP skills, spirit of motivational interviewing, and overall call quality significantly increased between baseline and follow up (P's < 0.05, d's > 2.27) (Table 4). Only one participant reached a level of competence appropriate for BAP certification.
Table 4 .
BAP and motivational interviewing spirit competence and theory of planned behavior construct scores
| Means and standard deviations |
RM-ANOVAs |
Bonferonni comparisons |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Items | Baseline (T1) | Post-training (T2) | Follow up (T3) | F | df | P | T1 vs. T2 |
T1 vs. T3 |
T2 vs. T3 |
|||
| P | d | P | d | P | d | |||||||
| Listening and motivational interviewing skills | ||||||||||||
| 1. I am a skillful, good listener is working with my matches | 7.31 ± 1.65a | 8.53 ± 0.97b | 8.46 ± 0.88ab | 4.23 | 2, 11 | 0.04 | 0.03 | 0.90 | 0.08 | 0.87 | 1.00 | 0.07 |
| 2. I think the most effective way to motivate matches to engage in physical activity is … . (pressure/internal motivation) | 8.38 ± 1.61a | 9.38 ± 0.96a | 9.08 ± 1.26a | 1.63 | 2, 11 | 0.24 | 0.25 | 0.75 | 0.54 | 0.48 | 1.00 | 0.26 |
| 3. I have the ability to increase my matches' motivation when they are not initially motivated to be physically active | 6.54 ± 1.94a | 8.31 ± 1.18b | 7.78 ± 1.83ab | 6.01 | 2, 11 | 0.01 | 0.01 | 1.10 | 0.12 | 0.66 | 0.33 | 0.34 |
| 4. I understand the basic ideas and principles of BAP | 7.23 ± 2.01a | 9.16 ± 0.55b | 9.00 ± 1.00ab | 6.89 | 2, 11 | 0.01 | 0.01 | 1.31 | 0.07 | 1.11 | 1.00 | 0.20 |
| 5. I feel capable and able to apply BAP in general | 6.23 ± 1.96a | 8.77 ± 0.93b | 8.46 ± 1.20b | 12.82 | 2, 11 | 0.001 | 0.002 | 1.66 | 0.03 | 1.37 | 0.79 | 0.29 |
| 6. I feel capable of using BAP in my role as a peer support volunteer | 7.08 ± 2.11a | 9.25 ± 0.87b | 8.75 ± 1.21b | 7.54 | 2, 11 | 0.01 | 0.006 | 1.34 | 0.02 | 0.97 | 0.33 | 0.47 |
| 7. I am confident in my ability to increase my matches' motivation to engage in physical activity | 7.31 ± 1.55a | 8.54 ± 0.97a | 8.38 ± 1.04a | 3.00 | 2, 11 | 0.09 | 0.09 | 0.95 | 0.25 | 0.81 | 1.00 | 0.16 |
| 8. I have the desire to learn more about how to do BAP | 9.31 ± 1.03a | 8.85 ± 1.14a | 7.69 ± 1.97b | 4.19 | 2, 11 | 0.04 | 0.41 | 0.42 | 0.04 | 1.03 | 0.03 | 0.72 |
| Theory of planned behavior | ||||||||||||
| Attitudes | 32.85 ± 3.50a | 34.00 ± 1.35a | 33.46 ± 2.40a | 0.92 | 2, 11 | 0.43 | 0.55 | 0.43 | 0.91 | 0.20 | 0.98 | 0.28 |
| Perceived behavioral control | 26.46 ± 3.43a | 30.00 ± 4.28b | 29.46 ± 4.33ab | 3.91 | 2,11 | 0.05 | 0.04 | 0.91 | 0.20 | 0.77 | 1.00 | 0.13 |
| Subjective norms | 16.67 ± 5.21a | 18.42 ± 2.50a | 16.67 ± 3.20a | 1.12 | 2,10 | 0.36 | 0.80 | 0.43 | 1.00 | 0.00 | 0.44 | 0.61 |
| Intentions | 17.61 ± 3.71a | 19.84 ± 1.28a | 18.53 ± 2.30a | 3.95 | 2.11 | 0.05 | 0.20 | 0.80 | 1.00 | 0.30 | 0.22 | 0.80 |
| Audio recordings | ||||||||||||
| BAP skills | 11.15 ± 1.14a | – | 21.31 ± 3.68b | 77.44 | 1,12 | <0.001 | – | – | <0.001 | 3.73 | – | – |
| Spirit of motivational interviewing | 8.15 ± 1.34a | – | 10.38 ± 1.12b | 20.27 | 1,12 | 0.001 | – | – | 0.001 | 4.83 | – | – |
| Call quality | 1.15 ± 0.38a | – | 2.54 ± 0.78b | 32.95 | 1,12 | <0.001 | – | – | <0.001 | 2.27 | – | – |
Note. Columns sharing the same letter are not significantly different whereas those with the different letter are significantly different (P < 0.05).
