Abstract
A 63-year-old woman with abdominal pain and melena developed a palpable, purpuric rash and acute kidney injury. Skin and kidney biopsy confirmed Henoch-Schönlein purpura. Upper endoscopy revealed diffuse, circumferential, black-appearing mucosa of the esophagus consistent with acute esophageal necrosis (AEN), also known as black esophagus. AEN is a very rare cause of gastrointestinal hemorrhage with a high mortality risk. To our knowledge, there have been no prior reports of AEN associated with Henoch-Schonlein purpura or other vasculitis.
Introduction
Acute esophageal necrosis (AEN), also known as black esophagus, is a rare clinical condition diagnosed based on characteristic endoscopic findings. It appears as diffuse, circumferential, black-appearing mucosa of the esophagus.1,2 The most common clinical presentation of AEN is gastrointestinal bleeding and it is associated with a significant morbidity and mortality.
Case Report
A 63-year-old woman with a history of multiple comorbidities including a kidney transplant, type II diabetes mellitus, and peripheral artery disease presented with 2 weeks of worsening abdominal pain, diarrhea, nausea, and vomiting. She also described multiple episodes of melena in the 3 days prior to hospitalization. She had symptoms of gastroesophageal reflux in the past and underwent an upper endoscopy 3 years prior that was normal. Since then, her symptoms have been well-controlled and she stopped taking a proton-pump inhibitor 1 year ago.
On presentation, the patient was found to have acute kidney injury with a creatinine of 4.2 mg/dL and anemia with a hemoglobin of 10.3 g/dL. She denied any sick contacts, recent travel, or fevers. One day prior to admission, a palpable, purpuric rash appeared on her extremities and involved the palms of her hands and soles of her feet. Her vital signs remained stable throughout her hospitalization. A non-contrast abdominal CT scan demonstrated a thick-walled, inflamed proximal jejunum, but was otherwise unremarkable. On upper endoscopy, the patient had necrotic-appearing panesophagitis and severely ulcerated, necrotic duodenitis involving the second and third portions of the duodenum (Figure 1).
Figure 1.
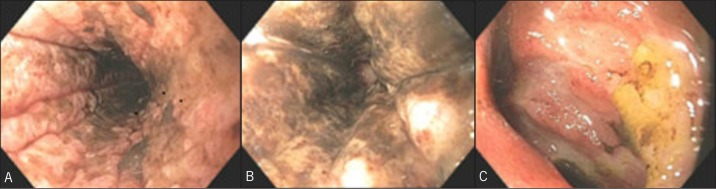
Initial upper endoscopy showing necrotic-appearing panesophagitis in the (A) upper third and (B) lower third of esophagus, and (C) severely ulcerated, necrotic duodenitis in the second portion of duodenum.
No infectious cause was identified, stool culture grew normal fecal flora, and blood cultures remained negative. Cytomegalovirus was not detected by culture or PCR, and acute hepatitis panel and HIV testing were negative. Biopsies of the esophagus showed fragments of granulation tissue consistent with ulceration. Duodenal biopsies revealed vasculitis and ischemic enteritis with ulceration. There was neutrophil infiltration into the vessel walls in the submucosa.
The skin rash spread from her hands in a centripetal manner to involve the chest and thorax during the first day of her hospitalization (Figure 2). Skin biopsy revealed perivascular neutrophil infiltration of the upper dermis with neutrophilic degeneration, fibrin exudation, destruction of the vascular wall, and intravascular thrombi, consistent with leukocytoclastic vasculitis. A kidney biopsy was also performed and demonstrated proliferative glomerulonephritis and advanced interstitial fibrosis and tubular injury, with IgA and C3 deposition. Serum rheumatoid factor was negative. IgA was elevated at 633 mg/dL (normal: 85–385 mg/dL) and IgM was reduced at 24 mg/dL (normal: 45–250 mg/dL), while IgG was normal. C4 was normal and C3 was reduced at 67.5 mg/dL (normal: 70–176 mg/dL). Based on these findings and both gastrointestinal and renal involvement, the patient was diagnosed with Henoch-Schönlein purpura (HSP). Treatment with intravenous methylprednisolone was initiated. Her rash rapidly improved; however, she did require hemodialysis for oliguric renal failure. The AEN was managed conservatively with proton pump inhibitors. She required parenteral nutrition until her oral intake improved. A repeat endoscopy 9 days later revealed a diffuse and circumferential, pale yellow fibrinous layer in the esophagus and slightly improved ischemic duodenitis in the second portion of the duodenum (Figure 3).
