Abstract
Coronary heart disease (CHD) remains the leading causes of death and disability for men and women in most developed countries. It may soon become the leading cause of death in developing countries. Several studies have examined the role of fibrinogen levels in the prediction of atherosclerosis and CHD events. The aim of this study was to explore the effects of plasma fibrinogen levels in Chinese patients with CHD and to examine the relationship of fibrinogen. We performed this meta-analysis of prospective studies of plasma fibrinogen level in relation to CHD risk in electronic database of Medline, EMBase, the Cochrane Library and CNKI (China National Knowledge Infrastructure). Plasma fibrinogen levels were calculated by mean difference with 95% confidence intervals (CI) in patients with CHD and related controls without CHD. The selected 23 studies included 2984 CHD cases and 2279 controls. Our results found that plasma fibrinogen levels of patients were significantly higher than control group (P<0.0001). The predicted odds ratio (OR) for a 1 g/L higher plasma fibrinogen level was 0.94 (95% CI=0.78-1.10). Furthermore, fibrinogen levels were slightly related to age-related CHD patients. The plasma fibrinogen lever was correlated with CHD in the Chinese population, and may be a risk factor and predictor of CHD. Further studies assessing any causal relevance of fibrinogen levels to disease are required.
Keywords: Coronary heart disease, plasma fibrinogen lever, meta-analysis
Introduction
Cardiovascular disease is the leading cause of global mortality, with coronary heart disease (CHD) its major manifestation in today’s clinical practice. CHD is a multifactorial disease results from a complex interplay between environmental and genetic factors [1]. Every year, more than 16.3 million adults have CHD, and an estimated 935 000 heart attacks occur in the United States alone [2]. It remains not only the leading cause of death in most developed and developing countries, but also complicates the identification of the causal pathways, and delaying the development of new treatments [3,4]. In the last few decades novel risk factors for CHD have been identified in previously healthy subjects, such as inflammatory markers (C-reactive protein), and prothrombotic markers (fibrinogen) [5,6]. Although prospective cohort studies have examined fibrinogen in large populations with long periods of follow-up, whether these markers are a cause or consequence of CHD remains debatable.
Fibrinogen, the precursor of fibrin, was the first described blood coagulation factor [7,8]. The mature fibrinogen protein is made up of two chains, each of which has three different polypeptides, alpha, beta, and gamma, encoding by three genes located in a cluster of 51 kb on chromosome 4 at q23-q32 [9]. Fibrinogen is an acute-phase inflammatory protein involved in blood clotting and is also a potentially suitable target for CHD [10]. Many studies had demonstrated that the plasma fibrinogen concentration was associated with CHD [11]. These associations indicated that fibrinogen might be a possible causal factor, a therapeutic target, and a risk predictor in not only healthy persons but also those with cardiovascular diseases. Observational studies show that an increase of 1 g/L of plasma fibrinogen is associated with more than a two-fold increase in CHD and fibrinogen lever may predict the development, the course, and negative prognosis of coronary heart disease (CHD) [12,13]. However, the relevance of circulating levels of plasma fibrinogen to CHD risk remains uncertain.
Moreover, Okwuosa et al. have demonstrated that fibrinogen tracked longitudinally with changes in traditional risk factors over 13 years through middle age among young black and white men and women with few baseline cardiovascular risk factors [14]. Considering the diversity between age, sex and ethnicity, and the necessity to improve prevention strategies in CHD patients, we conducted this meta-analysis and aimed to evaluate the prognostic implications of fibrinogen in a unique and relatively large cohort of Chinese patients with acute coronary syndrome.
Materials and methods
Search strategy for identification of studies
Four major electronic databases, Medline, EMBase, the Cochrane Library and China National Knowledge Infrastructure (CNKI) were searched for related reports between 2005 and 2013 using the following medical subject heading terms and keywords: coronary heart disease, CHD, plasma fibrinogen and risk factors. All eligible studies were retrieved. And references were retrieved for other relevant publications.
