Abstract
Background
Gait changes in patients with hallux valgus, including altered kinematic and temporal-spatial parameters, have been documented in the literature. Although operative treatment can yield favorable clinical and radiographic results, restoration of normal gait in this population remains unclear. Segmental kinematic changes within the foot and ankle during ambulation after operative correction of hallux valgus have not been reported. The aim of this study was to analyze changes in multisegmental foot and ankle kinematics in patients who underwent operative correction of hallux valgus.
Methods
A 15-camera Vicon Motion Analysis System was used to evaluate 24 feet in 19 patients with hallux valgus preoperatively and postoperatively. The Milwaukee Foot Model was used to characterize segmental kinematics and temporal-spatial parameters (TSPs). Preoperative and postoperative kinematics and TSPs were compared using paired nonparametric methods; comparisons with normative data were performed using unpaired nonparametric methods. Outcomes were evaluated using the SF-36 assessment tool.
Results
Preoperatively, patients with hallux valgus showed significantly altered temporal-spatial and kinematic parameters. Postoperatively, kinematic analysis demonstrated restoration of hallux position to normal. Hallux valgus angles and intermetatarsal angles were significantly improved, and outcomes showed a significant increase in performance of physical activities. Temporal-spatial parameters and kinematics in the more proximal segments were not significantly changed postoperatively.
Conclusion
Postoperative results demonstrated significant improvement in foot geometry and hallux kinematics in the coronal and transverse planes. However, the analysis did not identify restoration of proximal kinematics.
Clinical Relevance
Further investigation is necessary to explore possible causes/clinical relevance and appropriate treatment interventions for the persistently altered kinematics.
Keywords: Motion Analysis, Kinematics, Gait, Hallux Valgus, Multisegmental Foot Model, Foot and Ankle
INTRODUCTION
Hallux valgus (HV) is the most common pathology involving the first metatarsophalangeal joint. Changes in gait in patients with hallux valgus have been documented in the literature.1,3,15,26 Patients have been noted to have slower walking speeds, shorter stride lengths, and prolonged stance phases.5,16,25 Recent studies have detailed multisegmental kinematic changes in the foot with hallux valgus during ambulation.5,11 The hallux showed a valgus position throughout the gait cycle and pronation peaking at push off. A more dorsifiexed forefoot and a more plantarflexed hindfoot suggest flattening of the longitudinal arch. Forefoot valgus from terminal stance through initial swing, hindfoot inversion and tibial internal rotation are findings consistent with lateral plantar loading.
Over 100 different operative treatments have been proposed for hallux valgus,7 each aiming to restore alignment and biomechanical function.19 Operative treatment of hallux valgus has demonstrated very good results.9,23,24 Patients who underwent surgery were more satisfied, had higher functional scores and less pain, and required less help from a specialist for their footwear as compared to patients who were treated nonsurgically with orthoses. However, recent findings from plantar pressure analysis have suggested that physiologic gait patterns are not restored after hallux valgus surgery, despite favorable clinical and radiographic results.19,20
We have conducted a study characterizing gait in patients with hallux valgus which included preliminary postoperative findings.5 These initial findings showed significantly improved postoperative hallux position in all three planes, but temporal-spatial parameters and range of motion did not exhibit similar improvements. This study also demonstrated significantly lower SF-36 scores (Physical Functioning and Bodily Pain subscales) preoperatively when compared to age-matched normative values,2 denoting some functional impairment. Based on these initial findings, we hypothesized that surgery for hallux valgus would restore alignment and patient-reported function but that proximal kinematics and temporal-spatial parameters would not show significant postoperative changes. The aim of this study was to analyze changes in multisegmental foot and ankle kinematics in patients who underwent hallux valgus surgery.
MATERIALS AND METHODS
This prospective study, involving patients with hallux valgus from the Medical College of Wisconsin/Froedtert Hospital Foot and Ankle Clinics, was approved by the Institutional Review Board. All recruited subjects gave informed consent prior to participating in the study. Twenty-four feet (15 lefts and nine rights) in 19 subjects (17 females and two males) were tested at the Orthopaedic and Rehabilitation Engineering Center (OREC) Motion Analysis Laboratory. The mean age at the time of preoperative testing was 52.5 (24 to 72) years. All subjects demonstrated mild to severe hallux valgus, which was defined by the hallux valgus angle or HVA (HVA ≥ 15 degrees) and the intermetatarsal angle or IMA (IMA ≥ 9 degrees).6 Clinical assessment and operative treatment were performed by a single orthopaedic surgeon (R.M.M.) Preoperative gait evaluation was done at an average of 45 days prior to surgery. Postoperative testing was conducted only after complete return to a stable ambulatory pattern. Followup visits were conducted between 7 to 60 months with a mean of 16 months. Data from these subjects pre- and postoperatively are referenced as HVpre and HVpost, respectively.
