Abstract
Objective: The aim of this study is to evaluate the efficacy and feasibility of three-dimensional printing (3D printing) assisted internal fixation of unstable pelvic fracture from minimal invasive para-rectus abdominis approach. Methods: A total of 38 patients with unstable pelvic fractures were analyzed retrospectively from August 2012 to February 2014. All cases were treated operatively with internal fixation assisted by three-dimensional printing from minimal invasive para-rectus abdominis approach. Both preoperative CT and three-dimensional reconstruction were performed. Pelvic model was created by 3D printing. Data including the best entry points, plate position and direction and length of screw were obtained from simulated operation based on 3D printing pelvic model. The diaplasis and internal fixation were performed by minimal invasive para-rectus abdominis approach according to the optimized dada in real surgical procedure. Matta and Majeed score were used to evaluate currative effects after operation. Results: According to the Matta standard, the outcome of the diaplasis achieved 97.37% with excellent and good. Majeed assessment showed 94.4% with excellent and good. The imageological examination showed consistency of internal fixation and simulated operation. The mean operation time was 110 minutes, mean intraoperative blood loss 320 ml, and mean incision length 6.5 cm. All patients have achieved clinical healing, with mean healing time of 8 weeks. Conclusion: Three-dimensional printing assisted internal fixation of unstable pelvic fracture from minimal invasive para-rectus abdominis approach is feasible and effective. This method has the advantages of trauma minimally, bleeding less, healing rapidly and satisfactory reduction, and worthwhile for spreading in clinical practice.
Keywords: 3D printing, minimally invasive, pelvic fracture, internal fixation, para-rectus abdominis approach
Introduction
Though the incidence of unstable pelvic fractures is not well documented, they are associated with significant mortality and disability due to complications such as hemorrhagic shock [1-5]. Surgery has been advocated as the primary choice thanks to the absence of contraindications and hemodynamic instability [6]. However, the anatomical complexity of pelvic presents challenge to conventional surgery approach. Furthermore, conventional surgery may result in associated complications including wound infection and impaired wound healing. Numerous studies have demonstrated that rigid internal fixation can decrease the rate of post-trauma complications and improve functional outcomes.
Previous surgical treatments of pelvic fractures capitalize on existing iconographic technology to comprehend anatomical structure. However, lack of tactile experience may limit deep understanding of the complex anatomy even for a well-trained surgeon. The application of 3D printing technology in surgical realm has brought new opportunities for the treatment of unstable pelvic fracture. The simulation model of the pelvis facilitates both accurate judgment for fracture displacement and more reasonable operation scheme. In 2012, we have constructed 3D model of the exact anatomy of acetabulum in one patient with acetabular fracture. Because of our good experience in the first case, subsequent 38 cases with pelvic fractures were operated using this technology. Therefore, the aim of this study is to describe the technique and evaluate the clinical results using 3D printing assisted internal fixation operation from minimal invasive para-rectus abdominis approach [7].
Materials and methods
Patients
From August 2012 to February 2014, 38 cases with unstable pelvic fractures underwent surgical treatment. Among these cases, there were 25 male and 13 female cases. The age at the time of surgery was between 19 and 75 years old with an average of 32 years old; the mechanism of injury was car accident in 27 cases, high falling injury in 11 cases. Fractures were classified according to Tile’s classification of pelvic injuries [8]. There were 13 patients with type B, 15 patients with type C1, 8 patients with type C2, 2 patients with type C3. Concurrent injuries were Merger urethral injury in 5 cases, abdominal visceral injury in 8 cases, vaginal injury in 1 case, renal contusion in 1 case, femoral fracture in 2 cases, tibiofibula fracture in 4 cases, nerve injury in 2 cases, shock in 9 cases. After clinical evaluation and initial resuscitation, all patients had preoperative X-rays taken, pelvic CT thin layer scanned and 3D reconstructed.
Virtual simulation surgery
Patient pelvis is scanned by CT (0.6 mm thin); the scanned image is saved with the DICOM format. Mimics software was used for three-dimensional editing, virtual fracture reduction and optimization design. Multi-dimensional measurement determines the best location of implant reconstruction plate and screws, screw length and angle etc (Figure 1).
