Abstract
Objective
To describe the rate of concomitant oral corticosteroid use at antitumour necrosis factor (TNF) initiation and at disease remission, and to assess its effect on incidence of infection and sustainability of remission among patients with rheumatoid arthritis (RA) treated with infliximab in Canadian routine care.
Methods
Biological naïve patients with RA followed in the Biologic Treatment Registry Across Canada (BioTRAC) were included. The time-dependent association between corticosteroid dose (no use, ≤5 mg/day, >5 mg/day) and the incidence of first infection, while considering possible confounders, remission sustainability and the incidence of subsequent infections were assessed with Cox regression.
Results
838 patients were included; mean (SD) baseline age and disease duration were 55.6 (13.5) and 10.5 (9.8) years, respectively. After a mean (SD) of 51.3 (43.6) months, the total incidence of adverse events (AEs) and infections were 110.2 and 19.6 per 100 person-years (PY), respectively. In multivariate analysis, the HR (95% CI) for acquiring an infection was 2.48 (1.24 to 4.98) with >5 mg/day of corticosteroids versus no corticosteroids. Similarly, ≤5 mg/day of corticosteroids was associated with increased hazard for infection (2.12 (0.97 to 4.66)). Despite DAS28 (disease activity score 28) or Clinical Disease Activity Index (CDAI) remission, corticosteroids were continued in 16.4% and 16.7% of cases, respectively. Continued corticosteroid treatment was not associated with sustainability of remission (HRDAS28 (95% CI) 1.40 (0.95 to 2.06); HRCDAI 1.19 (0.75 to 1.88)), however, it had a significant impact on development of infection (HRDAS28 (95% CI) 1.78 (1.00 to 3.19); HRCDAI 2.38 (1.14 to 4.99)).
Conclusions
Oral corticosteroid treatment was associated with increased risk of development of infection without impacting sustainability of remission. These results support the notion that corticosteroids should be used concomitantly with anti-TNF for the shortest period possible to achieve remission, and then tapered.
Trial registration number
Keywords: Rheumatoid Arthritis, Corticosteroids, TNF-alpha, DMARDs (biologic), Infections
Key messages.
What is already known on this subject?
Oral corticosteroids remain a viable and widely used therapeutic option in rapidly and effectively managing rheumatoid arthritis symptoms.
What might this study add?
Despite achievement of remission a considerable number of RA patients remain on corticosteroid treatment. Continued corticosteroid treatment was not associated with sustainability of remission; however, it had a significant impact on development of infection.
How might this impact on clinical practice?
Corticosteroids should be administered for the shortest period possible in RA patients concomitantly receiving biologic therapy to achieve remission, and then tapered.
Introduction
Oral corticosteroids remain a viable and widely used therapeutic option in rapidly and effectively managing rheumatoid arthritis (RA) symptoms.1 However, corticosteroid use is controversial, with concerns regarding safety outcomes, including cardiovascular disease, diabetes, osteoporosis, peptic ulcers and, more commonly, infections.2 Several studies have confirmed that the use of corticosteroids is associated with an increased risk for infection: a study by Wolfe et al3 showed that a dose-related relationship exists between use of prednisone and incidence of pneumonia, and identified prednisone as the treatment variable conferring the greatest increase in risk of infection in patients with RA. Similarly, Lacaille et al4 found use of corticosteroid, with or without concomitant non-biological disease-modifying antirheumatic drug (DMARD) administration, to be significantly associated with an increase in the risk of developing both mild and serious infections, and Doran et al5 identified corticosteroids as the only RA medication type associated with an increased infection risk in patients with RA.
Based on the results of these and other studies, in which systemic corticosteroid use for the treatment of RA was associated with increased risk of infection6–9 and other comorbidities,10 the most recent treatment guidelines put forth by the Canadian Rheumatology Association (CRA),11 as well as the European League against Rheumatism (EULAR),12 dictate that corticosteroids, administered in the lowest possible dose, could be added to DMARD therapy as part of the initial treatment strategy for the management of RA, or as bridging therapy for managing flares;11 12 however, they should be tapered as rapidly as clinically feasible.
Several Canadian observational studies have estimated corticosteroid use among patients with RA between 30% and 40%,13–15 with up to approximately 75% of patients exposed at any time in their course of treatment.14 In 2007, in Canada, 62% of corticosteroid prescriptions were for patients with a diagnosis that fell into the category of arthritis conditions.16 Despite their widespread use in RA, information on the concomitant administration of corticosteroids with antitumour necrosis factor (TNF) agents in routine clinical care as well as on the adherence to currently recommended practice guidelines is scarce.
Postapproval clinical epidemiological studies allow the assessment of the real-world utilisation of treatments, and the evaluation of their effectiveness and safety in the target population under routine clinical care. Using data from the Biologic Treatment Registry Across Canada (BioTRAC), an ongoing, Canada-wide, multicentre, prospective, observational registry of patients with inflammatory arthritis, the aim of this analysis was to describe the rate of concomitant corticosteroid use at anti-TNF initiation and at the time of disease remission, and to assess its effect on the incidence of infections and sustainability of remission among patients with RA treated with infliximab in Canadian routine clinical practice.