Radiographic and outcomes assessment
Changes in static deformity were evaluated based on measurements of the HVA and IMA on weightbearing AP plain radiographs.
The SF-36 Health Survey was administered at both pre-and postoperative visits to objectively evaluate functional levels before and after surgery. Specific subscale scores of interest included four areas: Physical Functioning (extent to which health interferes with physical activities), Role Functioning-Physical (extent to which physical health interferes with work and daily activities), Bodily Pain (intensity and effect of pain on work), and General Health (personal evaluation of health).
Motion analysis
Foot and ankle motion analyses were performed using a video-based Vicon 524 Motion Analysis System (Vicon Motion Systems, Inc.; Lake Forest, CA) with 15 cameras operating at 120 Hz. Data were collected as subjects walked at self-selected speed along a 6-m walkway. At least three walking trials were completed. Temporal-spatial parameters (walking speed, stride length, cadence, and stance/swing ratio) as well as foot and ankle kinematics (position and range of motion) were measured using the Milwaukee Foot Model (MFM). The MFM is a four-segment kinematic model which has been validated for adult and pediatric populations.13,17
Using the MFM, the foot and ankle were divided into tibia, hindfoot, forefoot, and hallux, and measures of motion for each segment were calculated in three planes (sagittal, coronal, and transverse). Measurements from weightbearing radiographs were used to index surface marker motion to the underlying bony anatomy and create local bone-based axes for each segment. The reference coordinate system for the tibia was the laboratory (global) coordinate system. The reference coordinate system for all other segments was the body coordinate system for the next most proximal segment (i.e. hindfoot with respect to tibia, forefoot with respect to hindfoot, and hallux with respect to forefoot).12
Segment positions and ranges of motion (ROM) as captured during marker-based motion analysis testing were compared pre- and postoperatively during each of the seven phases of gait as described by Perry.18 The two groups were thus compared in each of the seven phases of gait, namely load response (0% to 10% of the gait cycle), midstance (10% to 30%), terminal stance (30% to 50%), preswing (50% to 60%), initial swing (60% to 73%), midswing (73% to 87%), and terminal swing (87% to 100%). ROM was defined as maximum position minus minimum position within a particular gait phase. Timing and position information associated with heelstrike and toe-off events were used to determine temporal-spatial parameters (walking speed, stride length, cadence, and stance-swing ratio).
Statistical analysis
Preoperative and postoperative values for radiographic measurements and the SF-36 were compared using the Wilcoxon signed rank test (p ≤ 0.05). Preoperative and postoperative temporal-spatial and kinematic data comparisons were also analyzed using the Wilcoxon signed rank test, a version of the Friedman’s test (a nonparametric alternative to repeated measures AN OVA). Comparisons to a previously tested population of 25 healthy ambulators (13 males and 12 females) with no known foot pathology or surgeries were also made using unpaired nonparametric methods.5 Normative data were obtained following the protocol described for the HV population. A Bonferroni correction was used to achieve a family-wise 5% overall error rate in adjusting for multiple tests over the set of seven test points in the gait cycle. This made p < 0.002 the level of significance for all joint kinematic comparisons.
The relationship between followup time and postoperative change was analyzed using the Pearson correlation coefficient. For each kinematic and temporal-spatial variable N, we analyzed the relationship between Npost-Npre and followup time in days.
RESULTS
Radiographic and outcomes assessment
Mean HVA decreased from 30 (HVpre; range, 17 to 50) degrees to 13 (HVpost; range, −5 to 28) degrees (p < 0.0001), and mean IMA decreased from 15 (HVpre; range, 10 to 21) degrees to 10 (HVpost; range, 3 to 19) degrees (p = 0.0029). Average metatarsal length was also found to be shorter postoperatively (p = 0.004) with mean lengths of 65.3 (range, 57 to 73) mm and 63.7 (range, 54 to 73) mm for HVpre and HVpost, respectively: SF-36 subscale results are reported in Table 1. Of these subscale scores, statistically significant improvement was seen in Physical Functioning (p = 0.0059).
Table 1.
SF-36 Results
| Mean and Standard Deviation |
|||
|---|---|---|---|
| Preop | Postop | p | |
| Physical Functioning | 77.8 ± 16.9 | 93.5 ± 9.1 | 0.01 |
| Role Functioning-Physical | 84.4 ± 30.1 | 87.0 ± 29.1 | 0.63 |
| Bodily Pain | 62.2 ± 20.4 | 78.3 ± 24.7 | 0.15 |
| General Health | 79.9 ± 13.8 | 83.3 ± 12.4 | 0.64 |
| Vitality | 67.8 ± 21.4 | 67.8 ± 18.2 | 0.43 |
| Social Functioning | 88.3 ± 21.6 | 90.2 ± 18.8 | 0.61 |
| Role Functioning-Emotional | 85.4 ± 34.4 | 87.0 ± 28.0 | 0.94 |
| Mental Health | 75.3 ± 22.4 | 77.6 ± 16.1 | 0.91 |
Values are scaled to a 100-point scale.