Listening and motivational interviewing spirit skills
The majority of items (five of eight) assessing participants' skills significantly increased post-training and were maintained at follow up or decreased slightly such that they were not significantly different than baseline or post-training (P's < 0.05). There was no change (P > 0.05) in participants' (1) perceptions that the most effective way to motivate clients was through internal motivation; and (2) confidence in their ability to increase their clients' motivation to engage in physical activity. Participants' desire to learn more about BAP significantly decreased at follow up (Table 4).
Training satisfaction
Participants' responses to the training satisfaction questionnaire were very positive with all means falling above the scale midpoint and ranging from 6.46 to 6.77 on a seven-point scale (Table 3).
Motivation to use of BAP
Participants' perceived behavioral control to use BAP increased from baseline to post and decreased at follow up such that no significant differences were observed between follow up and baseline or post. Although the RM-ANOVA assessing participants' intention to use BAP was significant, pairwise comparisons did not reveal significant differences between time points. Likewise, significant changes in participants' attitudes and subjective norms were not observed (Table 4). At follow up, because none of the participants had a peer interaction since the training, none had used BAP.
Discussion
The present study examined the feasibility of training peers with SCI to learn BAP to promote physical activity to mentees with SCI. In particular, we examined the feasibility of training peers who were identified as less confident in promoting physical activity to mentees. Significant increases were observed in the majority of self-reported listening and motivational interviewing spirit skills and ratings of participants' audio recordings following the training. Regarding training satisfaction, findings indicate the training was well received by the peers. Findings assessing participants' motivation to use BAP to promote physical activity to mentees were mixed. Peers' attitudes, subjective norms, and intentions toward using BAP were already very positive to start and did not change following the training. Conversely, increases in participants' perceived behavioral control to use BAP were observed after the training but were not maintained at follow up. Overall, findings provide preliminary indication that training peers with SCI to learn BAP to promote physical activity to mentees is feasible.
Our findings demonstrate that a short training program can increase peers' BAP and motivational interviewing skills. However, ratings of participants' final audio calls highlight the need for further practice and feedback following training. While final ratings of audio calls significantly increased from baseline, only one participant reached a level of practice that was deemed acceptable for certification in BAP. Furthermore, initial changes in participants' perceived behavioral control were not maintained at follow up. Research examining the training of health professionals to use motivational interviewing has indicated that workshops may increase knowledge but not necessarily skill.32,33 Furthermore, if gains in motivational interviewing skills are observed, they do not always endure post-training.34 Therefore, it had been recommended that motivational interviewing trainings be supplemented with coaching and feedback for trainees.32,33 In spite of the reduced number of skills needed for BAP compared to motivational interviewing, our results indicate that future trainings should incorporate opportunities for individuals to receive additional coaching and feedback. There may be value in conducting these trainings through mediated forms of communication as these have been identified as preferred communication channels in the SCI population.11
The current study findings also suggest value in tailoring training content to the unique role of trainees. Peers' high satisfaction with the training is likely attributed to the care taken to tailor each aspect of the training to peers with SCI. Constituent input and tailored training goals are key elements of successful dissemination of evidence-based practice.35 By developing the trainings in the context of a multidisciplinary partnership, appropriate expertise was leveraged to ensure that both the BAP tool, questionnaires and the training best met the needs of peers with SCI.36
The trainings were likely also strengthened by targeting each of the constructs of the theory of planned behavior.37 While calls have been issued for greater integration of theory in motivational interviewing training,38 to our knowledge, this is the first training study in the motivational interviewing literature to target constructs of a behavior change theory to encourage evidence-based practice. This theory-based content likely lead to initial increases in participants' perceived behavioral control to use BAP. Conversely, the lack of change observed in participants' attitudes, subjective norms, and intentions toward using BAP are likely due to ceiling effects. Participants in the present study were recruited by the community-based organization and were motivated to attend. The recruitment techniques and participants' willingness to learn and use BAP may have led to participants' initial and consistently high positive attitudes, subjective norms, and intentions. Nevertheless, participants, perceived behavioral control to use BAP did decrease at follow up. This decrease may be attributed to participants' lack of opportunity to apply their skills and practice. Follow-up coaching and feedback efforts should not only aim to encourage skill development but should also maintain confidence among trainees by continuing to target individuals' perceived behavioral control to use BAP.
