Abstract
Foreign body aspiration (FBA) is more common in children than adults with about 80% occurring in children aged less than 15 years. FBA in adults is often overlooked as a potential cause of airway obstruction especially if there is no asphyxiation. We present a case of a 45-year-old male with alcohol abuse who presented with post-obstructive pneumonia secondary to aspiration of tooth of unknown duration. The tooth was removed via flexible bronchoscopy (FBr) and we will discuss the use of FBr for foreign body (FB) removal, which FB can be easily removed by FBr, and the different techniques and devices used for FB removal via FBr.
Keywords: foreign body aspiration in adults, flexible bronchoscopy, post-obstructive pneumonia
Foreign body aspiration (FBA) is more common in children than adults with about 80% occurring in children aged less than 15 years (1). FBA in adults is often overlooked as a potential cause of airway obstruction specially if there is no asphyxiation. However, adults with risk factors such as alcoholism, drug abuse, mental retardation, and neuromuscular conditions are predisposed to aspiration. We present a case of an adult with such risk factors presenting with pneumonia.
Case report
Forty-five-year-old male shelter resident, chronic alcoholic, chronic smoker, and marijuana abuser presented to emergency department (ED) with complaints of intermittent fever with night sweats and productive-cough for 10 days with yellowish sputum associated with pleuritic chest pain. Patient reported a single episode of minimal amount of hemoptysis. He complained of generalized weakness and decreased appetite and claimed to have lost approximately 10 pounds in 2 weeks.
Physical examination including respiratory system was unremarkable. Patient had high grade fever of 102°F and tachycardia of 110–122/min on admission.
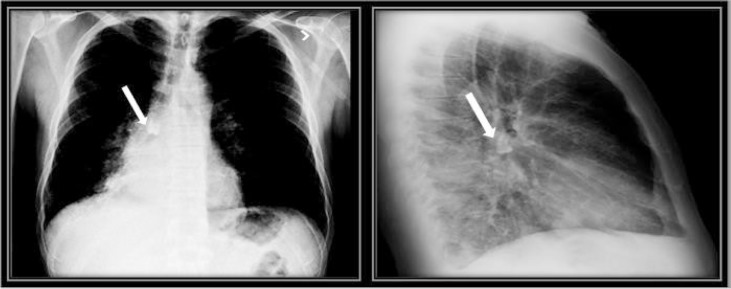
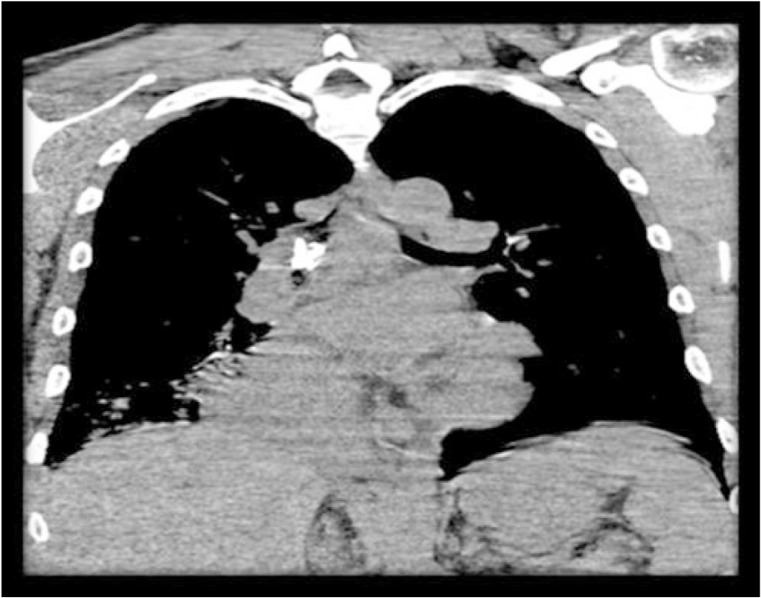
Laboratory results showed leukocytosis of 17,000/mm3 with neutrophil differential of 11,200/mm3 (65%) with band neutrophils of 10%. Comprehensive metabolic panel was normal. Urine toxicology panel was positive for cannabinoids. Chest radiograph was reported as right middle lobe consolidation but careful observation revealed a foreign body (FB), likely a tooth in the right bronchus intermedius (Fig. 1). CT scan of chest showed a well calcified FB likely a tooth at the level of carina obstructing right intermedius bronchus and consolidation in right lower lobe indicating post-obstructive pneumonia (Fig. 2). Patient was admitted and prescribed intravenous antibiotics targeting Gram-negative organisms and anaerobes. His fever subsided within 48 h of starting antibiotics.