Temporal-spatial parameters
Preoperatively, persons with hallux valgus demonstrated significantly slower walking speed (p = 0.0004) and shorter stride length (p < 0.0001), with significantly prolonged stance (p = 0.0154) when compared to the normal population (Table 2). After surgery, no statistical differences compared to the preoperative data were evident in temporal-spatial parameters. Correlation analysis with the Pearson coefficient did not demonstrate any significant relationship between followup time and postoperative change from the baseline condition. No correlations were greater than 0.515 and none achieved significance at the 1% level. Postoperative comparisons to the normal population showed that walking speed (p = 0.0046) and stride length (p < 0.0001) were smaller. Stance duration, however, was not significantly different (p = 0.0745).
Table 2.
Temporal-Spatial Parameters (mean ± SD)
| Temporal-Spatial Parameters |
HVPre | HVPost | Normal |
p value HVpre vs. HVpost |
p value HVpre vs. Normal |
p value HVpost vs. Normal |
|---|---|---|---|---|---|---|
| Stride Length | 1.1 ± 0.1 | 1.2 ± 0.1 | 1.3 ± 0.1 | 0.0633 | <0.0001 ◆ | 0.0001 ◆ |
| Cadence | 105.5 ± 6.5 | 105.4 ± 5.6 | 104.2 ± 7.9 | 1.0000 | 0.4517 | 0.4394 |
| Walking Speed | 1.0 ± 0.1 | 1.0 ± 0.1 | 1.1 ± 0.1 | 0.3037 | 0.0004 ◆ | 0.0046 ◆ |
| Stance % | 64.3 ± 2.0 | 63.8 ± 2.1 | 62.3 ± 2.6 | 0.1034 | 0.0154 ◆ | 0.0745 |
, significant at p < 0.05.
Hallux kinematics
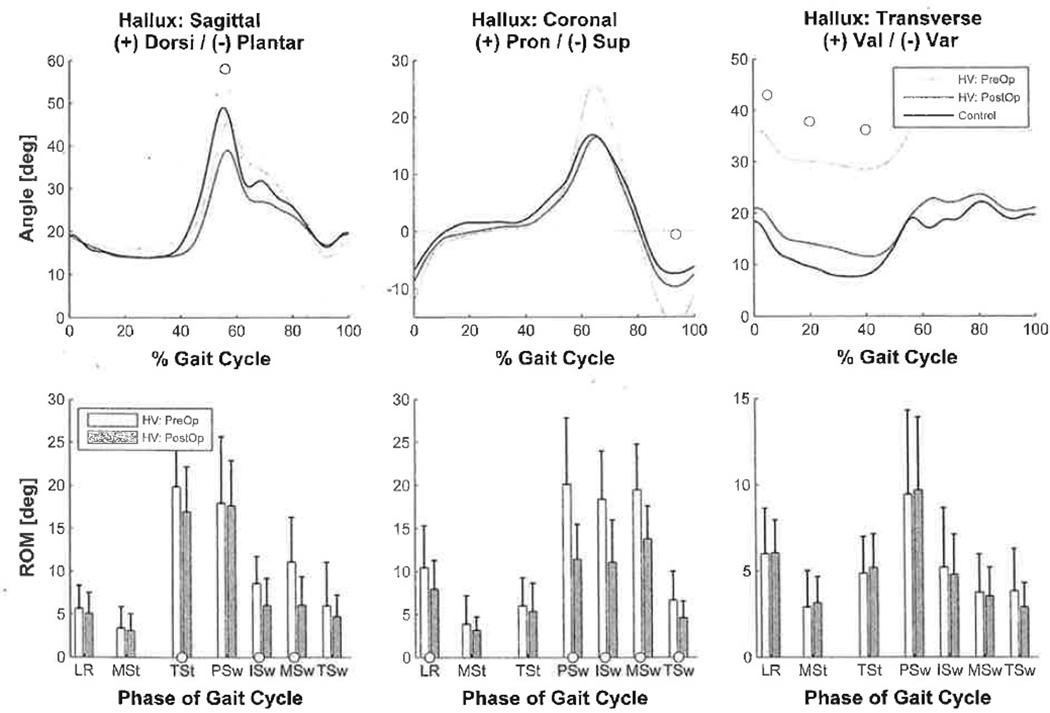
Hallux kinematics were calculated relative to the forefoot. Preoperatively, compared to the normative data, hallux position was in valgus (p < 0.0001) throughout the gait cycle (Figure 1). Transverse ROM was significantly smaller from midswing through terminal stance (p ≤ 0.0008). Sagittal range was also significantly smaller from terminal swing through midstance (p ≤ 0.0011). In the coronal plane, maximum hallux pronation during preswing was significantly greater (p ≤ 0.0007). Hallux position at terminal swing was significantly more supinated (p < 0.0001). Coronal ROM was significantly increased from preswing to midswing (p ≤ 0.0003). Postoperatively, compared to preoperative values, hallux valgus position significantly shifted toward normal (p ≤ 0.0001). Excessive hallux pronation and supination in the coronal plane also shifted toward normal values (p ≤ 0.0011) as did coronal ROM (p ≤ 0.0002). Compared to normative data, postoperative transverse (p ≤ 0.0011) and sagittal (p ≤ 0.0003) ranges remained significantly smaller. Other postoperative measures were not significantly different from normal values.