Figure 1.
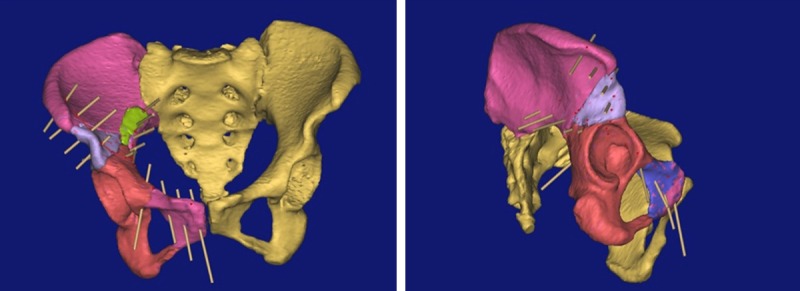
Virtual implantation of internal fixiation. A 44-year-old woman, pelvic fractures caused by high falling injury. Tile’s classification is type B. Preoperative digital virtual diaplasis and design of plate and screw are showed.
3D printing pelvic models for surgery simulation in vitro
First, data of three-dimensional fractured model was edited by Mimics software. Then, data was exported to 3D printer and fractured pelvic simulation model was fabricated (Figure 2). Afterwards, the 3D model was used to perform virtual surgery, i.e. steel plate pre-bent. We confirmed and corrected the data from Mimics software virtual surgery.
Figure 2.
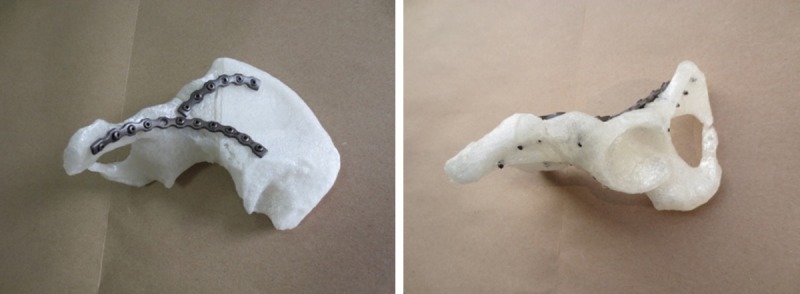
Simulated operation by 3D printed pelvic model. Bending plates on the reduction model find its design position; Fixing plates on the reduction models. The model came from the patient showed in Figure 1.
Surgical procedure
All patients with unstable pelvic fracture were performed surgery operation of internal fixation from minimal invasive para-rectus abdominis approach 5 to 10 days after injury General anesthesia or epidural anesthesia were used. The length of the skin incision is 5~8 cm. The operation procedures were implemented in accordance with the one we had confirmed in the virtual and simulation operation (Figure 3). During the process of operation, it is important to identify and ligate anastomosis (death cap) between inferior epigastric artery or external iliac vessels and obturator so as to put steel plate or screws into a safety place.
Figure 3.