Fig. 1.
Tooth in the right bronchus intermedius as seen on chest X-ray.
Fig. 2.
Coronal CT with the aspirated tooth in rat bronchus intermedius.
Bronchoscopy was planned for the removal of FB from the right intermedius bronchus.
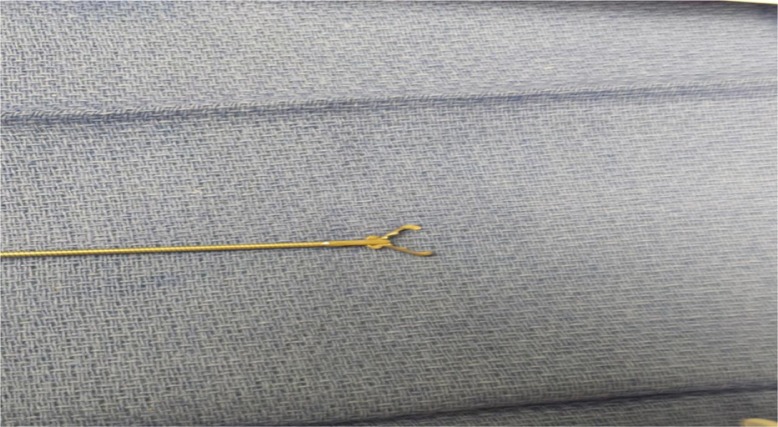
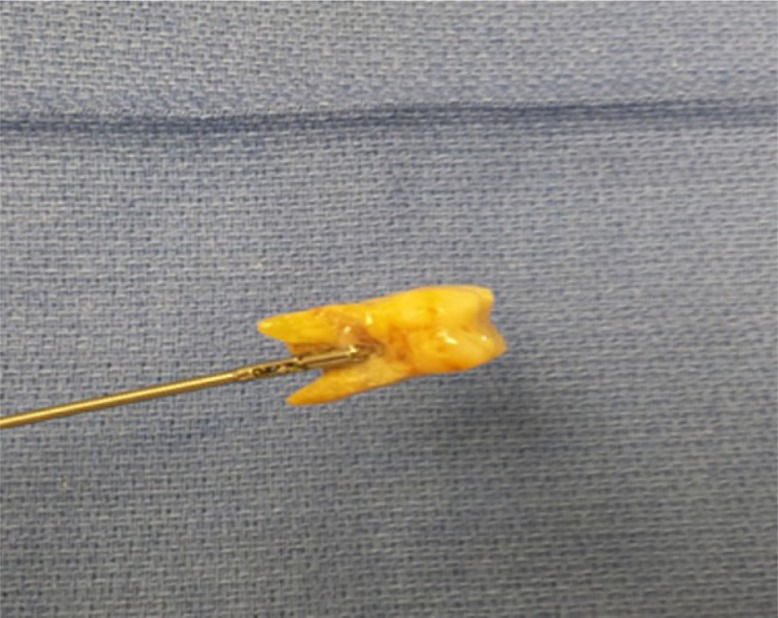
Deep conscious sedation was achieved by propofol infusion in the presence of an anesthesiologist and cardiothoracic surgery backup. Bronchoscopy showed tooth in right intermediate bronchus with ~75% occlusion, and purulent secretions from the right main stem (Figs. 3–6). The FB was removed successfully with rat tooth forceps (Figs. 7 and 8). No significant bleeding was noted at the site of removal. Post bronchoscopy inspection showed right main stem, bronchus intermedius, and right middle and lower lobe bronchi to be well patent. Granulation tissue was noted around previous embedded FB site. Broncho-alveolar lavage was performed, the results of which were negative.
