Abstract
Central quadriceps tendon (CQT) graft has been successfully used as a viable autograft option in cruciate ligament reconstruction of the knee. The prime emphasis in the majority of the literature is given to surgical details of quadriceps graft harvesting and outcome of cruciate ligament reconstruction. There is less discussion about donor site morbidity in CQT graft, and it is less frequent as compared to that in bone patellar tendon bone graft. We report an extremely unusual case of late quadriceps tendon rupture at the donor site following anterior cruciate ligament reconstruction using CQT graft.
Background
Central quadriceps tendon graft (CQTG), with or without patellar bone plug, for cruciate ligament reconstruction, has remained a second choice1–3 until recently, after several authors used it as a primary graft.4–7 The outcome after anterior cruciate ligament (ACL) reconstruction using QTG is similar to that of bone patellar tendon bone (BPTB) and quadrupled hamstring graft (QHG).5 8 9 Extensor mechanism grafts (CQTG, BPTB) are more prone for donor site morbidity as compared to QHG. The literature is abundant with reports of associated sensory loss, kneeling pain, patella fracture and patellar tendon rupture after ACL reconstruction using BPTB graft at the donor site.10–13 Nevertheless, these complications after CQTG harvest appear to be quite low as compared to BPTB.5 8 14 So far, there have been no reports of quadriceps tendon rupture at the donor site following graft harvest. We report an extremely unusual case of late quadriceps tendon rupture at the donor site; this is perhaps the first case reported in the English literature of post-ACL reconstruction surgery using CQTG with patella bone plug.
Case presentation
A 29-year-old man presented to our sports injuries clinic, with a 2-day history of pain and swelling of his right knee and inability to bear weight over his right lower limb. The patient, while alighting from a halted train, had jumped directly onto the ground, missing three steps of the side ladder of the compartment. Following the jump, his right knee buckled and he heard a ‘pop’ within it. The pain was sudden in onset and located mainly over the front of the right knee, directly above the patella. The patient could not immediately stand or bear weight on the affected limb after the incident. Prior to this, the patient had no symptoms concerning the affected knee. The patient gave a history of being operated, 10 years earlier, at a different centre, for bi-cruciate ligament injuries of his left knee, which he had sustained in a road traffic accident. Medical documents from the previous centre revealed that the patient had undergone ACL and posterior cruciate ligament (PCL) reconstruction using CQTG with a patella bone plug from the right side and QHG from the left, for ACL and PCL, respectively. Post ligament reconstruction, he was apparently asymptomatic and could carry out all his daily routine activities. However, he had restrained himself from participating in any sporting activities. The medical and personal history of the patient was normal otherwise.
On examination of the right knee, there was fullness over the suprapatellar pouch and a 10 cm midline vertical scar healed by primary intention over the anterior aspect of the knee, starting at the superior border of the patella and extending proximally (figure 1). Palpation in the suprapatellar region was tender, and a palpable defect was noted in the quadriceps tendon just above the superior border of the patella. The range of motion was limited and painful. The neurovascular status of the limb was intact. Examination of the left knee revealed scars from the arthroscopic portals and the hamstring graft harvest site used for the cruciate ligaments reconstruction. The range of movement was 0–140° and there was grade-I laxity noted for both anterior and posterior drawer in the left knee. His retrospect Lysholm score was 95.
Figure 1.

Clinical photograph of both knees showing the previous healed scar over the right knee indicating harvest site for central quadriceps tendon.
Investigations
Plain X-rays of the right knee revealed no bony injury. MRI revealed that the medial quadriceps tendon was ruptured whereas lateral most fibres were intact (figure 2A–C). MRI axial image also revealed that a patella bone plug was also harvested along with the CQT.
Figure 2.