Methods
Study design
BioTRAC is an ongoing Canadian prospective, multicentre, observational registry collecting real-world clinical, laboratory, patient-centric and safety data in RA, ankylosing spondylitis and psoriatic arthritis patients treated with infliximab, golimumab or ustekinumab as part of their routine care. The historical development of the registry has been described by Thorne et al.17 To date, there are over 70 rheumatology sites participating, both in an institutional and private setting, with over 1800 patients enrolled in the programme across all indications. In accordance with the observational nature of the registry, there is no protocol-defined intervention in patient management, and all clinical decisions and treatments are based on routine practice and the judgement of the treating physicians. Patients provided written informed consent prior to participation in the study. Ethics approval for participation in the BioTRAC programme was obtained from the respective Research Ethics Boards of participating institutional sites, and a Central Institutional Review Board (IRB Services, Ontario Canada) for private practice sites. BioTRAC is conducted according to the tenets of the Declaration of Helsinki.
Study population
Biological naïve patients, or patients previously treated with a biological for less than 6 months and who are eligible for treatment with infliximab, golimumab or ustekinumab as per their respective Canadian Product Monograph are considered for inclusion in the registry. For the purpose of the current analysis, only patients with RA who received at least one dose of infliximab up to June 2011 were included (safety population; N=838). All effectiveness analyses were performed in the modified intent-to-treat (mITT; N=628) population comprising all enrolled patients who received at least one dose of infliximab and had at least one follow-up assessment.
Data collection
The following clinical/laboratory parameters and patient-reported outcomes are collected as per routine care at baseline (ie, study enrolment) and at all follow-up visits with suggested assessments every 6 months, given that this is within acceptable practice patterns for patients with active RA:11 morning stiffness, swollen joint count (SJC-28), tender joint count (TJC-28), patient's (PtGA) and physician's (PhGA) global assessment of disease activity, health assessment questionnaire (HAQ), patient's assessment of pain, C reactive protein and erythrocyte sedimentation rate. Remission was defined per the DAS28 (disease activity score 28) (<2.6) and Clinical Disease Activity Index (CDAI) (≤2.8) criteria. Additionally, at each visit, concomitant RA (including, but not limited to, DMARDs, non-steroidal anti-inflammatory drugs (NSAIDs) and steroids) and non-RA medication use is recorded by the treating physician. Safety, including the occurrence of infections, is assessed with the incidence of physician-detected and patient-reported treatment-emergent adverse events (AEs).
Statistical analysis
Summary statistics including the mean and SD for continuous variables, and the count and proportion for discrete and categorical variables, were used to describe the baseline patient profile, the incidence rate (number of events per person time) of AEs/serious AEs (SAEs)/infections/serious infections, as well as steroid use at the time of remission. Drug survival was described with the Kaplan-Meier estimator of the survival function. The impact of steroid use on time-to-first infection was assessed using Cox regression. For this, steroid use was used as a time-dependent covariate to take into consideration changes over time in steroid utilisation. Potential confounders considered were: age, gender, presence of comorbidity at baseline using concomitant medications as a proxy, HAQ disability index (HAQ-DI), enrolment period, baseline disease duration, geographical zone and number of steroid prescriptions. Backwards variable selection with α level of 0.2 was used to derive the parsimonious model. Sustainability of remission and time to infection by continued steroid use among patients in remission were assessed with the Kaplan-Meier estimator of the survival function, and the effect of continued steroid use was compared with the log-rank test. Owing to the low number of remission cases, steroid use in these analyses was used as a binary variable (use vs no use). AEs were classified according to the Medical Dictionary for Regulatory Activities (MedDRA; V.13.0) and summarised using the total number of AEs, the total number and percentage of patients who experience an AE, and the number of AEs over 100 patient-years (PYs). All AEs classified under the system organ class ‘infections and infestations’ were included in the infection analysis. Statistical analyses were conducted with SAS V.9.2 (SAS Institute, Cary, North Carolina, USA).
Results
Baseline demographics, disease parameters and concomitant medications
A total of 838 patients with 4582 assessments (mean (SD) interval of 6.0 (3.0) months) were included. Mean (SD) age was 55.6 (13.5) years, and disease duration at infliximab initiation (baseline) was 10.5 (9.8) years (table 1). The majority was female (74.7%), and had been previously treated with one or more traditional DMARDs (86.9%). At baseline, mean (SD) DAS28 was 5.4 (1.3), CDAI was 36.1 (16.1), TJC-28 was 12.5 (7.9), SJC-28 was 10.6 (7.0) and HAQ-DI was 1.7 (0.7). Concomitant corticosteroid use was reported for 38.2% of patients, most of whom (77.5%) were treated with >5 mg/day.