Fig. 7.
Rat tooth forceps.
Fig. 8.
The aspirated tooth removed by rat tooth forceps.
Fig. 3.
Bronchoscopic view of the foreign body visible in the right mainstem bronchus.
Fig. 4.
Closer view of the foreign body, identifiable as tooth in right main stem bronchus.
Fig. 5.
Bronchoscopic view after removal of the tooth.
Fig. 6.
Granulation tissue visible in the right main stem bronchus after removal of the tooth.
Upon further questioning, the patient said that he did not remember having aspirated the tooth and hence the duration of aspiration could not be known. He was discharged home on oral antibiotics a couple of days after the bronchoscopy and counseled to quit alcohol and drugs.
Discussion
FBA is more common in children than adults with about 80% occurring in children aged less than 15 years. It is the fourth most common cause of unintentional injury deaths in the United States. While choking is a hazard for all ages, choking deaths peaked at age 84 in 2011 as per National Safety Council Injury Facts 2015 (1).
FBA in adults is often overlooked as a potential cause of airway obstruction especially if there is no asphyxiation. Adults with risk factors such as alcoholism, drug abuse, mental retardation, and neuromuscular conditions are predisposed to aspiration. However, accidental aspiration in adults without the aforementioned risk factors has been described (2–5). In adults, most common foreign bodies aspirated are food and broken fragments of teeth (6–8).
Chest radiographs are diagnostic of FB in 5–15% of cases (9).
CT scan is more sensitive and specific than chest radiograph in diagnosing radiolucent foreign bodies and for characterizing the attenuation of a suspected FB (9).
Unlike in children, less than half of FBs are lodged in the proximal airways in adults. Most of the FBs are lodged in the right bronchial tree, whereas in children no significant difference was seen between right and left bronchial tree (6).
Bronchoscopy for the removal of FB was introduced by Gustav Killian, an otolaryngologist in 1897. He used rigid bronchoscope for the purpose (10).
Flexible bronchoscopy (FBr) was developed by Shigeto Ikeda in 1968. Animal studies performed by Zavala and Rhodes (11) showed that FBr could be used to retrieve different kinds of FBs by using grasping forceps through the bronchoscope. Since then, it has gained popularity over rigid bronchoscopy.
FBr is considered as the diagnostic test of choice for initial diagnosis of FB in adults. The advantages of FBr over rigid bronchoscopy are that it can be performed under local anesthesia, visualization of smaller peripheral airway is better with relatively easier manipulation, and can be performed in patients with deformities of c-spine and pharynx.
It is also a relatively easy and safer procedure in experienced-hands (10, 12).
Rigid bronchoscopy is recommended if FBr fails, if the FB is centrally located, if firmly embedded in scar tissue, and for removal of sharp objects which require maneuvering to minimize mucosal trauma (13).
There have been several case series which have reported successful removal of foreign bodies by FBr.
Cunanan (12) reported a success rate of 89% in using FBr for the removal of FB in 300 mentally retarded and physically handicapped patients. The population age ranged from 10 years to above 40 years. They reported a decrease in mortality from 12 to 1% with the use of FBr over rigid bronchoscope. They, however, attribute to the increased mortality from rigid bronchoscopy to complications of general anesthesia in patients with comorbidities.
Limper and Prakash had a success rate of 60% with FBr, whereas rigid bronchoscopy showed a success rate of 98%. In their experience, Fbr is advantageous in distally lodged FB, in cases with cervical instability, mechanically ventilated patients, and also in removal of small FBs, which can be securely grasped with a fiberoptic bronchoscope (14).
Lan et al. (15) report a success rate of 97% for FB removal via FBr with low mortality and morbidity. They also reported that granulation tissue can be removed without much bleeding; thus, removal of FB can be achieved in a repeat FBr a week later. None of their cases had massive hemoptysis.