Criteria for article screening
Studies were defined as eligible if: 1) they were prospective cohort studies evaluating fibrinogen level to CHD risk; 2) adult patients with longer than 1 year of follow-up; 3) all CHD patients accorded with the diagnosis standard of WHO in 1999, and coronary angiography results show that at least one coronary artery lumen diameter was stenosed more than 50% [15]; 4) the two groups of subjects have no significant difference in such aspects as age and gender. No language restrictions were applied.
The excluded criteria were: 1) patients with diabetes, podagra, and immune system diseases; 2) patients with blood disease, malignant tumor, and heart kidney function; 3) patients have anticoagulant therapy prior to admission to hospital.
Data extraction
All of the data were independently abstracted in duplicate by two authors. The following information was concerned: study characteristics, participant information, analyses, CHD outcome, and adjustment. Discrepancies were resolved by discussing with a third author to reach a final consensus.
Statistical analysis
The strength of association between fibrinogen level and CHD risk was assessed by the mean difference with 95% confidence intervals (95% CI). A P-value of the Z test less than 0.05 was considered significant, which determined the significance of the pooled mean level. The between-study heterogeneity of all the included articles was evaluated by the Cochran’s Q test and the I2 statistics. The fixed-effect model was used when the P-value of the Q test more than 0.1 and the I2 less than 50%, considering no statistically significant heterogeneity among studies. Otherwise, the random-effect model was employed. The funnel plot was performed to examine the publication bias. Analyses were performed in the Review manager 5.2 (The Cochrane Collaboration). All tests were two-sided.
Results
Characteristics of included studies
The electronic database search identified 5321 references. Following the inclusion criteria for relevance, finally a total of 23 studies containing 5263 participants were included in this meta-analysis. Figure 1 showed the study flow.
Figure 1.
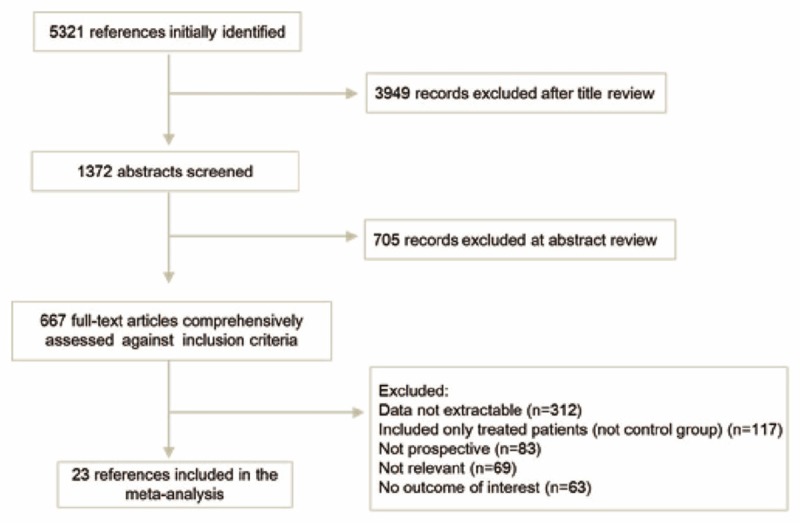
Summary of article selection process.
Among the 23 papers, one was written in English [16], twenty-two were published in Chinese [17-38]. All of them, including 2984 patients and 2279 healthy controls, was assessed the relationship between fibrinogen level and CHD. The major characteristics of the eligible publications are reported in Table 1.
Table 1.