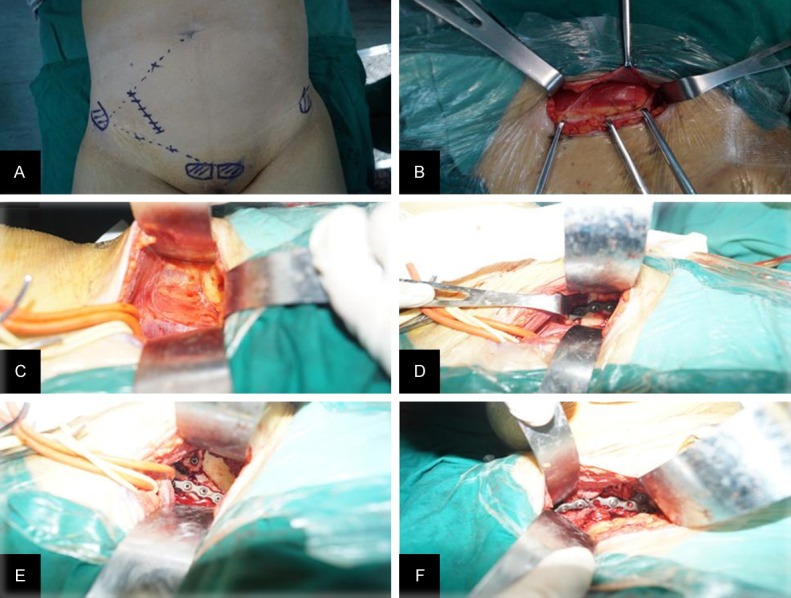
The operative process of pelvic fracture. The case in Figure 3 is the same patient as showed in Figures 1 and 2. A. Incision mark; B. Expose aponeurosis of obliquus externus abdominis and rectus abdominis anterior sheath; C. Expose the iliac crest; D. Place the plate in iliac crest; E. Exposed greater sciatic notch and iliopubic eminence, and placed the plate; F. Exposed superior ramus of pubis and placed the plate.
Results
The establishment of 3D physical models of pelvic fracture
Based on patient CT scan data and 3D printing technology, 1:1 3D physical models were printed. It showed strong stereoscopic sense. The morphological appearance of pelvic fracture can be observed from multi-angle and multi-direction.
The clinical results of surgery
Surgery went smoothly with a total of 80 pieces of plate and 501 pieces of screw implanted respectively. Postoperative imaging is consistent with intraoperative surgical simulation (Figure 4). The direction and length of the plates or screws implanted were highly consistent with the preoperative planning. None of the screws went into the hip joint cavity. The incision length was 5.5 cm~8 cm (average 6.5 cm). The operation time is 60~150 minutes (mean 110 minutes). Blood loss was 150 ml~900 ml (average 320 ml). One case happened with abdominal subcutaneous fat liquefaction, and the wound was recovered after 12 days. 38 patients were followed up from 6 to 18 months, all clinical fractures were healed, the healed time was 6~12 weeks (average 8 weeks). Matta [9] standard was used for fracture reduction, excellent in 33 cases, good in 4 cases, fair 1 case, good and excellent rate is 97.37%. Majeed [10] functional assessment score was used after 6 months, and excellent in 31 cases, good in 5 cases, fair in 2 cases, good and excellent rate was 94.74%.
Figure 4.
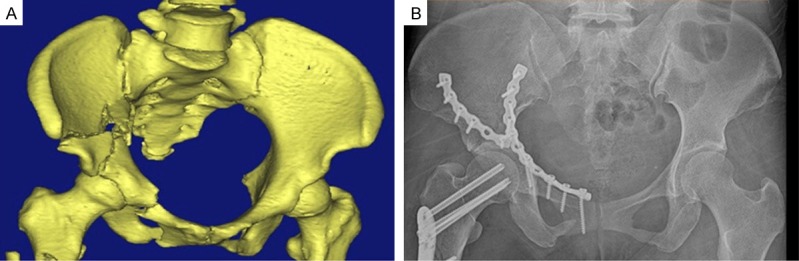
Imageological comparison between preoperation and postoperation. Preoperative three-dimensional CT scan (A) showed fracture displacement and postoperative X-ray examination (B) showed good reduction of the fracture for the case in Figure 1.
Discussion
Among patients with unstable pelvic fractures treated from conventional surgical approach, postoperative rates of complications tend to rise. Reports have showed the incidence of injuries to the lateral femoral cutaneous nerve, inability to close and postoperative hernia were 18%, 26% and 2%, respectively [12,13]. For these reasons, minimal invasive para-rectus abdominis approach has been suggested for stable pelvic fractures [14]. In our study, we have observed fewer postoperative complications such as reduced blood loss, lower infection rate, and less pain. This can be explained in two aspects. One was resulted from a shorter incision length when compared with other approaches. The other was that muscles or nerves were not injured due to avoidance of inguinal canal dissection during operation. However, the visualization of the fractures and subsequent fixation through 3-4 cm skin incision was rather restricted.