Debeljak et al. (13) indicate that FBr can be used to remove foreign bodies especially if they are small and peripheral and that FBr may be superior to rigid bronchoscopy for grasping tiny and far-reaching foreign bodies. Rigid bronchoscopy is recommended if FBr fails and especially if the FB is large and located in central bronchi or trachea. However, in children who may have central, asphyxiating foreign bodies, the rigid bronchoscope under general anesthesia is preferentially indicated.
Team-based approach with designated roles for team members improves the chances of a successful procedure. Anesthesia and CT surgery backup is essential. Team-based analysis of the nature, location of the FB, and appropriate accessory instruments is equally necessary. Steroids can be given to minimize inflammatory changes as they may lead to difficulty in FB extraction.
Orotracheal approach is preferred over nasotracheal, as it avoids FB from being lost in the nasal passages if accidently dislodged. Care should be taken to keep FB in the center of visual field and to avoid pushing FB distally into the airways. Once FB has been secured, bronchoscope, accessory instrument, and the secured FB are all withdrawn from the airway simultaneously.
Rare complications of FBr are likelihood of asphyxiation from losing the FB in the subglottic area and hemoptysis (10).
If asphyxiation occurs, immediate intubation is needed. Another approach is to reinsert flexible bronchoscope to push the FB into more peripheral airway thus resolving the central airway obstruction.
In case of hemoptysis, airway can be better managed by rigid bronchoscope, but this complication is very rare if performed by trained operators. Incidence of massive hemoptysis even in patients with significant granulation tissue around the FB is extremely low (15).
Organic materials can cause severe inflammation in a short period of time and tend to absorb water with development of airway obstruction relatively earlier. In contrast, inorganic FBs are inert, and so patients might be asymptomatic for a prolonged period (16).
Grasping forceps, baskets, magnet extractors, YAG Laser, and cryoprobes are available as accessories for FB removal via flexible bronchoscope (10).
Rat tooth forceps is a type of a grasping forceps, which is particularly useful for removing hard, flat, or thin organic or inorganic foreign bodies. These are used primarily when the FB is hard as a firm grip can be achieved. These cannot be used for the retrieval of organic friable objects which tend to fracture due to the firmness of the grip provided by these forceps (10).
Zero-tip basket is used in urological procedures like retrieval of ureteral stones. The tipless design allows close approximation to FB. They are used to retrieve FBs lodged in distal bronchi and mobile FBs (16, 17).
Fish net basket, a modified polypectomy snare, is useful in removing bulky FBs (10).
Magnet extractors contain flexible probe tipped with a magnet, useful for retrieval of metallic FBs (10).
FBs embedded in granulation tissue can be removed by YAG Laser, which vaporizes the surrounding granulation tissue. Lasers can also be used to break hard organic FBs (10).
Cryoprobe is used to freeze friable organic and small inorganic materials. Freezing the foreign bodies causes their adherence to the probe thus facilitating the removal (10).
Conclusions
FBA is often overlooked in adults especially if it does not cause asphyxiation. High index of suspicion is needed especially for high-risk patients presenting with compatible symptoms. CT scan is the most sensitive test for diagnosing FB. FBr is the initial diagnostic and therapeutic procedure recommended with low complication rates in experienced hands. Rigid bronchoscopy is performed if the flexible bronchoscopy fails or if the FB is large and centrally located, in case of significant hemoptysis and if significant granulation tissue is present with a FB which is deeply embedded.
Conflict of interest and funding
The authors report no conflict of interest.
References
- 1.National Safety Council. Report on injuries. Injury facts. 2015. Available from: www.nsc.org/library/report injury usa.htm [cited 7 March 2015].