Table 1.
Patient demographics and baseline characteristics
| Parameter | Safety population N=838 |
ITT population N=628 |
|---|---|---|
| Sociodemographics | ||
| Females*, % | 74.7 | 73.6 |
| Age (years), mean (SD) | 55.6 (13.5) | 55.8 (13.6) |
| Geographical zone†, % | ||
| Eastern Canada | 73.4 | 76.1 |
| Central Canada | 6.1 | 6.1 |
| Western Canada | 20.4 | 17.8 |
| Enrolment period, % | ||
| 1/2002 to 6/2005 | 45.2 | 45.9 |
| 7/2005 to 6/2008 | 34.1 | 34.6 |
| 7/2008 to 6/2011 | 20.6 | 19.6 |
| Disease parameters | ||
| Comorbidity‡, % | 12.4 | 11.3 |
| Disease duration (years), mean (SD) | 10.5 (9.8) | 10.2 (10.0) |
| RF positive, %* | 73.4 | 73.8 |
| Family history of RA, %* | 33.7 | 33.3 |
| DAS28, mean (SD) | 5.4 (1.3) | 5.4 (1.3) |
| SDAI, mean (SD) | 38.2 (16.9) | 37.9 (16.9) |
| CDAI, mean (SD) | 36.1 (16.1) | 35.9 (16.3) |
| TJC-28, mean (SD) | 12.5 (7.9) | 12.5 (7.9) |
| SJC-28, mean (SD) | 10.6 (7.0) | 10.6 (7.1) |
| PhGA (VAS cm), mean (SD) | 6.6 (2.1) | 6.6 (2.1) |
| PtGA (VAS cm), mean (SD) | 6.1 (2.4) | 6.0 (2.4) |
| AM stiffness§ (min), mean (SD) | 70.9 (43.8) | 70.4 (43.6) |
| HAQ-DI, mean (SD) | 1.7 (0.7) | 1.7 (0.7) |
| Pain (VAS mm), mean (SD) | 57.7 (24.1) | 57.4 (24.3) |
| ESR (mm/h), mean (SD) | 32.2 (23.9) | 32.2 (24.0) |
| CRP (mg/L), mean (SD) | 19.2 (24.3) | 19.5 (24.9) |
| RA medications | ||
| Infliximab dose (mg), mean (SD) | 3.4 (0.5) | 3.4 (0.5) |
| Number of previous DMARDs, % | ||
| 0 | 13.1 | 13.2 |
| 1 | 20.8 | 21.7 |
| 2 | 28.8 | 27.9 |
| 3 | 20.0 | 20.7 |
| ≥4 | 17.3 | 16.6 |
| Concomitant DMARD, % | 89.7 | 91.1 |
| Concomitant methotrexate, % | 70.4 | 72.1 |
| Concomitant corticosteroid use, % | ||
| No use | 61.8 | 61.8 |
| ≤5 mg/day | 7.9 | 8.1 |
| >5 mg/day | 29.5 | 29.6 |
| Missing dose | 0.8 | 0.6 |
| Corticosteroid dose¶, mean (SD) | 9.3 (11.0) | 9.3 (11.8) |
*Percentages based on responders.
†The geographical zone was categorised as: East=Maritimes, Ontario and Quebec; Central=Manitoba and Saskatchewan; West=Alberta and British Colombia.
‡Proxy based on the use of concomitant medications.
§Capped at 120 min.
¶Among patients taking a corticosteroid who had available information.
CDAI, Clinical Disease Activity Index; CRP, C reactive protein; DAS28, disease activity score 28; DMARD, disease-modifying antirheumatic drug; ESR, erythrocyte sedimentation rate; HAQ-DI, health assessment questionnaire disability index; ITT, intent to treat; PhGA, physician's global assessment; PtGA, patient's global assessment; RA, rheumatoid arthritis; RF; SDAI, Simplified Disease Activity Index; SJC, swollen joint count; TJC, tender joint count; VAS, visual analogue scale.