Main characteristics of included studies in this meta-analysis
| First author-published year | Cases | Controls | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Age | Total | FB level | Age | Total | FB level | |
| Li Y-2005 | 66.1±7.4 | 58 | 3.82±0.56 | 62.5±8.3 | 22 | 2.92±0.32 |
| Xia HJ-2005 | 68.3±19.2 | 109 | 3.99±1.17 | 65.7±12.3 | 162 | 3.32±1.05 |
| Zhou BR-2005 | 63.8±7.5 | 100 | 4.82±0.46 | - | 36 | 3.46±0.57 |
| Zhao Y-2005 | 70.65±11.35 | 75 | 3.69±0.81 | 67.62±10.60 | 65 | 3.33±0.86 |
| Hao JH-2006 | 71.02±15.56 | 78 | 5.74±2.54 | 68.35±14.83 | 60 | 3.82±1.70 |
| Ma ZX-2006 | 58.4±7.8 | 46 | 3.72±1.08 | 51.3±7.5 | 82 | 3.31±0.74 |
| Zhang ZL-2006 | 68.6±4.6 | 91 | 3.48±0.96 | 67.4±4.9 | 72 | 2.65±0.38 |
| Chen SA-2007 | 66.4±13.88 | 80 | 4.25±0.32 | 50.53±9.01 | 78 | 3.21±0.65 |
| Sun AJ-2008 | 64.2±10.2 | 836 | 3.43±2.03 | 59.7±11.1 | 418 | 3.11±0.68 |
| Tian CL-2008 | 62.5±11.2 | 120 | 3.64±0.76 | 58.7±10.3 | 100 | 2.89±0.62 |
| Bai CW-2009a | 43± 4 | 60 | 3.27±0.54 | 41±6 | 74 | 2.67±0.30 |
| Bai CW-2009b | 65±6 | 105 | 3.15±0.49 | 41±6 | 74 | 2.67±0.30 |
| Li GT-2009 | 67.1±8.4 | 106 | 4.04±0.49 | 64.5±7.3 | 50 | 2.91±0.36 |
| Li JQ-2010 | 69.8 | 83 | 4.91±0.51 | 63 | 54 | 3.21±0.54 |
| Liu CF-2010 | 41-75 | 112 | 4.01±0.51 | 23-67 | 150 | 3.17±0.73 |
| Lv LS-2010 | 44.1 | 103 | 4.03±0.43 | 43.6 | 108 | 3.19±0.25 |
| Hu YW-2011 | 62.16±8.72 | 100 | 3.50±1.06 | 56.00±10.25 | 100 | 2.83±0.46 |
| Sun RL-2011 | 46 | 76 | 3.51±0.52 | 44 | 82 | 2.21±0.32 |
| Wang YH-2011 | 62.5±11.2 | 120 | 3.64±0.76 | 58.7±10.3 | 100 | 2.89±0.62 |
| Zhang YQ-2011 | 60±12 | 128 | 4.94±1.87 | - | 32 | 3.06±0.58 |
| Rong YZ-2012 | 63.25±8.06 | 50 | 4.76±0.25 | 59.31±4.79 | 50 | 3.22±0.43 |
| Du MY-2013 | 68.5±5.6 | 112 | 4.35±0.55 | 68.0±5.2 | 100 | 3.58±0.48 |
| Liang ZH-2013 | 63.2±1.4 | 80 | 3.4±0.6 | 62.7±1.9 | 80 | 2.4±0.4 |
| Zhang Y-2013 | 42.5 | 156 | 4.12± 0.58 | 43.1 | 130 | 3.20±0.27 |
Association of fibrinogen level and CHD risk
The case-control comparison yielded a risk ratio for CHD of 0.94 (95% CI=0.78-1.10) per 1 g/L higher usual plasma fibrinogen concentration, which is equivalent to a risk ratio of middle-aged less than 50-year-old (OR=0.90, 95% CI=0.71-1.10) and old-aged (OR=0.96, 95% CI=0.75-1.16). There is a significantly association between plasma fibrinogen level and CHD risk (P<0.0001). Table 2 shows the predicted OR for about 1 g/L increase in plasma fibrinogen, calculated assuming a linear-logistic relationship between plasma fibrinogen level and risk of CHD. Figure 2 showed the relationship among middle-aged patients (less than 50-year-old). However, there is a significantly heterologous among studies.
Table 2.
