Abstract
Choledochal cyst is prevalent in female than male. Diagnosis and management of choledochal cyst is important in clinical practice, or else, patients may develop cholangiocarcinoma. Currently, complete resection is the standard method for the treatment of choledochal cyst. However, traditional open surgery is usually needed in these procedures, which may induce postoperative injuries. In this case, we present our experiences for the management of choledochal cyst through radical removal combined with Roux-en-Y anastomosis under laparoscope. Our procedures are minimally invasive and the outcomes are satisfactory during the follow up.
Keywords: Choledochal cyst, Roux-en-Y anastomosis, surgery
Introduction
Choledochal cyst, a common type of congenital mal-development of biliary tract, is more prevalent in female [1]. Diagnosis and management of choledochal cyst is important in clinical practice as patients may develop cholangiocarcinoma [2]. In the past decades, choledochal cyst was mainly reported in young girls [3]. Recent studies suggest that a large number of adults present with such disease [1,4].
To date, removal cyst combined with Roux-en-Y anastomosis has been well acknowledged as the standard treatment strategy [5,6]. In these procedures, traditional open surgery is usually needed, which may induce postoperative injuries. Therefore, in clinical practice, we have been focusing on treating choledochal cyst using minimally invasive techniques with no undermining of the outcome. In this case, we present our experiences for the management of choledochal cyst through radical removal combined with Roux-en-Y anastomosis under laparoscope. Our study reveals the procedure is effective for treating choledochal cyst.
Case report
Case 1 was a female aged 22 years old, who was admitted to our hospital due to choledochal cyst, confirmed by enhanced contrast CT and magnetic resonance cholangiopancreatography (MRCP). No abnormalities were noted in the liver function, bilirubin and tumor markers (Figure 1).
Figure 1.
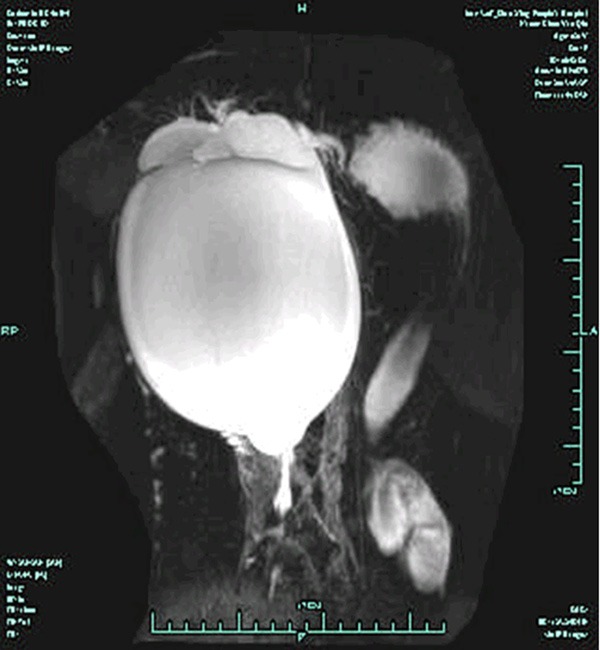
MRCP imaging of the choledochal cyst in Case 1. T2W indicated significant dilation of the common bile duct in a ball-like profile with a size of 160 × 150 mm. No significant dilation was observed in the intra-hepatic bile duct.
Case 2 was a female aged 54 years old. She was diagnosed with choledochal cyst through ultrasound examination. The patient’s complaint of pain was in right upper quadrant of the abdomen. The liver function was normal, together with the concentration of bilirubin and tumor markers (Figure 2).
Figure 2.
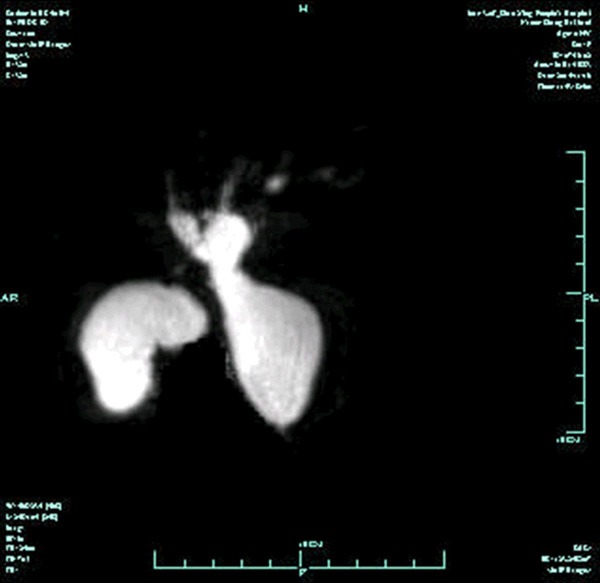
MRCP imaging of the choledochal cyst in Case 2. T2W indicated significant dilation of the common bile duct in a ball-like profile with a size of 35 × 30 mm. Slight dilation was observed in the intra-hepatic bile duct and common hepatic duct. The inferior segment of the common bile duct in proximity to the duodenum opening was narrowed.