Three-dimensional printing technology is being rapidly developed in the medical field [15-21]. It allows surgeons to combine imagination with practicality 3D. With the aid of 3D printed models, preoperative situation of complex fractures is easier to understand. 3D printed model can also be used in preoperative realistic simulation and in turn facilitates more accurate surgical procedures. Therefore, the disadvantage of minimal invasive approach was offset by the information from 3D printed model. In our study, we have found both virtual surgical planning and post-operative results were consistent with the one from real surgery. Intraoperative fluoroscopy, postoperative X-ray examination and three-dimensional CT scan also showed good reduction of the fracture. Another advantage of this approach is the short average incision length of 6.5 cm, short operation time of 110 minutes, and less the average blood loss of 320 ml. Long-term follow-up showed good functional recovery for all the patients. These results suggested 3D printing assisted internal fixation from minimal invasive para-rectus abdominis approach has the advantages of minimal trauma, less bleeding, rapid healing and satisfactory reduction.
The limitation of this study is that the sample number is too small; we were unable to conduct randomized controlled trial to enhance the reliability of conclusions. Therefore we need to increase the sample number.
In conclusion, 3D printing assisted internal fixation of unstable pelvic fracture from minimal invasive para-rectus abdominis approach have better feasibility and effectivity. 3D printing technology contributes to developing individualized, optimal surgical options for pelvic fractures and make up vision deficiency of the small incision, which will prompt the operation of pelvic fracture more accurate and safe.
Acknowledgements
This work was supported by grants from 863 Science and technology projects of China (2012AA02A603SQ, 2010AA0221962001); Science and technology projects of tianhe district in Guangdong Province (201404KW025); Science Foundation of Hunan Province (2013FJ4094); High-level medical talents of ‘225’ project and Educational Project of Hunan province (XJK013CGD081) China.
Disclosure of conflict of interest
None.
References
- 1.Marmor M, Elson J, Mikhail C, Morshed S, Matityahu A. Short-term pelvic fracture outcomes in adolescents differ from children and adults in the National Trauma Data Bank. J Child Orthop. 2015;9:65–75. doi: 10.1007/s11832-015-0634-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fitzgerald CA, Morse BC, Dente CJ. Pelvic ring fractures: has mortality improved following the implementation of damage control resuscitation? Am J Surg. 2014;208:1083–90. doi: 10.1016/j.amjsurg.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 3.Marrinan S, Pearce MS, Jiang XY, Waters S, Shanshal Y. Admission for osteoporotic pelvic fractures and predictors of length of hospital stay, mortality and loss of independence. Age Ageing. 2015;44:258–61. doi: 10.1093/ageing/afu123. [DOI] [PubMed] [Google Scholar]
- 4.Dong J, Hao W, Wang B, Wang L, Li L, Mu W, Yang Y, Xin M, Wang F, Zhou D. Management and outcome of pelvic fractures in elderly patients: a retrospective study of 40 cases. Chin Med J (Engl) 2014;127:2802–7. [PubMed] [Google Scholar]
- 5.Perkins ZB, Maytham GD, Koers L, Bates P, Brohi K, Tai NR. Impact on outcome of a targeted performance improvement programme in haemodynamically unstable patients with a pelvic fracture. Bone Joint J. 2014;96:1090–7. doi: 10.1302/0301-620X.96B8.33383. [DOI] [PubMed] [Google Scholar]