Meta-analysis of predicted association for plasma fibrinogen level and CHD risk
| OR (95% CI) | P value | PHeterogeneity | Model | |
|---|---|---|---|---|
| All studies | 0.94 (0.78, 1.10) | P<0.0001 | P<0.0001 | Random-effect model |
| Studies with middle patients | 0.90 (0.71, 1.10) | P<0.0001 | P<0.0001 | Random-effect model |
| Studies with old patients | 0.96 (0.75, 1.16) | P<0.0001 | P<0.0001 | Random-effect model |
Figure 2.
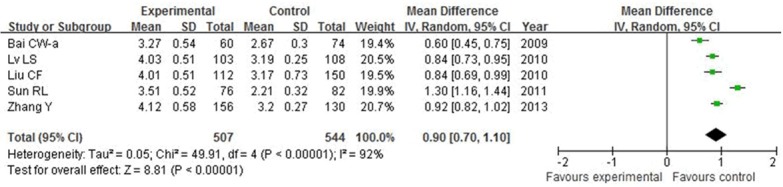
Forest plot on the association between plasma fibrinogen level and CHD risk among middle-aged patients.
Sensitivity analyses and publication bias
The individual study included was omitted one time to estimate the influence of the single article to the pooled ORs. The corresponding pooled ORs were not materially changed, which confirmed the stability of our overall result.
The funnel plot was conducted to assess the publication bias of the included studies. Its shape did not reveal any evidence of funnel plot asymmetry. As shown in Figure 3. The statistical results still did not show publication bias.
Figure 3.
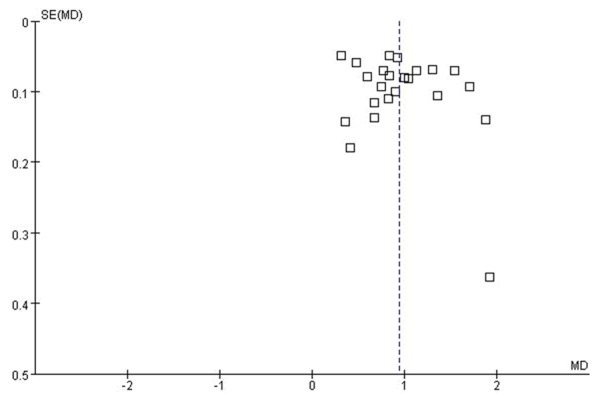
Publication bias for the analysis of all the studies.
Discussion
Fibrinogen plays a key role in the final step of the coagulation cascade such as the formation of fibrin [39]. It is also a major determinant of plasma viscosity and erythrocyte aggregation [40,41]. Fibrinogen, as well as its decomposition products, mediates the transportation of adhesion molecules in the surface of endothelium and their further migration to the intima. They can also trigger proliferation and migration of smooth-muscle cells [42]. In regard to the inflammatory aspect of fibrinogen, inflammatory process is mainly mediated by the interaction of fibrinogen-leukocytes mediated by integrins [43].
Many studies have examined the role of fibrinogen levels alone or combined with other risk factors in the prediction of atherosclerosis and CHD events. Xu et al. shown that high fibrinogen may be a possible link between job stress and cardiovascular disease [44]. Aliberti et al. found an association between fibrinogen plasma levels and platelet counts in an outpatient population and in patients with CHD [45]. In the past years, plasma fibrinogen is under debate whether it is a primary risk factor/mediator for CHD, or whether it is a marker for disease [46]. Many cohort studies showed that fibrinogen may partly mediate the effects of other risk factors on carotid atherosclerosis [47]. Molecular biology found that fibrinogen is a marker, rather than a mediator, of vascular disease [48].