Incidence of infections
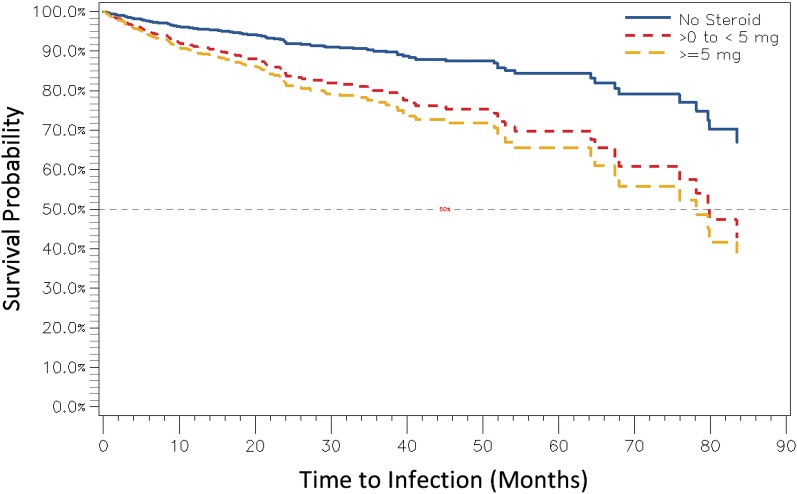
After a mean Kaplan-Meier-based duration of follow-up of 51.3 months, the incidence of total (non-serious and serious) AEs was 110.2 per 100 PYs, and the incidence of serious AEs was 8.5 per 100 PYs. The overall incidence rate of total infections and serious infections was 19.6 per 100 PYs and 2.0 per 100 PYs (1.3 per 100 PYs resulting in hospitalisation), respectively. On adjusting for enrolment period, baseline age and disease duration, number of prescriptions, and HAQ-DI, the HR (95% CI) for acquiring an infection was 2.48 (1.24 to 4.98) in patients treated with >5 mg/day of corticosteroids compared with patients not receiving corticosteroids (p=0.011; figure 1). Treatment with ≤5 mg/day of corticosteroids was associated with an increased hazard for infection (HR (95% CI)=2.12 (0.97 to 4.66), p=0.146), which approached but did not reach statistical significance (p=0.061). Additional factors associated with higher infection risk were increased HAQ-DI (HR (95% CI)=1.51 (1.15 to 1.92)), longer baseline disease duration (HR (95% CI)=1.01 (1.00 to 1.03)), and later enrolment period (HR2005–2008 vs 2002–2005: (95% CI)=2.99 (1.96 to 4.56), p<0.001; HR2008–2011 vs 2002–2005: (95% CI)=4.24 (2.56 to 7.02), p<0.001). Notably, the later enrolment period has been previously associated with less severe disease at initiation of treatment with infliximab.18
Figure 1.
Time to infection by steroid use. Month 0 corresponds to the time of inclusion in the cohort.
Corticosteroid use at disease remission
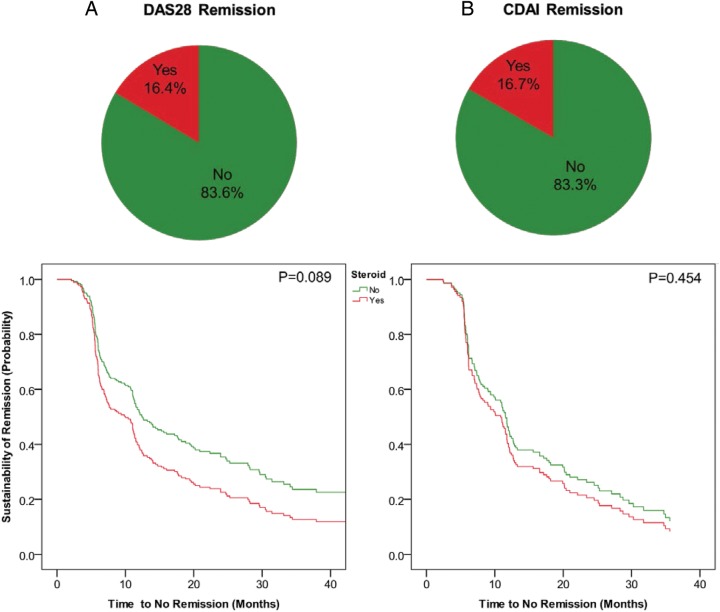
After a mean (SD) follow-up of 29.3 (22.9) months, remission, as defined by DAS28 and CDAI, was achieved by 46.5% and 30.4% of patients, respectively. Despite achievement of DAS28 or CDAI remission, corticosteroid use was continued in 16.4% and 16.7% of cases of the ITT population, respectively (figure 2), as compared with 34.2% and 33.5% who were treated with a corticosteroid at baseline. In approximately half (DAS28 48.2%; CDAI 48.3%) of these remission cases, a >5 mg/day dose of corticosteroid was administered. Although not statistically significant, corticosteroid use at the time of remission was higher in earlier compared with later years (2002–2005 vs 2005–2008 vs 2008–2011) both for DAS28 (22.2% vs 15.8% vs 13.6%; p=0.356) and CDAI (20.8% vs 15.8% vs 15.8%; p=0.829). DMARD use and methotrexate (MTX) dose at the time of DAS28 remission (DMARD 90.2% vs 95.2%, p=0.132; MTX 19.0 vs 18.3 mg/week, p=0.811) and CDAI remission (DMARD 100.0% in both groups; MTX 18.5 vs 18.6 mg/week, p=0.980) were comparable between patients using versus not using a corticosteroid at remission (table 2). Similarly, no statistical differences were observed between groups in baseline age, disease duration, and concomitant DMARD use at baseline; however, patients still on a corticosteroid at the time of DAS28 (72.1% vs 14.7%; p<0.001) and CDAI (64.1% vs 15.1%; p<0.001) remission were more likely to have been on a >5 mg/day dose corticosteroid at baseline.
