Abstract
Wellens’ syndrome, also known as LAD coronary T-wave syndrome or the ‘widow maker’, is a pre-infarction syndrome with non-classical ischemic ECG changes and unremarkable cardiac biomarkers. This syndrome continues to be a ‘can't miss’ for the clinician as delay in urgent angiography and intervention can result in anterior myocardial infarction, left ventricular dysfunction, arrhythmias, and death. We describe a case followed by a discussion of identification criteria and clinical implications.
Keywords: left anterior descending artery, Wellen, anterior myocardial infarction, Ischemia, electrocardiogram, T-wave
A 42-year-old male came to the emergency department (ED) for new onset of chest pain. The chest pain was described as pressure in the left chest, episodic over the prior month, with exertional onset. Two days prior to presentation, the patient had chest pain so unbearable that he fell to his knees. Nausea, emesis, shortness of breath, and diaphoresis accompanied this episode. After 2 hours of rest, the symptoms completely resolved. On the morning of presentation, this same chest pain and symptom constellation returned, and he came immediately by car to the ED. He was asymptomatic by the time of ED evaluation.
The patient denied any previous history of chest pain, hypertension, hyperlipidemia, or arrhythmia. He was a current smoker with a ten-pack-year history and recreational marijuana use. His brother had died suddenly at age 48 from a myocardial infarction (MI) despite a healthy lifestyle and marathon running.
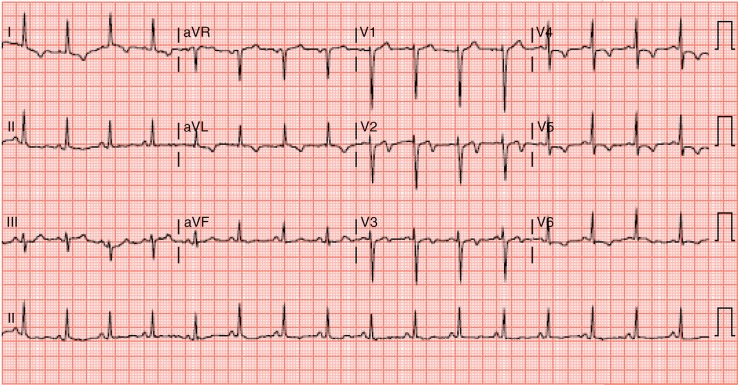
The patient was slightly diaphoretic but in no distress and denied any current chest pain. Vital signs were temperature 96.5°F, pulse 50, blood pressure 146/86, respiration rate 17, and 97% oxygen saturation on room air. Examination revealed regular cardiac rate and rhythm with no extra heart sounds or murmurs, non-displaced PMI, no carotid bruits, +2 pedal pulses with no extremity edema, and clear lungs by auscultation. ECG revealed biphasic T waves in leads V2 and V3 (1, 2) (Fig. 1).
Fig. 1.
Two-lead electrocardiogram of the patient at presentation.
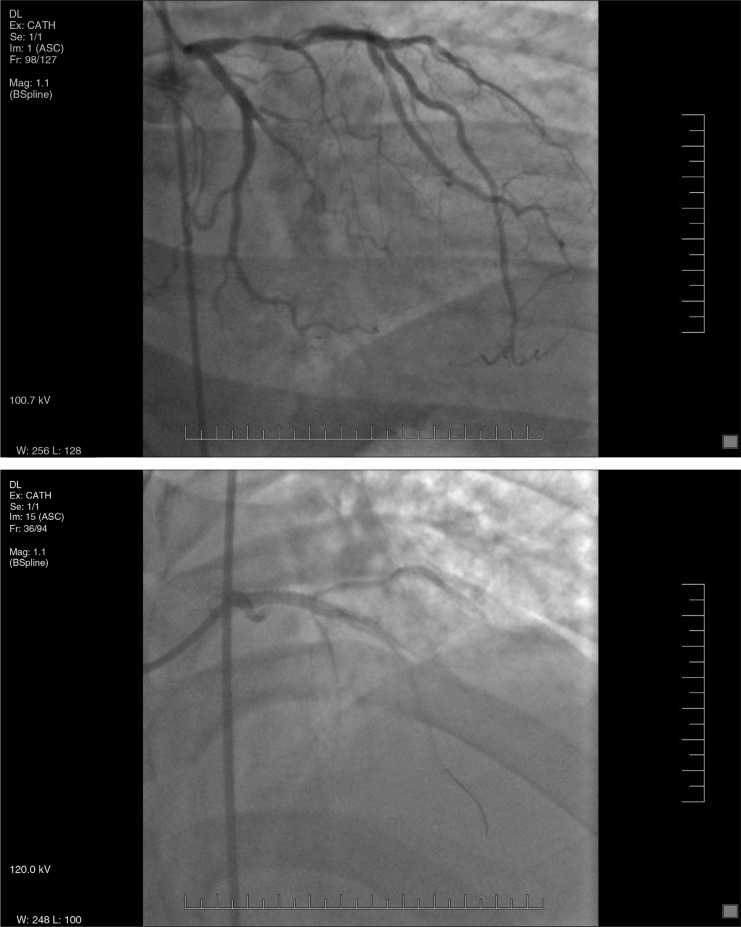
The patient was taken for urgent cardiac catheterization, which revealed 90% stenosis of the proximal left anterior descending (LAD) just before the major septal perforator (Fig. 2). He underwent successful PCI with a drug-eluting stent, was discharged 2 days later, and was still asymptomatic at 2-week follow-up in clinic.