Some limitations of our feasibility study should be mentioned and addressed. Owing to the short-term and exploratory nature of our study, our evaluation period was not long enough to assess the long-term impact of the training. Findings may have been affected by our study sample. In particular, volunteers are typically highly motivated individuals who are more willing to volunteer in a research study and learn a new approach.32 Site-level differences and staff's potentially differing perceptions of what constitutes a peer counselor who may be less confident in his or her skills to promote physical activity to people with SCI may have also affected our study sample. Furthermore, our findings may have been affected by our measures. In particular, we could only assess the face validity of the theory of planned behavior questionnaire and not the test–retest reliability of the questionnaire. However, our questionnaire adheres to the principles of measuring theory of planned behavior constructs.29,39 Finally, due to the exploratory nature of our study and the challenges of recruiting peers we did not have a comparison group; this prevented contrast with other training methods.
Despite these limitations, the study design has a number of strengths. Typically, motivational interviewing training studies only evaluate one or two training outcomes; rely on either self-reported measures or audio calls (i.e. not both); and only assess outcomes post-training.38 The design of the present study improves upon previous training studies by evaluating three measures of feasibility; using a combination of self-reported measures and audio calls to assess competence in BAP and motivational interviewing spirit; and assessing outcomes at baseline, post, and follow up. Moreover, this is the first study to examine the feasibility of peers, let alone peers with SCI, learning and implementing any form of motivational interviewing.
Conclusion
Results of the present study indicate that training peers with SCI to learn BAP to promote physical activity to mentees is feasible. However, results highlight the need for further coaching and feedback to achieve acceptable levels of evidence-based practice. Peers' high satisfaction with the trainings is likely attributed to the multidisciplinary partnership approach used to develop the trainings. In the future, researchers aiming to train peers to promote physical activity should consider establishing a multidisciplinary partnership to develop training content that is tailored to the needs and roles of peers. Further research is needed to determine the impact of training on peers' evidence-based practices and mentees' physical activity behavior.
Acknowledgements
The authors would like to acknowledge SCI Ontario staff for their assistance in organizing and facilitating the trainings. The authors would also like to thank Anam Imtiaz who was the standardized actor for all audio-taped samples, Lori Godin for her assistance in coding the audio recordings and the peer volunteers who participated in the training and study.
Disclaimer statements
Contributors All authors made a substantial contribution to the concept and design; acquisition of data; analysis; and/or interpretation of data. All authors drafted the article or revised it critically for important intellectual content. All authors approved the version to be published.
Funding Research supported by a Community-University Research Alliance grant from SSHRC. Research team members supported by a Mentor-Trainee Award from the Ontario Neurotrauma Foundation (KAMG and AEL), the Canada Research Chair (CIHR) program (AEL) and a CIHR Canada Graduate Scholarship (HLG).
Conflicts of interest Connie Davis is a paid consultant for the Centre for Collaboration, Motivation and Innovation and Sheila Casemore is a salaried employee of SCI Ontario.
Ethics approval This study was approved by the Queen's University General Research Ethics Board.
References
- 1.Rimmer J, Braddock D. Health promotion for people with physical, cognitive, and sensory disabilities: an emerging national priority. Am J Health Promot 2002;16(4):220–4. [DOI] [PubMed] [Google Scholar]
- 2.Martin Ginis KA, Latimer AE, Arbour-Nicitopoulos KP, Buchholz AC, Bray SR, Craven BC, et al. Leisure time physical activity in a population-based sample of people with spinal cord injury part I: demographic and injury-related correlates. Arch Phys Med Rehabil 2010;91(5):722–8. [DOI] [PubMed] [Google Scholar]
- 3.Wolfe DL, McIntyre A, Ravenek K, Martin Ginis KA, Latimer-Cheung AE, Eng J, et al. Physical activity and SCI. In: Eng J, Teasell R, Miller W, Wolfe D, Townson A, Hsieh J, et al. (eds.) Spinal cord injury rehabilitation evidence. 4th ed 2013. Available at http://www.scireproject.com/rehabilitation-evidence/physical-activity. [Google Scholar]
- 4.SCI Action Canada. SCI Action Canada website 2011 [2011 Jun 6]. Available from: http://www.sciactioncanada.ca/.