Figure 2.
Steroid use among remission cases and impact on sustainability of remission. Month 0 corresponds to the time of inclusion in the cohort (CDAI, Clinical Disease Activity Index; DAS28, disease activity score 28).
Table 2.
Patient characteristics by steroid use at remission
| Parameter | On steroid While at remission |
Not on steroid While at remission |
p Value |
|---|---|---|---|
| DAS28 remission | |||
| At remission | |||
| Concomitant DMARD, % | 90.2 | 95.2 | 0.132 |
| Methotrexate dose, mg/week, mean (SD) | 19.0 (4.5) | 18.3 (14.0) | 0.811 |
| Concomitant corticosteroid use, % | |||
| No use | 0.0 | 100.0 | NC |
| ≤5 mg/day | 51.8 | 0.0 | |
| >5 mg/day | 48.2 | 0.0 | |
| Corticosteroid dose*, mean (SD) | 6.2 (3.0) | NA | NC |
| At baseline | |||
| Age (years), mean (SD) | 57.9 (13.2) | 55.0 (13.8) | 0.419 |
| Disease duration (years), mean (SD) | 10.0 (9.4) | 9.2 (9.4) | 0.821 |
| Concomitant DMARD, % | 90.2 | 93.9 | 0.299 |
| Concomitant corticosteroid use, % | |||
| No use | 8.2 | 81.0 | <0.001 |
| ≤5 mg/day | 18.0 | 4.3 | |
| >5 mg/day | 72.1 | 14.7 | |
| Missing dose | 1.6 | 0.0 | |
| Corticosteroid dose*, mean (SD) | 8.0 (4.6) | 10.1 (21.6) | 0.499 |
| CDAI remission | |||
| At remission | |||
| Concomitant DMARD, % | 100.0 | 100.0 | NC |
| Methotrexate dose†, mg/week, mean (SD) | 18.5 | 18.6 | 0.980 |
| Concomitant corticosteroid use, % | |||
| No use | 0.0 | 100.0 | NC |
| ≤5 mg/day | 51.7 | 0.0 | |
| >5 mg/day | 48.3 | 0.0 | |
| Corticosteroid dose*, mean (SD) | 5.6 (5.8) | NA | NC |
| At baseline | |||
| Age (years), mean (SD) | 58.1 (13.9) | 54.1 (13.7) | 0.675 |
| Disease duration (years), mean (SD) | 9.9 (8.2) | 8.7 (9.1) | 0.480 |
| Concomitant DMARD, % | 92.3 | 95.4 | 0.440 |
| Concomitant corticosteroid use, % | |||
| No use | 10.3 | 80.9 | <0.001 |
| ≤5 mg/day | 23.1 | 3.9 | |
| >5 mg/day | 64.1 | 15.1 | |
| Missing dose | 2.6 | 0.0 | |
| Corticosteroid dose*, mean (SD) | 8.0 (4.2) | 6.3 (5.3) | 0.175 |
*Among patients taking a corticosteroid who had available information.
†Among users.
CDAI, Clinical Disease Activity Index; DAS28, disease activity score 28; DMARD, disease-modifying antirheumatic drug; NA, not applicable; NC, not calculable.
Impact of continued corticosteroid use on remission sustainability and infection
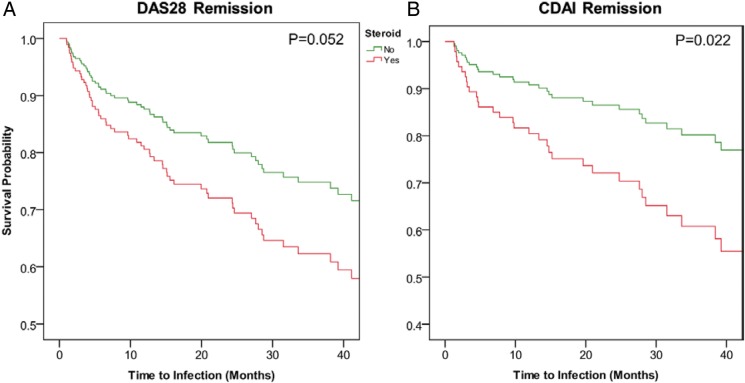
Among patients achieving disease remission, survival analysis did not show a significant positive effect of continued corticosteroid use on sustainability of remission (figure 2). The HR (95% CI) for sustaining DAS28 remission (time to no remission) was 1.40 (0.95 to 2.06) in patients using versus not using corticosteroids. The HR (95% CI) for sustaining CDAI remission was 1.19 (0.75 to 1.88). Age and disease duration were not associated with sustainability of remission. Time to acquiring an infection, however, was significantly shorter among patients treated with a corticosteroid when compared with the absence of corticosteroid treatment (HRDAS28 (95% CI)=1.78 (1.00 to 3.19); HRCDAI (95% CI)=2.38 (1.14 to 4.99); figure 3).