Fig. 2.
Cardiac catheterization pictures of proximal LAD before and after stent placement.
Discussion
First described in 1982 by de Zwann et al. (3), Wellens’ syndrome can be classified as a pattern of ECG changes implying critical stenosis of the LAD (4). Criteria include a history of anginal chest pain, less than twice the upper limit of normal in cardiac serum markers (5), and biphasic or deeply inverted T waves in the precordial leads on an ECG obtained during a pain-free interval (6). This patient presented with Type 1 or A Wellens’, which comprises 25% of cases and has biphasic T waves in lead V2 and V3 (Fig. 1). The remaining 75% are Type 2 or B Wellens’ syndrome, which is deeply inverted, symmetrical T waves in predominantly V2 and V3 (1). This case highlights the need for timely identification of Wellens’ syndrome and the appropriate move to urgent coronary arteriography for possible angioplasty and assessment for emergency CABG. Stress testing should be avoided as this may induce an MI (1, 7). Recognition and appropriate management of Wellens’ is imperative as 75% of non-revascularized patients will progress to acute anterior wall MIs within 1 week, if left untreated (8).
Take home message
Recognition of the EKG findings of both Type 1 and 2 Wellens’ syndrome is critical to proper management and emergent intervention to avoid large anterior MI.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
References
- 1.Rhinehardt J, Brady WJ, Perron AD, Mattu A. Electrocardiographic manifestations of Wellens’ syndrome. Am J Emerg Med. 2002;20:638–43. doi: 10.1053/ajem.2002.34800. [DOI] [PubMed] [Google Scholar]
- 2.Yusuf Muharam M, Ahmad R, Harmy MY. The ‘widow maker’: Electrocardiogram features that should not be missed. Malays Fam Physician. 2013;8:45–7. [PMC free article] [PubMed] [Google Scholar]
- 3.de Zwann C, Bar FW, Wellens HJ. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J. 1982;103:730–6. doi: 10.1016/0002-8703(82)90480-x. [DOI] [PubMed] [Google Scholar]
- 4.de Zwann C, Bar FW, Janssen JH, Cheriex EC, Dassen WR, Brugada P, et al. Angiographic and clinical characteristics of patients with unstable angina showing an ECG pattern indicating critical narrowing of the proximal LAD coronary artery. Am Heart J. 1989;117:657–65. doi: 10.1016/0002-8703(89)90742-4. [DOI] [PubMed] [Google Scholar]
- 5.Singh B, Singh Y, Singla V, Nanjappa MC. Wellens’ syndrome: A classical electrocardiographic sign of impending myocardial infarction. BMJ Case Rep. 2013;2013 doi: 10.1136/bcr-2012-008513. pii: bcr2012008513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parikh S, Agarwal R, Mehrota A. Wellens syndrome: A life-saving diagnosis. Am J Emerg Med. 2012;30:255.e3–255.e5. doi: 10.1016/j.ajem.2010.10.014. [DOI] [PubMed] [Google Scholar]
- 7.Lawner B, Nable JV, Mattu A. Novel patterns of Ischemia and STEMI equivalents. Cardiol Clin. 2012;30:591–9. doi: 10.1016/j.ccl.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 8.Mead NE, O'Keefe KP. Wellens’ syndrome: An ominous EKG pattern. J Emerg Trauma Shock. 2009;2:206–8. doi: 10.4103/0974-2700.55347. [DOI] [PMC free article] [PubMed] [Google Scholar]