The present meta-analysis involves individual participant data from 23 prospective studies of CHD among 2984 individuals with known CHD at baseline and 2279 health controls. Our results found plasma fibrinogen levels of patients were 0.94-folder higher than control group, and showed a significantly association between plasma fibrinogen level and CHD risk (P<0.0001). The predicted causal odds ratio for a 1 g/L higher plasma fibrinogen level was 0.94 (95% CI=0.78-1.10), indicating fibrinogen level is associated with the incidence rates of CHD. These data showed that throughout the range of fibrinogen levels recorded in Asian populations, the proportional differences in risk of each of these end points associated with a given absolute difference in usual fibrinogen are generally similar at all fibrinogen levels.
Studies have shown that reducing the fibrinogen level might be a potential method in reducing the CHD risk [49]. Lifestyle interventions can considerably reduce the fibrinogen level and influence levels of several established risk factors such as moderate alcohol consumption, and regular exercise, which may help in disease prediction or prevention [50]. A previous meta-analysis which included 18 such studies and about 4000 CHD cases, indicated a relative risk of 1.8 (95% CI=1.6-2.0) per 1 g/L increase in plasma fibrinogen level [51].
Fibrinogen levels were related with several established risk factors, for example, blood pressure and serum cholesterol levels. Panagiotakos et al. showed that in individuals with heterozygous familial hypercholesterolemia, fibrinogen levels are among the strong predictors of CHD [52]. These confounding factors probably have been measured with some error so substantial residual confounding may remain. Furthermore, an interesting study by Several limitations were presented in this study. Firstly, we only evaluated associations between plasma level and CHD risk among Chinese population, other populations should be considered. Secondly, there is large heterologous among studies in our analysis due to a small group of patients. Thirdly, fibrinogen levels may correlate with several other factors such as smoking, sex, serum lipid levels which should be considered. Fourthly, we did not investigate whether genetic and environmental factors modify each other in these associations.
Overall, our study found that plasma fibrinogen levels were higher in patients with CHD compared to normal subjects. These results proved that there is a significant relationship between fibrinogen levels and the progress of CHD. Further studies involving larger numbers of patients and relating with other risk factors may elucidate the clearly association between fibrinogen levels and the CHD severity.
Disclosure of conflict of interest
None.
References
- 1.Allender S, Peto V, Scarborough P, Boxer A, Rayner M. Coronary heart disease statistics. 2012 [Google Scholar]
- 2.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Soliman EZ, Sorlie PD, Sotoodehnia N, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. Heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Barker-Collo S, Bartels DH, Bell ML, Benjamin EJ, Bennett D, Bhalla K, Bikbov B, Bin Abdulhak A, Birbeck G, Blyth F, Bolliger I, Boufous S, Bucello C, Burch M, Burney P, Carapetis J, Chen H, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahodwala N, De Leo D, Degenhardt L, Delossantos A, Denenberg J, Des Jarlais DC, Dharmaratne SD, Dorsey