Fig. 1.
Upper: average hallux kinematics during complete gait cycle (HVpre versus HVpost versus Normals). Circles denote phases of gait cycle with significantly different minimum and maximum positions (HVpre versus HVpost). Lower: hallux ROM (average ± SD). Circles denote phases of gait cycle with significantly different ROMs (HVpre versus HVpost). Note: Hallux kinematics were calculated relative to forefoot.
Forefoot kinematics
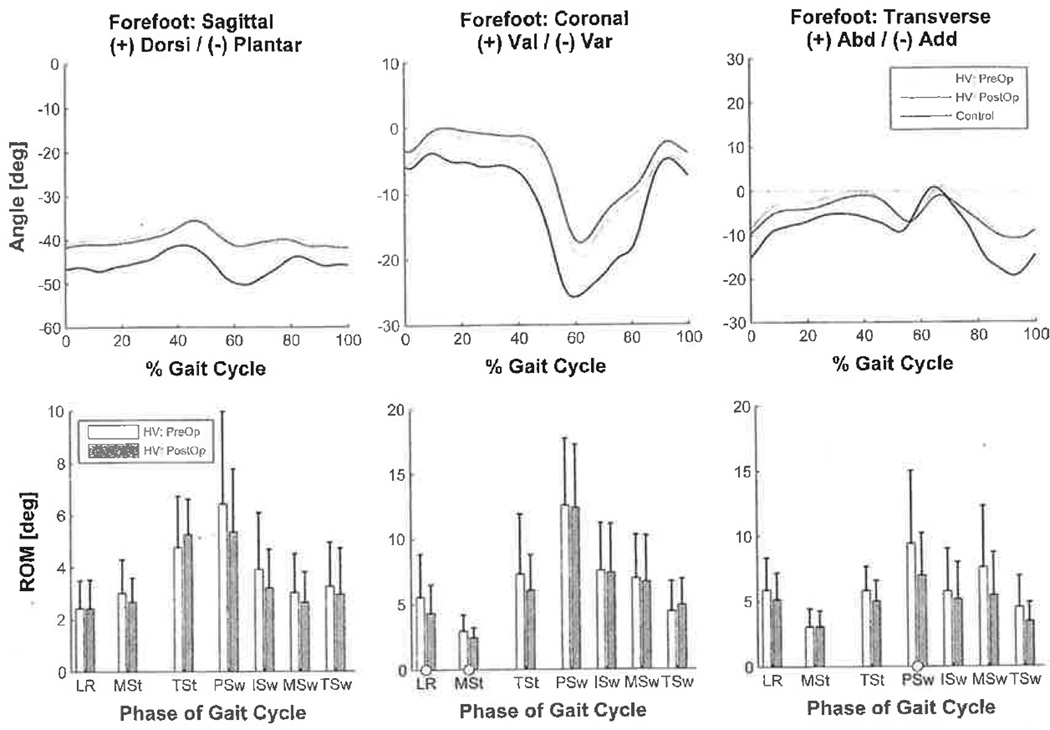
Forefoot kinematics were calculated relative to the hind-foot. Preoperatively, compared to normal data, significantly smaller forefoot varus was seen from terminal stance through initial swing (p ≤ 0.0018) in the coronal plane (Figure 2). Sagittal and transverse ROMs were significantly smaller from initial swing through midstance (p ≤ 0.0004). Coronal range was smaller at midstance and midswing through terminal swing (p = 0.0003). After surgery, there was no significant change in forefoot kinematics. Abnormalities in forefoot kinematics seen preoperatively remained postoperatively with respect to the normal population (p < 0.0019).
Fig. 2.
Upper: average forefoot kinematics during complete gait cycle (HVpre versus HVpost versus Normals). Circles denote phases of gait cycle with significantly different minimum and maximum positions (HVpre versus HVpost). Lower: forefoot ROM (average ± SD). Circles denote phases of gait cycle with significantly different ROMs (HVpre versus HVpost). Note: Forefoot kinematics were calculated relative to hindfoot.