Case 3 was also a female aged 44 years old who presented to our hospital due to vague pain in right upper quadrant of abdomen for 6 months (Figure 3).
Figure 3.
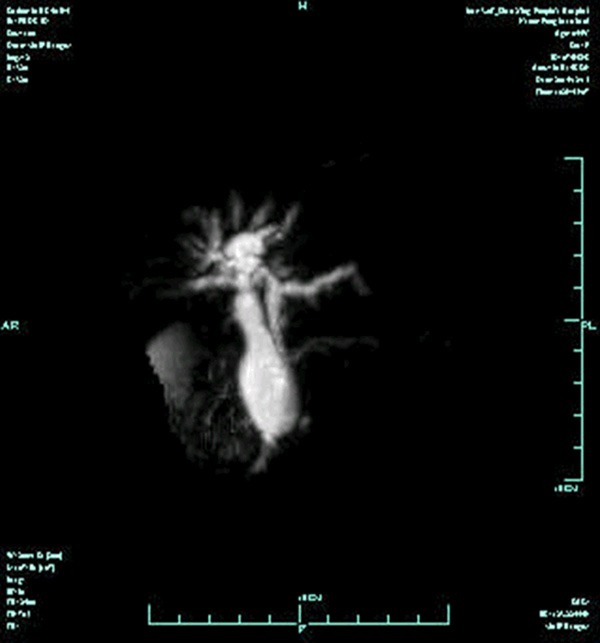
MRCP imaging of the choledochal cyst in Case 3. T2W indicated fusiform dilatation in the middle and upper segment of common bile duct with the largest width of 25 mm approximately. The inferior segment of the common bile duct was significantly narrowed.
After anesthesia, the patient was in a supine position. For the laparoscopic surgery, four incisions were made in total. One incision was made at the umbilical part for the insertion of the camera, two incisions at the right rectus abdominis parallel to the umbilicus, and one incision at the right anterior axillary line. The pneumoperitoneum pressure was maintained at 12-15 mmHg. For the surgery, the ligamentum teres hepatis was cut off and ligated using a 2-0 suture at the root. Afterwards, an incision about 2 mm in length was made beneath the xiphoid process. Subsequently, the hepatoduodenal ligament was isolated to expose the choledochal cyst. For the cyst with a large dimension, decompression was performed at the anterior wall of the cyst. For the cyst with a moderate or small dimension, the bile duct was completely isolated at the anterior part of the portal vein, followed by ligation using a 2.0 suture. Subsequently, the cyst was cut off from the gallbladder.
Cholangiography was performed during the surgery to identify the distance between the stenosis and the duodenal papilla (Figure 4). Subsequently, the cyst was removed upon the protection of opening of pancreas. Upon the exposure of the Treitz’s ligament, the jejunum was dissected using a stitching instrument under the laparoscope at the position that was 15-20 cm beneath the Treitz’s ligament. Afterwards, the mesojejunum was opened using the ultrasound knife. The distal part of the jejunum loop was lifted to the first porta hepatis across the colon, and then an incision with similar diameter to the bile duct was made at the margin of the mesenterium. The anastomosis of the gallbladder and intestine was performed using 4-0 absorbable suture. Side-to-side anastomosis was performed to the distal and proximal end of the jejunum. Before the closure of the anastomotic stoma, a catheter was inserted to the anastomotic stoma of gallbladder and intestine. After distal occlusion, special cares were taken to prevent from leak. Finally, a drainage tube was inserted at the inferior part of the anastomotia stoma, and was led out from the right operating whole.
Figure 4.