ER, Driscoll T, Duber H, Ebel B, Erwin PJ, Espindola P, Ezzati M, Feigin V, Flaxman AD, Forouzanfar MH, Fowkes FG, Franklin R, Fransen M, Freeman MK, Gabriel SE, Gakidou E, Gaspari F, Gillum RF, Gonzalez-Medina D, Halasa YA, Haring D, Harrison JE, Havmoeller R, Hay RJ, Hoen B, Hotez PJ, Hoy D, Jacobsen KH, James SL, Jasrasaria R, Jayaraman S, Johns N, Karthikeyan G, Kassebaum N, Keren A, Khoo JP, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Lipnick M, Lipshultz SE, Ohno SL, Mabweijano J, MacIntyre MF, Mallinger L, March L, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGrath J, Mensah GA, Merriman TR, Michaud C, Miller M, Miller TR, Mock C, Mocumbi AO, Mokdad AA, Moran A, Mulholland K, Nair MN, Naldi L, Narayan KM, Nasseri K, Norman P, O’Donnell M, Omer SB, Ortblad K, Osborne R, Ozgediz D, Pahari B, Pandian JD, Rivero AP, Padilla RP, Perez-Ruiz F, Perico N, Phillips D, Pierce K, Pope CA 3rd, Porrini E, Pourmalek F, Raju M, Ranganathan D, Rehm JT, Rein DB, Remuzzi G, Rivara FP, Roberts T, De Leon FR, Rosenfeld LC, Rushton L, Sacco RL, Salomon JA, Sampson U, Sanman E, Schwebel DC, Segui-Gomez M, Shepard DS, Singh D, Singleton J, Sliwa K, Smith E, Steer A, Taylor JA, Thomas B, Tleyjeh IM, Towbin JA, Truelsen T, Undurraga EA, Venketasubramanian N, Vijayakumar L, Vos T, Wagner GR, Wang M, Wang W, Watt K, Weinstock MA, Weintraub R, Wilkinson JD, Woolf AD, Wulf S, Yeh PH, Yip P, Zabetian A, Zheng ZJ, Lopez AD, Murray CJ, AlMazroa MA, Memish ZA. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McPhee SJ, Papadakis MA, Rabow MW Current medical diagnosis & treatment 2010. McGraw-Hill Medical; 2010. [Google Scholar]
- 5.Kaptoge S, Di Angelantonio E, Lowe G, Pepys MB, Thompson SG, Collins R, Danesh J. C-reactive protein concentration and risk of coronary heart disease, stroke, and mortality: an individual participant meta-analysis. Lancet. 2010;375:132–140. doi: 10.1016/S0140-6736(09)61717-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hale L, Parente V, Dowd JB, Sands M, Berger JS, Song Y, Martin LW, Allison MA. Fibrinogen may mediate the association between long sleep duration and coronary heart disease. J Sleep Res. 2012;22:305–14. doi: 10.1111/jsr.12020. [DOI] [PubMed] [Google Scholar]
- 7.Lowe GD. Fibrinogen and cardiovascular disease: historical introduction. Eur Heart J. 1995;16(Suppl A):2–5. doi: 10.1093/eurheartj/16.suppl_a.2. [DOI] [PubMed] [Google Scholar]
- 8.Code C. Fibrinogen (mass) Current Medicinal Chemistry. 2010:17. [Google Scholar]
- 9.Kant JA, Fornace AJ Jr, Saxe D, Simon MI, McBride OW, Crabtree GR. Evolution and organization of the fibrinogen locus on chromosome 4: gene duplication accompanied by transposition and inversion. Proc Natl Acad Sci U S A. 1985;82:2344–2348. doi: 10.1073/pnas.82.8.2344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ait-Goughoulte M, Banerjee A, Meyer K, Mazumdar B, Saito K, Ray RB, Ray R. Hepatitis C virus core protein interacts with fibrinogen-beta and attenuates cytokine stimulated acute-phase response. Hepatology. 2010;51:1505–1513. doi: 10.1002/hep.23502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hale L, Parente V, Dowd JB, Sands M, Berger JS, Song Y, Martin LW, Allison MA. Fibrinogen may mediate the association between long sleep duration and coronary heart disease. J Sleep Res. 2013;22:305–314. doi: 10.1111/jsr.12020. [DOI] [PubMed] [Google Scholar]