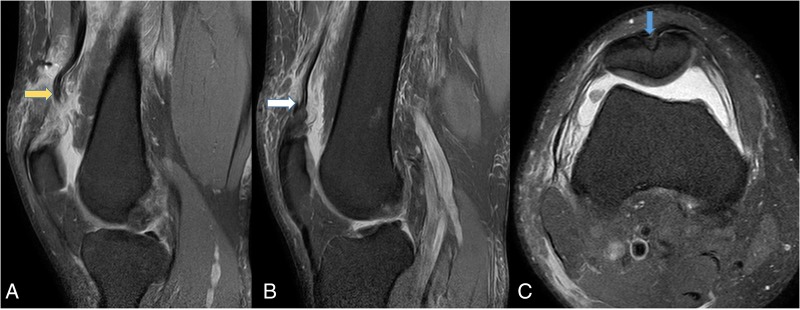
(A) T2 proton density fat saturation MRI of the knee showing (A) medial sagittal image of complete rupture of vastus medialis and vastus intermedius tendon with proximal retraction (yellow arrow). (B) Lateral sagittal image showing intact lateral most fibres of vastus lateralis. (C) Axial image showing a groove over the patella indicating the patella bone plug harvest site (blue arrow).
Treatment
The patient was posted for surgical repair/reconstruction of the right quadriceps tendon. Under spinal anaesthesia and tourniquet control, the defect was approached through an anterior midline incision over the old scar. Donor site exploration revealed rupture of vastus intermedius (VI) and vastus medialis (VM) at the QT-patella upper pole junction. The vastus lateralis (VL) appeared to be intact (figure 3). The donor site defect appeared to be filled with thin fibrous tissue. First, Ultrabraid sutures (Smith and Nephew, Andover, USA) were placed in the ruptured tendons of VI and VM using Bunnell’s technique. Then, three straight transosseous tunnels were drilled in the patella from inferior to superior pole using 1.8 mm Kirshner's wire using an ACL aiming device to accommodate sutures of VI and straight fibres of VM. Then, oblique tunnels were drilled using 1.8 mm Kirshner's wire from the inferolateral border of the patella to the superomedial border to accommodate the sutures of oblique fibres of VM, as VM Obliquus is obliquely inserted on the superomedial border of the patella. The free limbs of sutures through the VI, straight and oblique fibres of VM were passed through the respective tunnels. The sutures were sequentially tied over the bone, keeping the knee in extension. The gap between VL and VM was also loosely closed using absorbable suture material. The wound was then closed in layers over a suction drain, and the knee was kept in extension in a knee immobiliser.
Figure 3.
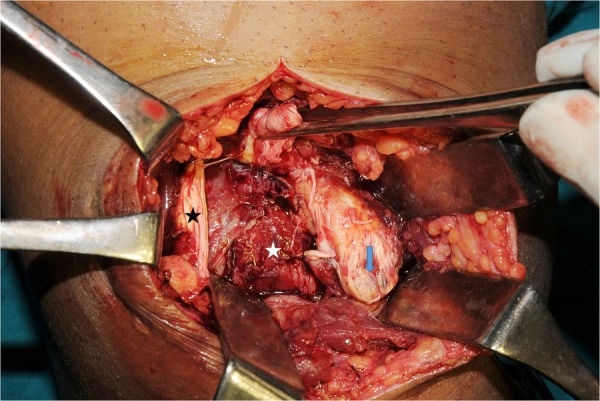
Intraoperative clinical picture showing complete rupture of vastus intermedius (white arrow) and vastus medialis (blue arrow) with intact vastus lateralis fibres (black star). A part of the rectus femoris is held by forceps.
Outcome and follow-up
Postoperatively, the patient was allowed non-weight bearing mobilisation with axillary crutches. Static quadriceps, active straight leg raising and hip abductor strengthening exercises were initiated. At the fifth week, active knee mobilisation was started. The patient regained near normal range of motion by the end of 4 months and was able to perform his routine activities without much difficulty. At his final follow-up, 14 months post surgery, the range of movement was 0–140° without any extensor lag with Lysholm score of 95 (figure 4A, B). Currently, the patient can carry out all his normal activities. However, the patient does not want to participate in any form of sporting activities.
Figure 4.