Hindfoot kinematics
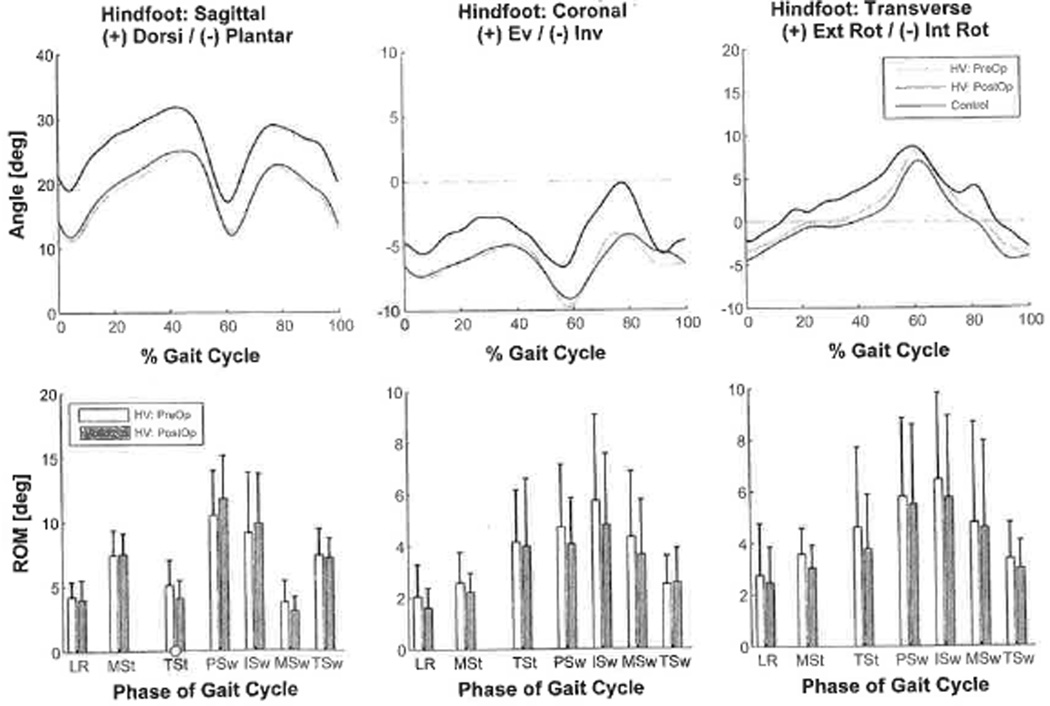
Hindfoot kinematics were calculated relative to the tibia. Although not significantly different from the healthy ambulators, hindfoot position prior to surgery was inverted in 15 of 24 subjects (Figure 3). After surgery, hindfoot position and ROM did not change significantly.
Fig. 3.
Upper: average hindfoot kinematics during complete gait cycle (HVpre versus HVpost versus Normals). Circles denote phases of gait cycle with significantly different minimum and maximum positions (HVpre versus HVpost). Lower: hindfoot ROM (average ± SD). Circles denote phases of gait cycle with significantly different ROMs (HVpre vs, HVpost). Note: Hindfoot kinematics were calculated relative to tibia.
Tibia Kinematics
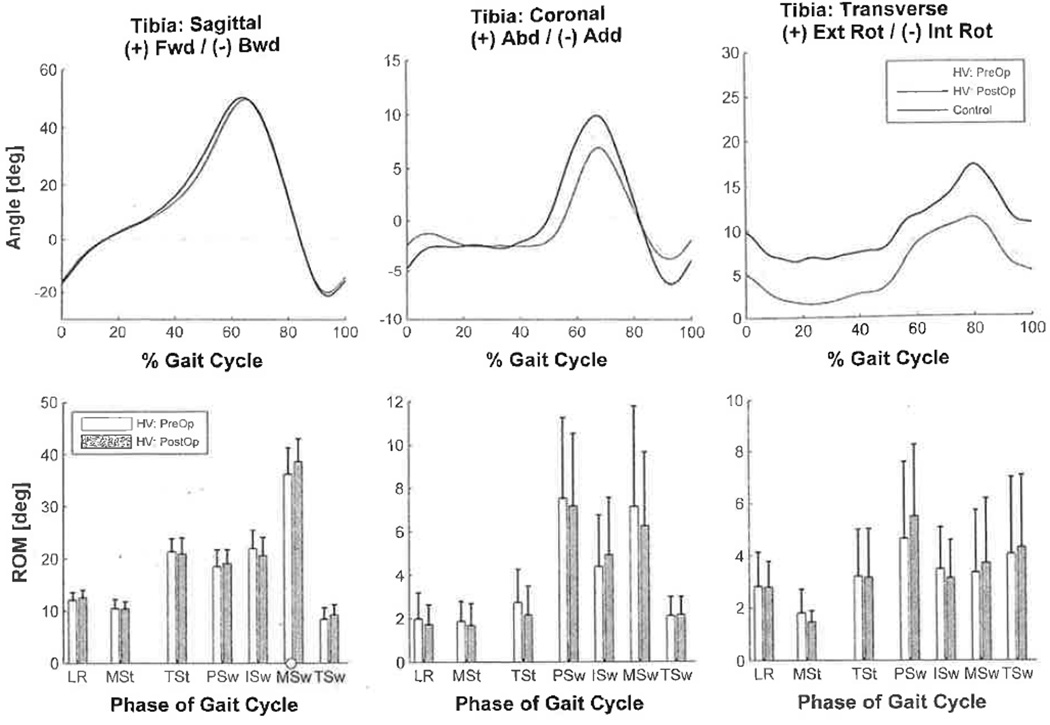
Tibia kinematics were calculated relative to the laboratory global values. Preoperatively, there were significant ROM differences noted in various phases in three planes (p ≤ 0.0014) with respect to the control group. No significant differences were observed in segment positions of the tibia.