Figure 3.
Time to infection by continued steroid use. Month 0 corresponds to the time of inclusion in the cohort (CDAI, Clinical Disease Activity Index; DAS28, disease activity score 28).
Discussion
Baseline concomitant steroid administration, reported for 38.2% of patients, was comparable with previously reported Canadian estimations of 30–40%,13–15 and the majority of these patients (approximately 80%) were administered ≥5 mg/day of corticosteroids based on the Canadian standard practices, for an overall mean (SD) dose of 9.3 (11.8) mg/day.
Overall, treatment with a systemic corticosteroid was identified as an independent predictor of infection in patients treated with infliximab: ≥5 mg/day administration conferred a 2.5-fold increase in the odds of occurrence of infection compared with patients not receiving systemic corticosteroids, and ≤5 mg/day was associated with a 2.1-fold increase. Although the latter increase in the risk for infection with ≤5 mg/day of corticosteroids was not statistically significant, this might be due to lack of statistical power. These results are comparable with previously reported data, which have shown a dose-dependent effect of systemic corticosteroid use on development of infection in patients with RA treated with anti-TNF-α therapy,3 9 8 and non-biological DMARDs.4 Based on data from the German biologics registry, RABBIT, showing a twofold to fourfold increased risk in serious infections when using corticosteroid doses ≥7.5 mg/day, the RABBIT risk score, a valuable instrument determining the risk of serious infections in individual patients based on clinical and treatment information, takes corticosteroid use into consideration.18 Furthermore, although established guidelines recommend that corticosteroids for the treatment of RA be administered in the lowest possible dose and tapered as early as possible, their use extending past achievement of DAS28 or CDAI remission occurred in 16.4% and 16.7% of patients, respectively, where >5 mg/day administration accounted for approximately half of these cases. This continued administration, however, was not associated with a significant positive effect on sustainability of remission: time to no remission was 1.4-fold and 1.2-fold higher in patients treated with systemic corticosteroids (DAS28 and CDAI remission, respectively). In addition to conferring impaired sustentation of remission, use of systemic corticosteroids was also significantly associated with a decrease in time to acquiring of an infection, where use versus no use resulted in a 1.8-fold and 2.4-fold increase in the chance of development of infection in patients having achieved DAS28 and CDAI remission, respectively.
With regard to patient characteristics associated with the continuation of corticosteroid use into remission, neither age, disease duration, nor concomitant DMARD use were identified as predictors. However, although not statistically significant, corticosteroid use at the time of remission was higher in earlier (approximately 20% in 2002) compared with later (approximately 15% in 2011) years. This may be a reflection of changes in physician awareness and evolving clinical practice: the 2002 update of the ACR guidelines for the treatment of RA recommended, although cautiously, that for patients functionally dependent on glucocorticoids for long-term disease control, administration could be kept to a minimum.19 Similarly, the 2007 EULAR recommendations, somewhat more accurately reflecting current guidelines, recommended the use of systemic corticosteroids as an (mainly temporary) adjunct to DMARD strategy due to risk of side effects.20 Additionally, the history of corticosteroid use for the treatment of RA has been marked by contradictory arguments with regard to benefits in terms of symptomatic control and prevention of radiographic progression, and disadvantages related to AEs following long-term use resulting in dichotomous views of their role in management of RA.1 2 21 Only the most recent guidelines have explicitly recommended that systemic corticosteroid use be limited in duration and dose.11 12 Implications of this gradual paradigm shift may therefore be responsible for the gradual tapering of postremission systemic corticosteroid use observed over time.
Serious infections are one of the main reasons of increased mortality in RA.22 23 Although a meta-analysis of randomised trials found the anti-TNF agents, infliximab and adalimumab, to be associated with increased risk of infection,24 the results of this, and other studies, confirm that treatment with a corticosteroid is an independent predictor of infection in patients treated with an anti-TNF treatment regimen,3 8 9 and should be considered in interpretation of safety data. Additionally, this analysis has identified that, despite the current RA treatment guidelines, over 15% of patients continue systemic use of corticosteroids past achievement of remission, to the detriment of remission sustentation, and with an associated decrease in time-to-infection acquisition. Consequently, use of systemic corticosteroids in a real-world Canadian clinical setting lowers the associated risk–benefit ratio, whereas careful timing and administration could, over time, reduce risks for infection and mortality.