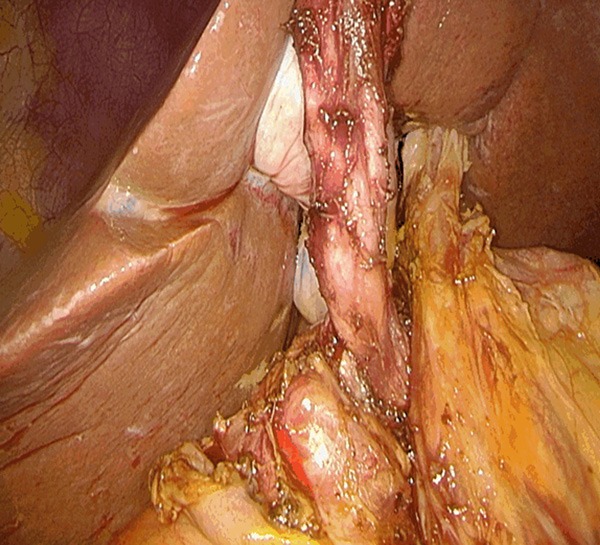
The whole picture of choledochal cyst. The superior border of the cyst was dissected at a position that was 1 cm to the bifurcation of the left/right hepatic duct. The inferior segment was isolated until reaching the bile duct localized at the pancreas.
The patients were discharged with satisfactory treatment outcome. Written informed consents were obtained from each patient. No gallbladder leak, postoperative bleeding or infection was reported during the 3-24 months follow up.
Discussion
Choledochal cyst has been commonly acknowledged as a precancerous lesion as patients may usually develop malignant carcinoma. Radical resection and Roux-en-Y anastomosis is the standard method for the management of congenital choledochal cyst. In 1995, video-guided laparoscopic treatment was initially used in clinical practice for the management of choledochal cyst [7]. In China mainland, increasing cases of such disease have been reported in children and teenagers [6,8]. However, rare studies on adults are available. In this case, we present the experiences of management of choledochal cyst in adults using the laparoscopic technique.
In our clinical experiences, we have been focusing on the management of choledochal cyst using laparoscope. Our experiences are summarized as follows: (i) The ligamentum teres hepatis was ligated using a suture, which contributed to the complete exposure of the first porta hepatis. In addition, such procedure could expand the surgical fields. (ii) Initially, the hepatoduodenal ligament was dissected to expose the cyst, based on which to identify the location of the bile duct and the conjunction of left/right hepatic duct. Afterwards, the bile duct was ligated using a suture in order to prevent the infection caused by leak of bile. On certain circumstances, a longitudinal incision should be made at the cystic wall to expose the cyst with a large dimension or those with unclear location of the bile duct or conjunction of left/right hepatic duct. (iii) Cholangiography was necessary for the removal of the distal cyst to ensure the distance between the bile duct and duodenal papilla. For the cyst very close to the duodenal papilla, measures should be taken to protect the integrity of the pancreatic duct. As pancreaticobiliary maljunction has been eliminated in the surgery, the tendency of malignancy was remarkably decreased. (iv) For the radical resection of cyst, the cyst should be cut off from the bile duct at a position that was 0.3-0.5 cm to the upper part. Meanwhile, part of the cystic wall should be kept in order to provide an appropriate stump, which contributed to the anastomosis of the gallbladder and intestinal tract, as well as reducing he chance of stenosis in the anastomotic stoma. (v) For the isolation of cystic wall, more attention should be paid to the blood vessels (with a diameter of more than 3 mm) of the cystic wall in proximity to the pancreas. To prevent the postoperative bleeding, vessel clamp was necessary. (vi) Special cares should be taken to prevent postoperative bile leak through pushing the ansa intestinalis to the porta hepatis during the knotting process. This procedure would decrease the tension during the suturing. (vii) Prior to the anastomosis of distal part and proximal part of the jejunum, a catheter should be inserted until the anastomosis of the gallbladder and intestine. Special cares should be taken to prevent leak in the anastomosis.
In the past decades, the accepted management method for choledochal cysts was drainage into the adjacent duodenum or stomach [9]. Subsequently, Roux-en-Y jejunal loop was used [10]. Nowadays, complete excision is recommended with the increase of the knowledge. To our knowledge, five types of choledochal cysts are available [1,11]. For patients with type I cysts, complete resection of cyst was performed together with reconstruction with a hepatic jejunostomy. For patients with type II cysts, solely resection was adequate. Unfortunately, the management efficiency for the other three types of choledochal cysts is still not well defined [11,12]. In this study, we present three cases of patients received resection and Roux-en-Y anastomosis under laparoscope. The surgery was minimally invasive, and no recurrence or postoperative complications were reported in the 3-24 months follow up.