- 5.Latimer AE, Martin Ginis KA, Arbour KP. The efficacy of an implementation intention intervention for promoting physical activity among individuals with spinal cord injury: a randomized controlled trial. Rehabil Psychol 2006;51(4):273–80. [Google Scholar]
- 6.Arbour-Nicitopoulos KP, Ginis KA, Latimer AE. Planning, leisure-time physical activity, and coping self-efficacy in persons with spinal cord injury: a randomized controlled trial. Arch Phys Med Rehabil 2009;90(12):2003–11. [DOI] [PubMed] [Google Scholar]
- 7.Bassett RL, Martin Ginis KA. Risky business: the effects of an individualized health information intervention on health risk perceptions and leisure time physical activity among people with spinal cord injury. Disabil Health J 2011;4(3):165–76. [DOI] [PubMed] [Google Scholar]
- 8.Gainforth HL, Latimer-Cheung AE, Athanasopoulos P, Martin Ginis KA. Examining the effectiveness of an event-based knowledge translation initiative for disseminating the physical activity guidelines for people with spinal cord injury. Disabil Health J 2013;6(3):260–5. [DOI] [PubMed] [Google Scholar]
- 9.SCI Ontario. Peer support 2012 [2012 Jun 22]. Available from: http://www.cpaont.org/service/peer-support.
- 10.Letts L, Ginis KA, Faulkner G, Colquhoun H, Levac D, Gorczynski P. Preferred methods and messengers for delivering physical activity information to people with spinal cord injury: a focus group study. Rehabil Psychol 2011;56(2):128–37. [DOI] [PubMed] [Google Scholar]
- 11.Faulkner G, Gorczynski P, Arbour KP, Letts L, Wolfe DL, Martin Ginis KA. Messengers and method of disseminating health information among individuals with spinal cord injury: a scoping review. In: Berkovsky T. (ed.) Hanbook of spinal cord injuries. Nova Science Publishers; 2010. pp. 349–74. [Google Scholar]
- 12.Ginis KA, Nigg CR, Smith AL. Peer-delivered physical activity interventions: an overlooked opportunity for physical activity promotion. Transl Behav Med 2013;3(4):434–43. doi:10.1007/s13142-013-0215-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miller WR, Rollnick S. Motivational interviewing: preparing people for change. New York: The Guilford Press; 2002. [Google Scholar]
- 14.Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: a meta-analysis of controlled clinical trials. J Consult Clin Psychol 2003;71(5):843–61. [DOI] [PubMed] [Google Scholar]
- 15.Rubak S, Sandbæk A, Lauritzen T, Christensen B. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract 2005;55(513):305–12. [PMC free article] [PubMed] [Google Scholar]
- 16.Dunn C, Deroo L, Rivara F. The use of brief interventions adapted from motivational interviewing across behavioral domains: a systematic review. Addiction 2002;96(12):1725–42. [DOI] [PubMed] [Google Scholar]
- 17.Latimer-Cheung AE, Arbour-Nicitopoulos KP, Brawley LR, Gray C, Justine Wilson A, Prapavessis H, et al. Developing physical activity interventions for adults with spinal cord injury. Part 2: motivational counseling and peer-mediated interventions for people intending to be active . Rehabil Psychol 2013;58(3):307–15. [DOI] [PubMed] [Google Scholar]
- 18.Castro CM, Pruitt LA, Buman MP, King AC. Physical activity program delivery by professionals versus volunteers: the TEAM randomized trial. Health Psychol 2011;30(3):285–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Resnicow K, DiIorio C, Soet JE, Borrelli B, Hecht J, Ernst D. Motivational interviewing in health promotion: it sounds like something is changing. Health Psychol 2002;21(5):444–51. [PubMed] [Google Scholar]
- 20.Rollnick S. Behaviour change in practice: targeting individuals. Int J Obes Relat Metab Disord 1996;20(Suppl 1):S22–6. [PubMed] [Google Scholar]
- 21.Gutnick D, Reims K, Davis C, Gainforth H, Jay M, Cole S. Brief action planning to facilitate behavior change and support patient self-management. J Clin Outcomes Manag 2014;21(1). [Google Scholar]