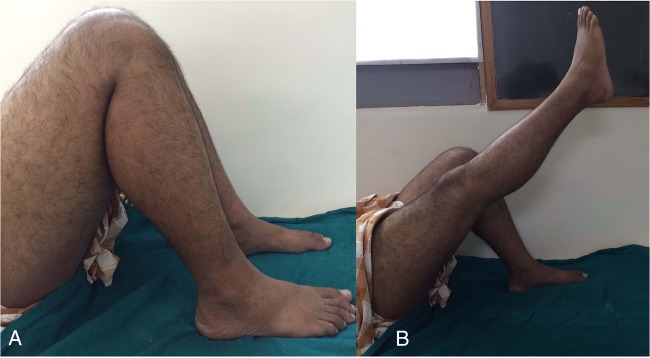
(A) Clinical picture of the index knee demonstrates full flexion. (B) Demonstrates complete knee extension without extensor lag.
Discussion
When considering this case, in particular, the discussion must turn to why this extremely rare complication occurred. To understand this, the biomechanical behaviour of the different grafts must be appreciated.
Currently, BPTB and QHG remain the most popular autograft choice for primary ACL reconstruction because their biomechanical properties are similar to those of native ACL.15 16 The load to failure and cross-sectional area of normal ACL is 1725–2160 N and 44 mm2, respectively. The ultimate tensile strength of autologous CQTG is 2352 N, which exceeds that of native ACL (1725 N), and is similar to that of BPTB graft (2977 N) and QHG (2422 to 4090 N).17 However, in comparison, the cross-sectional area of QTG is 62 mm2, whereas it is only 53 and 35 mm2 in the QHG and BPTB, respectively.17 18 Hence, CQTG provides a thicker graft as compared to QHG and BPTB with the adequate load to failure strength. The CQTG has an obvious advantage in that it has a higher cross-sectional area than the BPTB; both of their strengths are found to be comparable.19 Therefore, the results of ACL reconstruction using BPTB, QHG and CQTG are comparable.5 8 9 16
Both the BPTB and CQTG are comparable in that both the grafts are from the extensor mechanism of the knee. Hence, theoretically, the potential morbidity arising out of donor site may be similar. Nevertheless, BPTB carries a higher incidence of morbidity in terms of anterior knee pain, kneeling pain, patellofemoral arthritis, infrapatellar nerve injury, patella fracture and patella tendon rupture.10–13 16 20 Albeit very rare, patella fracture and patella tendon rupture are disastrous complications after BPTB graft harvest, and can seriously compromise the outcome of ACL reconstruction.10 21 Benner et al reported the incidence of 0.24% of patella tendon rupture in their series of 5364 ACL reconstruction with BPTB graft. In their series, all the patients reported that rupture occurred after their foot hit the ground forcefully in an attempt to prevent further flexion and to keep from falling.10
The potential advantages of free CQTG over BPTB are reduced anterior knee pain, no risk of patella fracture especially when no bone plug is taken along with CQT, no kneeling pain and virtually no risk of injury to infrapatellar branches of the saphenous nerve.8 14 To date, there have been no reports of postharvest quadriceps tendon rupture at the donor site in the literature as compared to BPTB.
It appears that there are certain factors (harvest diameter, live loading conditions and postharvest tissue remodelling at the donor site) that may influence the postoperative strength of the donor site.
After the CQTG or BPTB graft harvest, it would leave a defect in the tendon leading to decrease in the strength of the residual tendon and possibly rupture in the event of significant trauma. Adams et al,22 in their cadaveric study, concluded that, after removal of 10 mm wide strip of QT, the postharvest strength of the residual quadriceps tendon reduces by 34% (3660+830 N to 2430 N). However, postharvest strength is still greater than that of a native patellar tendon (1725–2160N).22 They also concluded that there is 25% reduction in strength of the patellar tendon when a 10 mm wide strip of the patellar tendon is harvested without a bone plug (1920±330 N to 1460 N).22 However, in practice, when coupled with a bone plug of 20×10×8 mm from patella and tibial tuberosity, it may further reduce the strength of the patellar tendon construct and may predispose the tendon rupture at forces less than those established under laboratory conditions. In our patient, it is not known that what diameter of CQTG was previously harvested as the precise intraoperative details of the previous surgery were unavailable. However, our intraoperative findings indicate that, possibly, 9–10 mm of CQTG with patella bone must have been harvested at that point as the majority of VL, VI and VM were intact except the central portion of QT. This would have led to 30–35% reduction in strength at the donor site as discussed above.