- 6.Kabak S, Halici M, Tuncel M, Avsarogullari L, Baktir A, Basturk M. Functional outcome of open re-duction and internal fixation for completely unstable pelvic ring fractures (type C): a report of 40 cases. J Orthop Trauma. 2003;17:555–562. doi: 10.1097/00005131-200309000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Briffa N, Pearce R, Hill A M, Bircher M. Outcomes of acetabular fracture fixation with ten years’ follow-up. J Bone Joint Surg Br. 2011;93:229–36. doi: 10.1302/0301-620X.93B2.24056. [DOI] [PubMed] [Google Scholar]
- 8.Tile M. Pelvic ring fractures: should they be fixed. J Bone Joint Surg (Br) 1988;70:1–12. doi: 10.1302/0301-620X.70B1.3276697. [DOI] [PubMed] [Google Scholar]
- 9.Matta JM, Dickson KF, Markovich CD. Surgical treatment of pelvic nonunions and malunions. Clin Orthop Relat Res. 1996;329:199–206. doi: 10.1097/00003086-199608000-00024. [DOI] [PubMed] [Google Scholar]
- 10.Majeed SA. Grading the outcome of pelvic fracture. J Bone Joint Surg Br. 1989;71:304–306. doi: 10.1302/0301-620X.71B2.2925751. [DOI] [PubMed] [Google Scholar]
- 11.Helfet DL, Schmeling GJ. Management of complex acetabular fractures through single nonextensile exposures. Clin Orthop. 1994;305:58–68. [PubMed] [Google Scholar]
- 12.Sagi HC, Afsari A, Dziadosz D. The anterior intrapelvic (modified rives-stoppa) approach for fixation of acetabular fractures. J Orthop Trauma. 2010;24:263–270. doi: 10.1097/BOT.0b013e3181dd0b84. [DOI] [PubMed] [Google Scholar]
- 13.Cole JD, Bolhofner BR. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach: description of operative technique and preliminary treatment results. Clin Orthop. 1994;305:112–123. [PubMed] [Google Scholar]
- 14.Keel MJ, Ecker TM, Cullmann JL, Bergmann M, Bonel HM, Büchler L, Siebenrock KA, Bastian JD. The Pararectus approach for anterior intrapelvic management of acetabular fractures. J Bone Joint Surg Br. 2012;94:405–411. doi: 10.1302/0301-620X.94B3.27801. [DOI] [PubMed] [Google Scholar]
- 15.Chia HN, Wu BM. Recent advances in 3D printing of biomaterials. J Biol Eng. 2015;9:4. doi: 10.1186/s13036-015-0001-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rose AS, Webster CE, Harrysson OL, Formeister EJ, Rawal RB, Iseli CE. Pre-operative simulation of pediatric mastoid surgery with 3D-printed temporal bone models. Int J Pediatr Otorhinolaryngol. 2015;79:740–4. doi: 10.1016/j.ijporl.2015.03.004. [DOI] [PubMed] [Google Scholar]
- 17.Shim JH, Yoon MC, Jeong CM, Jang J, Jeong SI, Cho DW, Huh JB. Efficacy of rhBMP-2 loaded PCL/PLGA/β-TCP guided bone regeneration membrane fabricated by 3D printing technology for reconstruction of calvaria defects in rabbit. Biomed Mater. 2014;9:065006. doi: 10.1088/1748-6041/9/6/065006. [DOI] [PubMed] [Google Scholar]
- 18.Larkin M. 3-D printing makes its way to veterinary medicine. J Am Vet Med Assoc. 2014;245:24–5. [PubMed] [Google Scholar]
- 19.Jeong HS, Park KJ, Kil KM, Chong S, Eun HJ, Lee TS, Lee JP. Minimally invasive plate osteosynthesis using 3D printing for shaft fractures of clavicles: technical note. Arch Orthop Trauma Surg. 2014;134:1551–5. doi: 10.1007/s00402-014-2075-8. [DOI] [PubMed] [Google Scholar]
- 20.Zhou Z, Buchanan F, Mitchell C, Dunne N. Printability of calcium phosphate: calcium sulfate powders for the application of tissue engineered bone scaffolds using the 3D printing technique. Mater Sci Eng C Mater Biol Appl. 2014;38:1–10. doi: 10.1016/j.msec.2014.01.027. [DOI] [PubMed] [Google Scholar]
- 21.Inzana JA, Olvera D, Fuller SM, Kelly JP, Graeve OA, Schwarz EM, Kates SL, Awad HA. 3D printing of composite calcium phosphate and collagen scaffolds for bone regeneration. Biomaterials. 2014;35:4026–34. doi: 10.1016/j.biomaterials.2014.01.064. [DOI] [PMC free article] [PubMed] [Google Scholar]