- 22.Arain M, Campbell MJ, Cooper CL, Lancaster GA. What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Med Res Methodol 2010;10:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process 1991;50:179–211. [Google Scholar]
- 24.Baer JS, Wells EA, Rosengren DB, Hartzler B, Beadnell B, Dunn C. Agency context and tailored training in technology transfer: a pilot evaluation of motivational interviewing training for community counselors. J Subst Abuse Treat 2009;37(2):191–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Godin G, Belanger-Gravel A, Eccles M, Grimshaw J. Healthcare professionals' intentions and behaviours: a systematic review of studies based on social cognitive theories. Implement Sci 2008;3: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martin Ginis KA, Phang SH, Latimer AE, Arbour-Nicitopoulos KP. Reliability and validity tests of the leisure time physical activity questionnaire for people with spinal cord injury. Arch Phys Med Rehabil 2012;93(4):677–82. [DOI] [PubMed] [Google Scholar]
- 27.Moyers TB, Martin T, Manuel JK, Hendrickson SM, Miller WR. Assessing competence in the use of motivational interviewing. J Subst Abuse Treat 2005;28(1):19–26. [DOI] [PubMed] [Google Scholar]
- 28.Miller R, Mount K. A small study of training in motivational interviewing: does one workshop change clinician and client behavior. Behav Cogn Psychother 2001;29:457–71. [Google Scholar]
- 29.Francis J, Eccles M, Jonston M, Walker A, Grimshaw J, Foy R, et al. Constructing questionnaires based on the theory of planned behavior: a manual for health services researchers. Quality of life and management of living resources, 2004. Available at http://pages.bangor.ac.uk/~pes004/exercise_psych/downloads/tpb_manual.pdf.
- 30.Fields A. Discovering statistics using SPSS. London: Sage; 2009. [Google Scholar]
- 31.Cohen J. A power primer. Psychol Bull 1992;112(1):155–9. [DOI] [PubMed] [Google Scholar]
- 32.Miller WR, Yahne CE, Moyers TB, Martinez J, Pirritano M. A randomized trial of methods to help clinicians learn motivational interviewing. J Consult Clin Psychol 2004;72(6):1050–62. [DOI] [PubMed] [Google Scholar]
- 33.Miller WR, Rollnick S. Motivational interviewing: helping people change. 3rd ed New York: The Guilford Press; 2013. [Google Scholar]
- 34.Martino S, Brigham GS, Higgins C, Gallon S, Freese TE, Albright LM, et al. Partnerships and pathways of dissemination: the National Institute on Drug Abuse-Substance Abuse and Mental Health Services Administration blending initiative in the clinical trials network. J Subst Abuse Treat 2010;38(Suppl 1):S31–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Simpson D. A conceptual framework for transferring research to practice. J Subst Abuse Treat 2002;22(4):171–82. [DOI] [PubMed] [Google Scholar]
- 36.Martin Ginis KA, Latimer-Cheung A, Corkum S, Ginis S, Anathasopoulos P, Arbour-Nicitopoulos K, et al. A case study of a community-university multidisciplinary partnership approach to increasing physical activity participation among people with spinal cord injury. Transl Behav Med 2012;2(4):516–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Obrusnikova I, Block M, Dillon S. Children's beliefs toward cooperative playing with peers with disabilities in physical education. Adapt Phys Activ Q 2010;27(2):127–42. [DOI] [PubMed] [Google Scholar]
- 38.Soderlund LL, Madson MB, Rubak S, Nilsen P. A systematic review of motivational interviewing training for general health care practitioners. Patient Educ Couns 2011;84(1):16–26. [DOI] [PubMed] [Google Scholar]
- 39.Ajzen I. Construction of a standard questionnaire for the theory of planned behavior. 2002. Available at http://people.umass.edu/aizen/pdf/tpb.measurement.pdf. [accessed 2014 Jun 6].