Although this study supports the association between systemic corticosteroid use and risk of infection, a low incidence of serious infections population (2.0 per 100 PYs) was observed in the overall population, compared with previously published data: Grijalva et al9 recently reported for patients with RA treated with infliximab, a rate of 10.3 serious infections per 100 PYs. Subsequently, due to a low number of events, association of corticosteroid use with serious infections/different types of infections was not possible. A possible explanation for the discrepancy in incidences of serious infections between studies is the method of data collection. Grijalva et al relied on insurance claims forms, which ensures accurate and detailed disease history and specifics, whereas this study recommended patient assessment at 6-month intervals, possibly resulting in an underestimation of actual corticosteroid use due to incomplete patient data, and of the actual incidence of serious infections due to recall bias. An additional limitation of our study relates to the fact that the presence of comorbidity at baseline was assessed using concomitant medications as proxy which may have resulted in the underestimation of the prevalence of comorbid conditions.
Among the strengths of the current study, as compared with the use of administrative databases, are the availability of granular data on the dosing of steroids and other concomitant RA medications, and on the timing of remission, as well as the inclusion in the registry of validated RA cases, and the use of validated RA disease activity measures.
Treatment with a corticosteroid was associated with an increased risk for acquiring an infection without having an impact on sustainability of remission. These results support the recommendations of the CRA and EULAR that corticosteroids should be used concomitantly with anti-TNF treatment for the shortest period possible to achieve remission, but not thereafter.
Footnotes
Funding: Study financed by Janssen Inc.
Competing interests: BH: research grants, advisory boards and speaker's bureau: AbbVie, Amgen, BMS, Celgene, Janssen, Pfizer, Roche, UCB. AJ: consulting fees: AbbVie, AstraZeneca, Amgen, Janssen, Lilly, Pfizer, Roche, UCB, Takeda. WGB: grants and/or honoraria for his roles as investigator and/or consultant: Abbott, AbbVie, Amgen, AstraZeneca, Bristol-Myers Squibb, Celgene, Janssen, Eli Lilly, Merck-Shering, Novartis, Pfizer, Roche, Servier, UCB, Warner Chilcott, Wyeth. RF: speaker: Roche, Janssen, Pfizer, Amgen. Research grants: Roche, Pfizer, Janssen. Advisory board: Roche, Janssen, Amgen. JK: grants and/or honoraria: Abbott, Amgen, Merck Schering, Janssen. SD: grants and/or honoraria for his roles as investigator and/or consultant: Abbott, AstraZeneca, Bristol-Myers Squibb, Merck-Schering, Janssen, Lilly, Pfizer, Wyeth, Roche, Takeda, UCB. JR: consultant for advisory board of Janssen. MS: grants and/or honoraria for his roles as investigator and/or consultant: AbbVie, Janssen, Amgen, Bristol-Myers Squibb, UCB. ER and JSS: employees of JSS Medical Research, the CRO hired. AJL, SO, FN, MS: employees of Janssen Inc.
Patient consent: Obtained.
Ethics approval: Ethics approval for participation in the BioTRAC programme was obtained from the respective Research Ethics Boards of the participating institutional sites and a Central Institutional Review Board (IRB Services, Ontario Canada) for private practice sites.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Caplan L, Wolfe F, Russell AS et al. . Corticosteroid use in rheumatoid arthritis: prevalence, predictors, correlates, and outcomes. J Rheumatol 2007;34:696–705. [PubMed] [Google Scholar]
- 2.Hoes JN, Jacobs JW, Buttgereit F et al. . Current view of glucocorticoid co-therapy with DMARDs in rheumatoid arthritis. Nat Rev Rheumatol 2010;6:693–702. 10.1038/nrrheum.2010.179 [DOI] [PubMed] [Google Scholar]
- 3.Wolfe F, Caplan L, Michaud K. Treatment for rheumatoid arthritis and the risk of hospitalization for pneumonia: associations with prednisone, disease-modifying antirheumatic drugs, and anti-tumor necrosis factor therapy. Arthritis Rheum 2006;54:628–34. 10.1002/art.21568 [DOI] [PubMed] [Google Scholar]
- 4.Lacaille D, Guh DP, Abrahamowicz M et al. . Use of nonbiologic disease-modifying antirheumatic drugs and risk of infection in patients with rheumatoid arthritis. Arthritis Rheum 2008;59:1074–81. 10.1002/art.23913 [DOI] [PubMed] [Google Scholar]
- 5.Doran MF, Crowson CS, Pond GR et al. . Predictors of infection in rheumatoid arthritis. Arthritis Rheum 2002;46:2294–300. 10.1002/art.10529 [DOI] [PubMed] [Google Scholar]
- 6.Curtis JR, Yang S, Patkar NM et al. . Risk of hospitalized bacterial infections associated with biologic treatment among US veterans with rheumatoid arthritis. Arthritis Care Res (Hoboken) 2014;66:990–7. 10.1002/acr.22281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Curtis JR, Patkar N, Xie A et al. . Risk of serious bacterial infections among rheumatoid arthritis patients exposed to tumor necrosis factor alpha antagonists. Arthritis Rheum 2007;56:1125–33. 10.1002/art.22504 [DOI] [PubMed] [Google Scholar]