No significant changes were seen in tibia kinematics postoperatively (Figure 4). Significant postoperative ROM differences were still noted with respect to the normal population (p < 0.0017).
Fig. 4.
Upper: average tibia kinematics during complete gait cycle (HVpre versus HVpost versus Normals). Circles denote phases of gait cycle with significantly different minimum and maximum positions (HVpre versus HVpost). Lower: tibia ROM (average ± SD). Circles denote phases of gait cycle with significantly different ROMs (HVpre versus HVpost). Note: Tibia kinematics were calculated relative to laboratory global.
DISCUSSION
Preoperative findings of our current study were consistent with biomechanical dysfunction and impairment as noted by Shereff.21 Postoperative findings indicated better foot geometry and improved patient-reported function after surgery. Kinematics demonstrated that hallux position was restored to normal. Significant postoperative improvements were also seen in HVA and IMA. Outcomes analysis showed significant increase in performance of physical activities. These findings point to significant improvements in radiographic alignment, functional outcomes (SF-36), and hallux kinematics.
Postoperative results from this study suggest that although operative correction of hallux valgus did result in a more anatomically normal foot, reduced hallux motion, and improved overall function, it did not appear to restore normal gait. The more proximal segments did not demonstrate significant improvements in either ROM or position. While this lack of significant change does not indicate statistical equivalence, it does provide useful insight and a potential area for future study. Alternatively, the existing data set was reviewed using a post-hoc power analysis to determine the sample sizes necessary to detect a 10% difference in parameter values while rejecting the hypothesis of no difference with 80% power and alpha = 0.05. Power calculations were based on the paired t-test with 5% inflation on the sample size for the use of its nonparametric alternative. Population sizes of n = 76 to n = 5480 would be required to reject the null hypothesis of no difference. The variation in population size ranges from a minimum of 76 for hindfoot, coronal plane, midstance ROM to a maximum of 5480 for forefoot coronal plane, preswing ROM. Other comparisons lie between these population sizes. In future studies, presence of other proximal anatomic or kinematic abnormalities, which may be involved in the pathogenesis of hallux valgus, must be investigated as well.6 A combined lower extremity and foot model motion analysis would be useful to investigate such kinematic abnormalities. Investigation of such changes may provide insight to possible reasons why statistical changes in proximal kinematics were not identified.
Patients who undergo corrective osteotomy for hallux valgus may exhibit some shortening of the first ray postoperatively. This is especially true for older patients who exhibit joint stiffness in which some shortening is required to improve range of motion. An osteotomy which produces shortening of the metatarsal or dorsiflexion translation (metatarsal elevation) while correcting these deformities will change the biomechanics of the forefoot and the function of the first ray.22 In these cases, weight is not transferred to the first metatarsal head during ambulation because of its reduced length, and the stress of push-off is transferred to the longer second and lateral metatarsals during the third rocker of gait.15,16 Our postoperative findings of continued dorsiflexion and valgus shifting of the forefoot during plantar loading, as well as internal tibial rotation throughout the gait cycle, are consistent with lateral plantar loading. Hallux valgus surgery may also result in metatarsal elevation, which may exhibit the same gait alteration.7,22 In the current study, the measured change in metatarsal length was fairly small and the clinical significance of this change is unclear.