- 2.Qureshi A, Behzadi A. Foreign-body aspiration in an adult. Can J Surg. 2008;51(3):E69. [PMC free article] [PubMed] [Google Scholar]
- 3.Barbera N, Arcifa V, Valenti V, Spadaro G, Tomasello S, Romano G, et al. Fatal asphyxia by complete laryngeal obstruction due to chewing-gum aspiration in an adult woman. Rom J Leg Med. 2012;20:33–6. [Google Scholar]
- 4.Tam T, Weinberg L, Edington J. Airway obstruction from accidental ingestion of a live fish. BMJ Case Rep. 2013;2013:bcr013010486. doi: 10.1136/bcr-2013-010486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pinheiro J, Cordeiro C, Vieira DN. Choking death on a live fish (Dicologoglossa cuneata) Am J Forensic Med Pathol. 2003;24(2):177–8. doi: 10.1097/01.PAF.0000069564.43504.b7. [DOI] [PubMed] [Google Scholar]
- 6.Baharloo F, Veyckemans F, Francis C, Biettlot MP, Rodenstein DO. Tracheobronchial foreign bodies: Presentation and management in children and adults. Chest. 1999;115:1357–62. doi: 10.1378/chest.115.5.1357. [DOI] [PubMed] [Google Scholar]
- 7.Patel S, Kazerooni EA. Case 31: foreign body aspiration, chicken vertebra. Radiology. 2001;218:523–5. doi: 10.1148/radiology.218.2.r01fe49523. [DOI] [PubMed] [Google Scholar]
- 8.Lan R-S. Non-asphyxiating tracheobronchial foreign bodies in adults. Eur Respir J. 1994;7:510–14. doi: 10.1183/09031936.94.07030510. [DOI] [PubMed] [Google Scholar]
- 9.Kim M, Lee KY, Lee KW, Bae KT. MDCT evaluation of foreign bodies and liquid aspiration pneumonia in adults. Am J Roentgenol. 2008;190:907–15. doi: 10.2214/AJR.07.2766. [DOI] [PubMed] [Google Scholar]
- 10.Rafanan AL, Mehta AC. Adult airway foreign body removal. What's new? Clin Chest Med. 2001;22(2):319–30. doi: 10.1016/s0272-5231(05)70046-0. [DOI] [PubMed] [Google Scholar]
- 11.Zavala DC, Rhodes ML. Experimental removal of foreign bodies by fiberoptic bronchoscopy. Am Rev Respir Dis. 1974;110:357–60. doi: 10.1164/arrd.1974.110.3.357. [DOI] [PubMed] [Google Scholar]
- 12.Cunanan OS. The flexible fiberoptic bronchoscope in foreign body removal experience in 300 cases. Chest. 1978;73(Suppl 5):725–6. [PubMed] [Google Scholar]
- 13.Debeljak A, Sorli J, Music E, Kecelj P. Bronchoscopic removal of foreign bodies in adults: experience with 62 patients from 1974–1998. Eur Respir J. 1999;14:792–5. doi: 10.1034/j.1399-3003.1999.14d11.x. [DOI] [PubMed] [Google Scholar]
- 14.Limper AH, Prakash UB. Tracheobronchial foreign bodies in adults. Ann Intern Med. 1990;112(8):604–9. doi: 10.7326/0003-4819-112-8-604. [DOI] [PubMed] [Google Scholar]
- 15.Lan RS, Lee CH, Chiang YC, Wang WJ. Use of fiberoptic bronchoscopy to retrieve bronchial foreign bodies in adults. Am Rev Respir Dis. 1989;140:1734–7. doi: 10.1164/ajrccm/140.6.1734. [DOI] [PubMed] [Google Scholar]
- 16.Freiman MA, McMurray JS. Unique presentation of a bronchial foreign body in an asymptomatic child. Ann Otol Rhinol Laryngol. 2001;110:495–7. doi: 10.1177/000348940111000601. [DOI] [PubMed] [Google Scholar]
- 17.Varshney R, Zawawi F, Shapiro A, Lacroix Y. Use of an endoscopic urology basket to remove bronchial foreign body in the pediatric population. Int J Pediatr Otorhinolaryngol. 2014;78(4):687–9. doi: 10.1016/j.ijporl.2014.01.016. [DOI] [PubMed] [Google Scholar]