- 8.Schneeweiss S, Setoguchi S, Weinblatt ME et al. . Anti-tumor necrosis factor alpha therapy and the risk of serious bacterial infections in elderly patients with rheumatoid arthritis. Arthritis Rheum 2007;56:1754–64. 10.1002/art.22600 [DOI] [PubMed] [Google Scholar]
- 9.Grijalva CG, Chen L, Delzell E et al. . Initiation of tumor necrosis factor-alpha antagonists and the risk of hospitalization for infection in patients with autoimmune diseases. JAMA 2011;306:2331–9. 10.1001/jama.2011.1692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Da Silva JA, Jacobs JW, Kirwan JR et al. . Safety of low dose glucocorticoid treatment in rheumatoid arthritis: published evidence and prospective trial data. Ann Rheum Dis 2006;65:285–93. 10.1136/ard.2005.038638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bykerk VP, Akhavan P, Hazlewood GS et al. . Canadian Rheumatology Association recommendations for pharmacological management of rheumatoid arthritis with traditional and biologic disease-modifying antirheumatic drugs. J Rheumatol 2012;39:1559–82. 10.3899/jrheum.110207 [DOI] [PubMed] [Google Scholar]
- 12.Smolen JS, Landewe R, Breedveld FC et al. . EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2013 update. Ann Rheum Dis 2014;73:492–509. 10.1136/annrheumdis-2013-204573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McKeown E, Bykerk VP, De LF et al. . Quality assurance study of the use of preventative therapies in glucocorticoid-induced osteoporosis in early inflammatory arthritis: results from the CATCH cohort. Rheumatology (Oxford) 2012;51:1662–9. 10.1093/rheumatology/kes079 [DOI] [PubMed] [Google Scholar]
- 14.Dixon WG, Abrahamowicz M, Beauchamp ME et al. . Immediate and delayed impact of oral glucocorticoid therapy on risk of serious infection in older patients with rheumatoid arthritis: a nested case-control analysis. Ann Rheum Dis 2012;71:1128–33. 10.1136/annrheumdis-2011-200702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.vina-Zubieta JA, Abrahamowicz M, De Vera MA et al. . Immediate and past cumulative effects of oral glucocorticoids on the risk of acute myocardial infarction in rheumatoid arthritis: a population-based study. Rheumatology (Oxford) 2013;52:68–75. 10.1093/rheumatology/kes353 [DOI] [PubMed] [Google Scholar]
- 16.Public Health Agency of Canada. Life with Arthritis in Canada: A personal and public health challenge. 2010. http://www.phac-aspc.gc.ca/cd-mc/arthritis-arthrite/lwaic-vaaac-10/pdf/arthritis-2010-eng.pdf (accessed Nov 2014). [Google Scholar]
- 17.Thorne C, Bensen WG, Choquette D et al. . Effectiveness and safety of infliximab in rheumatoid arthritis: analysis from a Canadian multicenter prospective observational registry. Arthritis Care Res (Hoboken) 2014;66:1142–51. 10.1002/acr.22290 [DOI] [PubMed] [Google Scholar]
- 18.Strangfeld A, Eveslage M, Schneider M et al. . Treatment benefit or survival of the fittest: what drives the time-dependent decrease in serious infection rates under TNF inhibition and what does this imply for the individual patient? Ann Rheum Dis 2011;70:1914–20. 10.1136/ard.2011.151043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.American College of Rheumatology Subcommittee on Rheumatoid Arthritis Guidelines. Guidelines for the management of rheumatoid arthritis: 2002 update. Arthritis Rheum 2002;46:328–46. 10.1002/art.10148 [DOI] [PubMed] [Google Scholar]
- 20.Combe B, Landewe R, Lukas C et al. . EULAR recommendations for the management of early arthritis: report of a task force of the European Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Ann Rheum Dis 2007;66:34–45. 10.1136/ard.2005.044354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Caplan L, Russell AS, Wolfe F. Steroids for rheumatoid arthritis: the honeymoon revisited (once again). J Rheumatol 2005;32:1863–5. [PubMed] [Google Scholar]
- 22.Thomas E, Symmons DP, Brewster DH et al. . National study of cause-specific mortality in rheumatoid arthritis, juvenile chronic arthritis, and other rheumatic conditions: a 20 year followup study. J Rheumatol 2003;30:958–65. [PubMed] [Google Scholar]
- 23.Sihvonen S, Korpela M, Laippala P et al. . Death rates and causes of death in patients with rheumatoid arthritis: a population-based study. Scand J Rheumatol 2004;33:221–7. 10.1080/03009740410005845 [DOI] [PubMed] [Google Scholar]
- 24.Bongartz T, Sutton AJ, Sweeting MJ et al. . Anti-TNF antibody therapy in rheumatoid arthritis and the risk of serious infections and malignancies: systematic review and meta-analysis of rare harmful effects in randomized controlled trials. JAMA 2006;295:2275–85. 10.1001/jama.295.19.2275 [DOI] [PubMed] [Google Scholar]