Over a long period of time, soft tissue imbalance also occurs across the first MTP joint in hallux valgus.8 There are a number of musculotendinous units that function across the MTP joint, and the mechanics of their functional restoration following surgery have not been thoroughly described in the literature. Saltzman et al. investigated the major flexor moment arm of the first metatarsophalangeal joint in a cadaver model.19 They demonstrated that neither translational osteotomies nor supinatory rotations of the first metatarsal had any appreciable effect on the altered flexor moment arms in hallux valgus. They also noted that although the standard distal metatarsal osteotomy procedures used in hallux valgus surgery may address foot deformity, they appear to have no beneficial effect in terms of restoring normal function to the flexor apparatus of the hallux.
Further understanding of the biomechanical deficiencies will require measures of internal joint forces and moments within the various joints of the foot.4,10,14 At this time, standard gait models treat the foot as a single rigid segment, and the technological challenges limit the ability to accurately model multisegmental foot kinetics. To obtain these measures, the current segmental kinematic model must evolve to include multisegmental three-dimensional kinetic measurements. Clinical benefits of more rigorous modeling may include footwear prescription, surgical planning, postoperative management, and footwear/orthotics design.
CONCLUSION
Hallux valgus correction improves radiographic alignment, functional outcomes, and hallux kinematics. However, it is not clear whether or not hallux valgus correction alters the kinematics of the forefoot, hindfoot and tibia. A markedly larger sample size may demonstrate a change, but we were unable to identify any statistically significant kinematic changes other than to the hallux. It is also not clear whether or not hallux valgus correction improves temporal-spatial parameters of gait. However, patients with hallux valgus do have temporal-spatial gait abnormalities.
Acknowledgments
This work was supported by the National Institute on Disability and Rehabilitation Research (NIDRR), U.S. Department of Education grant numbers H133P020004 and H133P040008.
REFERENCES
- 1.Blomgren M, Turan I, Agadir M. Gait analysis in hallux valgus. J Foot Surg. 1991;30:70–71. [PubMed] [Google Scholar]
- 2.Bowling A, Bond M, Jenkinson C, Lamping DL. Short Form 36 (SF-36) Health Survey questionnaire: which normative data should be used? Comparisons between the norms provided by the Omnibus Survey in Britain, the Health Survey for England and the Oxford Healthy Life Survey. J. Public Health Med. 1999;21:255–270. doi: 10.1093/pubmed/21.3.255. http://dx.doi.org/10.1093/pubmed/21.3.255. [DOI] [PubMed] [Google Scholar]
- 3.Brodsky JW, Beischer AD, Robinson AHN, Westra S, Negrine JP, Shabat S. Surgery for hallux valgus with proximal crescentic osteotomy causes variable postoperative pressure patterns. Clin Orthop. 2006;443:280–286. doi: 10.1097/01.blo.0000191269.50033.ec. http://dx.doi.org/10.1097/01.blo.0000191269.50033.ec. [DOI] [PubMed] [Google Scholar]
- 4.Buczek FL, Walker MR, Rainbow MJ, Cooney KM, Sanders JO. Impact of mediolateral segmentation on a multi-segment foot model. Gait Posture. 2006;23:519–522. doi: 10.1016/j.gaitpost.2005.06.004. http://dx.doi.Org/10.1016/j.gaitpost.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 5.Canseco K, Rankine L, Long J, et al. Motion of the multisegmental foot in hallux valgus. Foot Ankle Int. 2010;31:146–152. doi: 10.3113/FAI.2010.0146. http://dx.doi.Org/10.3113/FAI.2010.0146. [DOI] [PubMed] [Google Scholar]
- 6.Coughlin MJ. Hallux valgus. J Bone Joint Surg Am. 1996;78:932–966. [PubMed] [Google Scholar]
- 7.Easley ME, Trnka HJ. Current concepts review: hallux valgus part II. operative treatment. Foot Ankle Int. 2007;28:748–758. doi: 10.3113/FAI.2007.0748. http://dx.doi.org/10.3113/FAI.2007.0748. [DOI] [PubMed] [Google Scholar]
- 8.Eustace S, Williamson D, Wilson M, et al. Tendon shift in hallux valgus: observations at MR imaging. Skeletal Radiol. 1996;25:519–524. doi: 10.1007/s002560050128. http://dx.doi.org/10.1007/s002560050128. [DOI] [PubMed] [Google Scholar]