- 12.Danesh J, Lewington S, Thompson SG, Lowe GD, Collins R, Kostis JB, Wilson AC, Folsom AR, Wu K, Benderly M, Goldbourt U, Willeit J, Kiechl S, Yarnell JW, Sweetnam PM, Elwood PC, Cushman M, Psaty BM, Tracy RP, Tybjaerg-Hansen A, Haverkate F, de Maat MP, Fowkes FG, Lee AJ, Smith FB, Salomaa V, Harald K, Rasi R, Vahtera E, Jousilahti P, Pekkanen J, D’Agostino R, Kannel WB, Wilson PW, Tofler G, Arocha-Pinango CL, Rodriguez-Larralde A, Nagy E, Mijares M, Espinosa R, Rodriquez-Roa E, Ryder E, Diez-Ewald MP, Campos G, Fernandez V, Torres E, Marchioli R, Valagussa F, Rosengren A, Wilhelmsen L, Lappas G, Eriksson H, Cremer P, Nagel D, Curb JD, Rodriguez B, Yano K, Salonen JT, Nyyssonen K, Tuomainen TP, Hedblad B, Lind P, Loewel H, Koenig W, Meade TW, Cooper JA, De Stavola B, Knottenbelt C, Miller GJ, Bauer KA, Rosenberg RD, Sato S, Kitamura A, Naito Y, Palosuo T, Ducimetiere P, Amouyel P, Arveiler D, Evans AE, Ferrieres J, Juhan-Vague I, Bingham A, Schulte H, Assmann G, Cantin B, Lamarche B, Despres JP, Dagenais GR, Tunstall-Pedoe H, Woodward M, Ben-Shlomo Y, Davey Smith G, Palmieri V, Yeh JL, Rudnicka A, Ridker P, Rodeghiero F, Tosetto A, Shepherd J, Ford I, Robertson M, Brunner E, Shipley M, Feskens EJ, Kromhout D, Dickinson A, Ireland B, Juzwishin K, Kaptoge S, Memon A, Sarwar N, Walker M, Wheeler J, White I, Wood A. Plasma fibrinogen level and the risk of major cardiovascular diseases and nonvascular mortality: an individual participant meta-analysis. JAMA. 2005;294:1799–1809. doi: 10.1001/jama.294.14.1799. [DOI] [PubMed] [Google Scholar]
- 13.Smith GD, Harbord R, Milton J, Ebrahim S, Sterne JA. Does elevated plasma fibrinogen increase the risk of coronary heart disease? Evidence from a meta-analysis of genetic association studies. Arterioscler Thromb Vasc Biol. 2005;25:2228–2233. doi: 10.1161/01.ATV.0000183937.65887.9c. [DOI] [PubMed] [Google Scholar]
- 14.Okwuosa TM, Klein O, Chan C, Jenny NS, Schreiner P, Green D, Liu K. 13-year long-term associations between changes in traditional cardiovascular risk factors and changes in fibrinogen levels: The Coronary Artery Risk Development in Young Adults (CARDIA) study. Atherosclerosis. 2012;226:214–9. doi: 10.1016/j.atherosclerosis.2012.10.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lavis J, Sullivan T, Drache D, Sullivan T. Governing health. Health Reform: Public Success, Private Failure. 1999;8:321. [Google Scholar]
- 16.Sun AJ, Ma HL, Chen XY, Wang Y, Fang YM, Ma YL, Wang KQ, Zou YZ, Huang W, Ge JB. Association of fibrinogen and fibrinogen gene beta148 and beta854 polymorphisms with coronary heart disease. Cardiology. 2008;111:167–170. doi: 10.1159/000121599. [DOI] [PubMed] [Google Scholar]
- 17.Bai CW, Huang ZJ, Yi ZH. The Relativity of Plasma Fibrinogen and Coronary Heart Disease of Young and Middle Age in South of China. Journal of University of South China (Medical Edition) 2009;3:017. [Google Scholar]
- 18.Hu YW, Gao P, Zhang YC, Xu FJ, Feng N, Ma YJ, Liu M. Clinical Applications of D-dimmer, fibrinogen and antithrombin III on diagnosis and treatment of coronary heart disease. Laboratory Medicine and Clinic. 2011;24:019. [Google Scholar]
- 19.Wang YH, Zeng JH. Role and its clinical significance of fibrinogen in coronary heart disease. Modern Medicine & Health. 2011;12:012. [Google Scholar]
- 20.Yongzhong R. The Diagnosis Value of Fibrinogen Apolipoprotein A Lipoprotein for Coronary Heart Disease. Hebei Medicine. 2012;1:005. [Google Scholar]