Second, the forces over the tendon are different in live loading conditions. In cases of unipedal jump landing on a flexed knee, there is a tendency of the body to have a downward momentum with a force 2–4 times body weight bearing onto the knee during landing.23 To arrest this downward momentum during unipedal jump landings, the quadriceps undergoes lengthening contraction to resist and arrest knee flexion after landing. This lengthening contraction can induce contractile forces in quadriceps in excess of 140% of isometric values.24 25 Withrow et al26 simulated the unipedal jump landing scenario in cadaveric knees to evaluate the contractile forces in the quadriceps at the knee flexion angle of 25° with additional knee flexion of 5–6° during the impact loading from 75 mm. The jumping generates forces ranging from 1022 to 1578 N in the quadriceps, which may exceed the residual strength of the patellar tendon but that fail to exceed those of residual QT.26 This may explain why there is a relatively higher risk of patellar tendon rupture as compared to virtually nil reports of QT rupture.10 12 However, these forces were measured in a cadaveric simulation model ignoring higher knee flexion angles, relative position of torso and other muscle loading patterns, and hence the forces may be greater in live loading conditions, exceeding to those of laboratory values at a donor site.
Our patient jumped from a train compartment and landed on uneven ground; the distance jumped was 4–5 feet. He was not sure whether he landed in a unipedal or bipedal manner. This must have produced a large amount of contractile force onto the postharvest QT leading to rupture of the quadriceps tendon. The force with which he landed on the ground would also be dependent on other factors such as his weight, position of torso, a unipedal or bipedal landing and the horizontal velocity of the jump.
Lastly, another factor that may influence the postharvest strength of donor area is remodelling due to histological changes in the donor area. There is ample evidence in the literature confirming the regeneration of semitendinosus after graft harvest.27–29 However, regardless of morphological regeneration, the regenerated tendon fails to improve the functional deficit in flexion strength and knee flexion torque.27 29 In case of BPTB donor site, the regenerated tissue has ill-defined fascicles and poorly aligned collagen tissue. These abnormal histological findings may persist for up to 27 months and may possess inferior mechanical properties.30–32 Hence, the area remains weak and does not contribute strength to the residual tendon. However, no such histological studies are available for quadriceps tendon in the literature.
Nevertheless, there is a remote possibility that the quadriceps tendon rupture might have resulted anyway, due to extreme eccentric loading force in flexion, and would have happened even if the tendon was normal. We cannot ignore this fact, as the injury occurred 10 years after the graft harvest.
Learning points.
This case illustrates extremely rare ‘late’ donor site morbidity of quadriceps tendon rupture following central quadriceps tendon graft harvest for cruciate ligament reconstruction of the knee.
Despite maintaining comparable strength post-harvest, the residual quadriceps tendon may remain vulnerable to early or late ruptures following trauma.