Figure 2.

Palpable, purpuric rash on the patient's (A) right thigh and torso and (B) hand.
Figure 3.
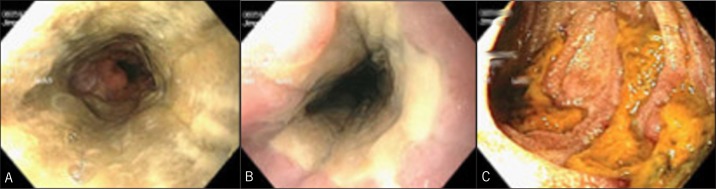
Repeat upper endoscopy 9 days after presentation showing improvement in the (A) upper third of esophagus, (B) lower third of esophagus, and (C) second portion of duodenum.
Discussion
The overall incidence of AEN is very low, between 0.01 and 0.28%.3 AEN characteristically involves the distal esophagus with variable extension proximally. The etiology likely involves tissue hypoperfusion, corrosive gastric reflux, diminished immune defenses, or infection.1,2,4 Based on prior case series, the most common presentation is upper gastrointestinal bleeding.2,4 Risk factors for developing AEN include cardiovascular disease, diabetes mellitus, chronic kidney disease, and cancer.1,2,4 Complications of AEN include esophageal stricture formation and rare esophageal perforation. The overall mortality is high and exceeds 30%.2,4 It has been postulated that the proximal extent of esophageal injury correlates with duodenal involvement, which may relate to the common blood supply from the celiac axis.1 HSP is a small-vessel disease with primarily dermal, renal, joint, and gastrointestinal tract involvement. It most commonly affects children.5 A retrospective study of gastrointestinal presentation of HSP reported mucosal erythema, edema, ulcers, and nodules on upper endoscopy, with the second portion of the duodenum most frequently involved.6
Although we are unable to definitively say that HSP was the direct cause of AEN, based on the patient's clinical presentation, it was a highly relevant factor. To our knowledge, this case is the first report of HSP presenting with AEN. This patient had several known comorbidities, which have been documented as risk factors for AEN, including chronic renal insufficiency and diabetes. She did not have any evidence of infection or hemodynamic instability on presentation. A potential mechanism may be ischemia and necrosis caused by inflammation of vessels and mucosal edema.
Disclosures
Author contributions: N. Iorio reviewed the literature and wrote the manuscript. GR Bernstein and Z. Malik wrote and edited the manuscript. R. Schey revised and reviewed the manuscript, and is the article guarantor.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
References
- 1.Gurvits GE, Cherian K, Shami MN, et al. Black esophagus: New insights and multicenter international experience in 2014. Dig Dis Sci. 2015;60(2):444–53. [DOI] [PubMed] [Google Scholar]
- 2.Gurvits GE, Shapsis A, Lau N, et al. Acute esophageal necrosis: A rare syndrome. J Gastroenterol. 2007;42(1):29–38. [DOI] [PubMed] [Google Scholar]
- 3.Ben Soussan E, Savoye G, Hochain P, et al. Acute esophageal necrosis: A 1-year prospective study. Gastrointest Endosc. 2002;56(2):213–7. [DOI] [PubMed] [Google Scholar]
- 4.Grudell AB, Mueller PS, Viggiano TR. Black esophagus: Report of six cases and review of the literature, 1963-2003. Dis Esophagus. 2006;19(2):105–10. [DOI] [PubMed] [Google Scholar]
- 5.Alvarez-Caro F, Concha-Torre JA, García-Hernández I. Massive lower gastrointestinal haemorrhage, successfully treated with corticosteroids, as main symptom of Schönlein-Henoch purpura. Rheumatol Int. 2009;29(12):1491–4. [DOI] [PubMed] [Google Scholar]
- 6.Zhang Y, Huang X. Gastrointestinal involvement in Henoch-Schönlein purpura. Scand J Gastroenterol. 2008;43(9):1038–43. [DOI] [PubMed] [Google Scholar]