- 9.Ferrari J, Higgins JP, Prior TD. Interventions for treating hallux valgus (abductovalgus) and bunions. Cochrane Database Syst. Rev. 2004;l:CD000964. doi: 10.1002/14651858.CD000964.pub2. [DOI] [PubMed] [Google Scholar]
- 10.Harris GF, Smith PA, Marks RM. Foot and Ankle Motion Analysis: Clinical Treatment and Technology. 2008 [Google Scholar]
- 11.Hwang SJ, Choi HS, Cha SD, Lee KT, Kim YH. Multi-Segment Foot Motion Analysis on Hallux Valgus Patients. 2005:6875–6877. doi: 10.1109/IEMBS.2005.1616085. [DOI] [PubMed] [Google Scholar]
- 12.Johnson JE, Lamdan R, Granberry WF, Harris GF, Carrera GF. Hindfoot coronal alignment: a modified radiographic method. Foot Ankle Int. 1999;20:818–825. doi: 10.1177/107110079902001212. [DOI] [PubMed] [Google Scholar]
- 13.Kidder SM, S AF, Jr, Harris GF, Johnson JE. A system for the analysis of foot and ankle kinematics during gait. IEEE Trans Rehabil Eng. 1996;4:25–32. doi: 10.1109/86.486054. http://dx.doi.org/10.1109/86.486054. [DOI] [PubMed] [Google Scholar]
- 14.MacWilliams BA, Cowley M, Nicholson DE. Foot kinematics and kinetics during adolescent gait. Gait Posture. 2003;17:214–224. doi: 10.1016/s0966-6362(02)00103-0. http://dx.doi.org/10.1016/S0966-6362(02)00103-0. [DOI] [PubMed] [Google Scholar]
- 15.Menz HB, Lord SR. Gait instability in older people with hallux valgus. Foot Ankle Int. 2005;26:483–489. doi: 10.1177/107110070502600610. [DOI] [PubMed] [Google Scholar]
- 16.Merkel KD, Katoh Y, W JE, Jr, Chao EY. Mitchell osteotomy for hallux valgus: long-term follow-up and gait analysis. Foot Ankle. 1983;3:189–196. doi: 10.1177/107110078300300402. [DOI] [PubMed] [Google Scholar]
- 17.Myers KA, Wang M, Marks RM, Harris GF. Validation of a multisegment foot and ankle kinematic model for pediatric gait. IEEE Trans Neural Syst Rehabil Eng. 2004;12:122–130. doi: 10.1109/TNSRE.2003.822758. http://dx.doi.org/10.1109/TNSRE.2003.822758. [DOI] [PubMed] [Google Scholar]
- 18.Perry J. Gait Analysis, Thorofare, NJ, SLACK Incorporated. 1992 [Google Scholar]
- 19.Saltzman CL, Aper RL, Brown TD. Anatomic determinants of first metatarsophalangeal flexion moments in hallux valgus. Clin. Orthop. 1997:261–269. doi: 10.1097/00003086-199706000-00035. http://dx.doi.org/10.1097/00003086-199706000-00035. [DOI] [PubMed] [Google Scholar]
- 20.Schuh R, Hofstaetter SG, Adams SB, Jr, et al. Rehabilitation after hallux valgus surgery: importance of physical therapy to restore weight bearing of the first ray during the stance phase. Phys. Ther. 2009;89:934–945. doi: 10.2522/ptj.20080375. http://dx.doi.org/10.2522/ptj.20080375 [DOI] [PubMed] [Google Scholar]
- 21.Shereff MJ. Pathophysiology, anatomy, and biomechanics of hallux valgus. Orthopedics. 1990;13:939–945. doi: 10.3928/0147-7447-19900901-06. [DOI] [PubMed] [Google Scholar]
- 22.Stephens MM. Does shortening of the first ray in the treatment of adolescent hallux valgus prejudice the outcome? J. Bone Joint Surg. Br. 2006;88:858–859. doi: 10.1302/0301-620X.88B7.17830. http://dx.doi.org/10.1302/0301-620X.88B7.17830. [DOI] [PubMed] [Google Scholar]
- 23.Thordarson D, Ebramzadeh E, Moorthy M, Lee J, Rudicel S. Correlation of hallux valgus surgical outcome with AOFAS forefoot score and radiological parameters. Foot Ankle Int. 2005;26:122–127. doi: 10.1177/107110070502600202. [DOI] [PubMed] [Google Scholar]
- 24.Torkki M, Malmivaara A, Seitsalo S, et al. Surgery vs orthosis vs watchful waiting for hallux valgus: a randomized controlled trial. JAMA. 2001;285:2474–2480. doi: 10.1001/jama.285.19.2474. http://dx.doi.org/10.1001/jama.285.19.2474. [DOI] [PubMed] [Google Scholar]
- 25.Vittas D, Jansen EC, Larsen TK. Gait analysis before and after osteotomy for hallux valgus. Foot Ankle. 1987;8:134–136. doi: 10.1177/107110078700800303. [DOI] [PubMed] [Google Scholar]
- 26.Waldecker U. Metatarsalgia in hallux valgus deformity: a pedographic analysis. J Foot Ankle Surg. 2002;41:300–308. doi: 10.1016/s1067-2516(02)80048-5. http://dx.doi.org/10.t016/S1067-2516(02)80048-5. [DOI] [PubMed] [Google Scholar]