Graft harvesting must be meticulous, and is probably the most important factor in determining final strength in the native extensor mechanism.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Blauth W. [2-strip substitution-plasty of the anterior cruciate ligament with the quadriceps tendon]. Unfallheilkunde 1984;87:45–51. [PubMed] [Google Scholar]
- 2.Howe JG, Johnson RJ, Kaplan MJ et al. . Anterior cruciate ligament reconstruction using quadriceps patellar tendon graft. Part I. Long-term followup. Am J Sports Med 1991;19:447–57. 10.1177/036354659101900505 [DOI] [PubMed] [Google Scholar]
- 3.Kornblatt I, Warren RF, Wickiewicz TL. Long-term followup of anterior cruciate ligament reconstruction using the quadriceps tendon substitution for chronic anterior cruciate ligament insufficiency. Am J Sports Med 1988;16:444–8. 10.1177/036354658801600503 [DOI] [PubMed] [Google Scholar]
- 4.Akoto R, Hoeher J. Anterior cruciate ligament (ACL) reconstruction with quadriceps tendon autograft and press-fit fixation using an anteromedial portal technique. BMC Musculoskelet Disord 2012;13:161 10.1186/1471-2474-13-161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim SJ, Kumar P, Oh KS. Anterior cruciate ligament reconstruction: autogenous quadriceps tendon-bone compared with bone-patellar tendon-bone grafts at 2-year follow-up. Arthroscopy 2009;25:137–44. 10.1016/j.arthro.2008.09.014 [DOI] [PubMed] [Google Scholar]
- 6.Schulz AP, Lange V, Gille J et al. . Anterior cruciate ligament reconstruction using bone plug-free quadriceps tendon autograft: intermediate-term clinical outcome after 24–36 months. Open Access J Sports Med 2013;4:243–9. 10.2147/OAJSM.S49223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Theut PC, Fulkerson JP, Armour EF et al. . Anterior cruciate ligament reconstruction utilizing central quadriceps free tendon. Orthop Clin North Am 2003;34:31–9. 10.1016/S0030-5898(02)00068-8 [DOI] [PubMed] [Google Scholar]
- 8.Magnussen RA, Carey JL, Spindler KP. Does autograft choice determine intermediate-term outcome of ACL reconstruction? Knee Surg Sports Traumatol Arthrosc 2011;19:462–72. 10.1007/s00167-010-1277-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mulford JS, Hutchinson SE, Hang JR. Outcomes for primary anterior cruciate reconstruction with the quadriceps autograft: a systematic review. Knee Surg Sports Traumatol Arthrosc 2013;21:1882–8. 10.1007/s00167-012-2212-2 [DOI] [PubMed] [Google Scholar]
- 10.Benner RW, Shelbourne KD, Urch SE et al. . Tear patterns, surgical repair, and clinical outcomes of patellar tendon ruptures after anterior cruciate ligament reconstruction with a bone-patellar tendon-bone autograft. Am J Sports Med 2012;40:1834–41. 10.1177/0363546512449815 [DOI] [PubMed] [Google Scholar]
- 11.Ejerhed L, Kartus J, Sernert N et al. . Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction? A prospective randomized study with a two-year follow-up. Am J Sports Med 2003;31:19–25. [DOI] [PubMed] [Google Scholar]
- 12.Ferrer GA, Miller RM, Murawski CD et al. . Quantitative analysis of the patella following the harvest of a quadriceps tendon autograft with a bone block. Knee Surg Sports Traumatol Arthrosc 2015. 10.1007/s00167-015-3550-7 [DOI] [PubMed] [Google Scholar]
- 13.Kartus J, Movin T, Karlsson J. Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts. Arthroscopy 2001;17:971–80. 10.1053/jars.2001.28979 [DOI] [PubMed] [Google Scholar]
- 14.DeAngelis JP, Fulkerson JP. Quadriceps tendon—a reliable alternative for reconstruction of the anterior cruciate ligament. Clin Sports Med 2007;26:587–96. 10.1016/j.csm.2007.06.005 [DOI] [PubMed] [Google Scholar]
- 15.Duquin TR, Wind WM, Fineberg MS et al. . Current trends in anterior cruciate ligament reconstruction. J Knee Surg 2009;22:7–12. 10.1055/s-0030-1247719 [DOI] [PubMed] [Google Scholar]
- 16.Mohtadi NG, Chan DS, Dainty KN et al. . Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev 2011;(9):CD005960 10.1002/14651858.CD005960.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Noyes FR, Butler DL, Grood ES et al. . Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. J Bone Joint Surg Am 1984;66:344–52. [PubMed] [Google Scholar]