Acknowledgements
This study was supported by the Talent Program of Medical Science of Zhejiang Province (group A, No. 2014RCA031).
Disclosure of conflict of interest
None.
References
- 1.De Vries JS, De Vries S, Aronson DC, Bosman DK, Rauws EA, Bosma A, Heij HA, Gouma DJ, Van Gulik TM. Choledochal cysts: age of presentation, symptoms, and late complications related to Todani’s classification. J Pediatr Surg. 2002;37:1568–1573. doi: 10.1053/jpsu.2002.36186. [DOI] [PubMed] [Google Scholar]
- 2.Franko J, Nussbaum ML, Morris JB. Choledochal cyst cholangiocarcinoma arising from adenoma: case report and a review of the literature. Curr Surg. 2006;63:281–284. doi: 10.1016/j.cursur.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 3.Kim OH, Chung HJ, Choi BG. Imaging of the choledochal cyst. Radiographics. 1995;15:69–88. doi: 10.1148/radiographics.15.1.7899614. [DOI] [PubMed] [Google Scholar]
- 4.Visser BC, Suh I, Way LW, Kang SM. Congenital choledochal cysts in adults. Arch Surg. 2004;139:855–862. doi: 10.1001/archsurg.139.8.855. [DOI] [PubMed] [Google Scholar]
- 5.Shimotakahara A, Yamataka A, Yanai T, Kobayashi H, Okazaki T, Lane GJ, Miyano T. Roux-en-Y hepaticojejunostomy or hepaticoduodenostomy for biliary reconstruction during the surgical treatment of choledochal cyst: which is better? Pediatr Surg Int. 2005;21:5–7. doi: 10.1007/s00383-004-1252-1. [DOI] [PubMed] [Google Scholar]
- 6.Shi LB, Peng SY, Meng XK, Peng CH, Liu YB, Chen XP, Ji ZL, Yang DT, Chen HR. Diagnosis and treatment of congenital choledochal cyst: 20 years experience in China. World J Gastroenterol. 2001;7:732–734. doi: 10.3748/wjg.v7.i5.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Farello GA, Cerofolini A, Rebonato M, Bergamaschi G, Ferrari C, Chiappetta A. Congenital choledochal cyst: video-guided laparoscopic treatment. Surg Laparosc Endosc. 1995;5:354–358. [PubMed] [Google Scholar]
- 8.Liuming H, Hongwu Z, Gang L, Jun J, Wenying H, Wong KK, Miao X, Qizhi Y, Jun Z, Shuli L. The effect of laparoscopic excision vs open excision in children with choledochal cyst: a midterm follow-up study. J Pediatr Surg. 2011;46:662–665. doi: 10.1016/j.jpedsurg.2010.10.012. [DOI] [PubMed] [Google Scholar]
- 9.Yamauchi Y, Hoshino S, Yamashita Y, Funamoto S, Ishida K, Shirakusa T. Successful resection of an infected duodenal duplication cyst after percutaneous cyst drainage: report of a case. Surg Today. 2005;35:586–589. doi: 10.1007/s00595-004-2968-1. [DOI] [PubMed] [Google Scholar]
- 10.Ure BM, Schier F, Schmidt AI, Nustede R, Petersen C, Jesch NK. Laparoscopic resection of congenital choledochal cyst, choledochojejunostomy, and extraabdominal Roux-en-Y anastomosis. Surg Endosc. 2005;19:1055–1057. doi: 10.1007/s00464-004-2191-6. [DOI] [PubMed] [Google Scholar]
- 11.Jordan PH, Goss JA, Rosenberg WR, Woods KL. Some considerations for management of choledochal cysts. Am J Surg. 2004;187:434–439. doi: 10.1016/j.amjsurg.2003.12.022. [DOI] [PubMed] [Google Scholar]
- 12.Stringer MD, Dhawan A, Davenport M, Mieli-Vergani G, Mowat AP, Howard ER. Choledochal cysts: lessons from a 20 year experience. Arch Dis Child. 1995;73:528–531. doi: 10.1136/adc.73.6.528. [DOI] [PMC free article] [PubMed] [Google Scholar]