- 18.Harris NL, Smith DA, Lamoreaux L et al. . Central quadriceps tendon for anterior cruciate ligament reconstruction. Part I: morphometric and biomechanical evaluation. Am J Sports Med 1997;25:23–8. 10.1177/036354659702500105 [DOI] [PubMed] [Google Scholar]
- 19.Xerogeanes JW, Mitchell PM, Karasev PA et al. . Anatomic and morphological evaluation of the quadriceps tendon using 3-dimensional magnetic resonance imaging reconstruction: applications for anterior cruciate ligament autograft choice and procurement. Am J Sports Med 2013;41:2392–9. 10.1177/0363546513496626 [DOI] [PubMed] [Google Scholar]
- 20.Lidén M, Ejerhed L, Sernert N et al. . Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction: a prospective, randomized study with a 7-year follow-up. Am J Sports Med 2007;35:740–8. 10.1177/0363546506298275 [DOI] [PubMed] [Google Scholar]
- 21.Lee GH, McCulloch P, Cole BJ et al. . The incidence of acute patellar tendon harvest complications for anterior cruciate ligament reconstruction. Arthroscopy 2008;24:162–6. 10.1016/j.arthro.2007.08.020 [DOI] [PubMed] [Google Scholar]
- 22.Adams DJ, Mazzocca AD, Fulkerson JP. Residual strength of the quadriceps versus patellar tendon after harvesting a central free tendon graft. Arthroscopy 2006;22:76–9. 10.1016/j.arthro.2005.10.015 [DOI] [PubMed] [Google Scholar]
- 23.Dufek JS, Bates BT. Biomechanical factors associated with injury during landing in jump sports. Sports Med 1991;12:326–37. 10.2165/00007256-199112050-00005 [DOI] [PubMed] [Google Scholar]
- 24.Pandy MG, Zajac FE, Sim E et al. . An optimal control model for maximum-height human jumping. J Biomech 1990;23:1185–98. 10.1016/0021-9290(90)90376-E [DOI] [PubMed] [Google Scholar]
- 25.Shelburne KB, Pandy MG. A musculoskeletal model of the knee for evaluating ligament forces during isometric contractions. J Biomech 1997;30:163–76. 10.1016/S0021-9290(96)00119-4 [DOI] [PubMed] [Google Scholar]
- 26.Withrow TJ, Huston LJ, Wojtys EM et al. . The relationship between quadriceps muscle force, knee flexion, and anterior cruciate ligament strain in an in vitro simulated jump landing. Am J Sports Med 2006;34:269–74. 10.1177/0363546505280906 [DOI] [PubMed] [Google Scholar]
- 27.Murakami H, Soejima T, Inoue T et al. . Inducement of semitendinosus tendon regeneration to the pes anserinus after its harvest for anterior cruciate ligament reconstruction-a new inducer grafting technique. Sports Med Arthrosc Rehabil Ther Technol 2012;4:17 10.1186/1758-2555-4-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Papandrea P, Vulpiani MC, Ferretti A et al. . Regeneration of the semitendinosus tendon harvested for anterior cruciate ligament reconstruction. Evaluation using ultrasonography. Am J Sports Med 2000;28:556–61. [DOI] [PubMed] [Google Scholar]
- 29.Tadokoro K, Matsui N, Yagi M et al. . Evaluation of hamstring strength and tendon regrowth after harvesting for anterior cruciate ligament reconstruction. Am J Sports Med 2004;32:1644–50. 10.1177/0363546504263152 [DOI] [PubMed] [Google Scholar]
- 30.LaPrade RF, Hamilton CD, Montgomery RD et al. . The reharvested central third of the patellar tendon: a histologic and biomechanical analysis. Am J Sports Med 1997;25:779–85. 10.1177/036354659702500609 [DOI] [PubMed] [Google Scholar]
- 31.Proctor CS, Jackson DW, Simon TM. Characterization of the repair tissue after removal of the central one-third of the patellar ligament. An experimental study in a goat model. J Bone Joint Surg Am 1997;79:997–1006. [DOI] [PubMed] [Google Scholar]
- 32.Sanchis-Alfonso V, Subías-López A, Monteagudo-Castro C et al. . Healing of the patellar tendon donor defect created after central-third patellar tendon autograft harvest. A long-term histological evaluation in the lamb model. Knee Surg Sports Traumatol Arthrosc 1999;7:340–8. 10.1007/s001670050177 [DOI] [PubMed] [Google Scholar]