- 21.Zhang Z, Zhou W, Zhu J, Zhou L. The relationship between high sensitive C-reactive protein and fibrinogen levels and coronary heart disease in elderly patients. Chinese Journal of Clinical Healthcare. 2006;5:004. [Google Scholar]
- 22.Ma ZX, Liu AL, Liu JH, Zhang HY, Chen X. The Role of Plasmatic Fibrinogen in the Pathogenesis of Coronary Heart Disease. Clinical Journal of Medical Officer. 2006;4:052. [Google Scholar]
- 23.Li GT, Li Y, Liang YB. Clinical Significance of Serum Lipids Blood Uric Acid and Fibrinogen in Coronary Heart Disease Patients. Hebei Medicine. 2009;3:017. [Google Scholar]
- 24.Jinhong H. Analysis of Fibrinogen, D-dimer, Lipoprotein (a) and White Blood Cell in Coronary Heart Disease. Journal of Qiqihar Medical College. 2006;12:001. [Google Scholar]
- 25.Zhang Y. Analysis of serum uric acid, bilirubin and plasma fibrinogen level on coronary heart disease. China Health Industry. 2013:135–136. [Google Scholar]
- 26.Liang Z. The clinical significance of detecting plasma fibrinogen and C-reactive protein in patients with coronary heart disease. Guide of China Medicine. 2013:535. [Google Scholar]
- 27.Du M. Roles of serum uric acid, plasma fibrinogen and antithrombin III combined determination in the diagnosis of coronary heart disease. Seek Medical and Ask The Medical. 2013:162–163. [Google Scholar]
- 28.Sun R, Cai J, Ge L. Analysis of serum uric acid, bilirubin and plasma fibrinogen on prevalence of coronary heart disease. Ningxia Medical Journal. 2011:1059–1060. [Google Scholar]
- 29.Zhang Y, Tang Y, Liu Y. Roles of plasma fibrinogen on prevalence of coronary heart disease. Shanxi Medical Journal. 2011:982–983. [Google Scholar]
- 30.Liu C. Association between serum uric acid, bilirubin and plasma fibrinogen and coronary heart disease. Chinese Journal of Laboratory Diagnosis. 2010:225–226. [Google Scholar]
- 31.Lv L. Association between serum uric acid, bilirubin and plasma fibrinogen and coronary heart disease. Guide of China Medicine. 2010:103–104. [Google Scholar]
- 32.Li J, Lei X. Significant of homocysteine, plasma fibrinogen and lipoprotein (a) in the diagnosis of coronary heart disease. Guangzhou Medical Journal. 2010:61–62. [Google Scholar]
- 33.Tian C. Relationship between plasma fibrinogen and coronary heart disease. Zhejiang Journal of Traumatic Surgery. 2008:175–176. [Google Scholar]
- 34.Xia H, Liu W, Jiang L, Chen G. Relationship of plasma fibrinogen, uric acid and coronary heart disease. Journal of Chinese Physician. 2005;7:419–420. [Google Scholar]
- 35.Zhao Y, Pan G, Sun X, Han L. Study on coronary heart disease with serum uric acid, bilirubin and plasma fibrinogen levels. Journal of Clinical Internal Medicine. 2005;22:200–201. [Google Scholar]
- 36.Zhou B, Xu Y, Wu J, Xu Y. Significance of detecting coronary heart disease with plasma fibrinogen, serum lipoprotein (a) and platelet. Chinese Journal of Cardiovascular Rehabilitation Medicine. 2005;14:514–516. [Google Scholar]
- 37.Li Y, Jia Q. Measurement and analysis of blood lipids, blood uric acid and plasma fibrinogen in patients with coronary heart disease. International Medicine & Health Guidance News. 2005;11:21–22. [Google Scholar]
- 38.Chen S, Mai A, Tang Y. Association of serum uric acid, bilirubin and plasma fibrinogen in coronary heart disease. Journal of Practical Medical Techniques. 2007;14:45–46. [Google Scholar]
- 39.Danesh J, Collins R, Peto R, Lowe GD. Haematocrit, viscosity, erythrocyte sedimentation rate: meta-analyses of prospective studies of coronary heart disease. Eur Heart J. 2000;21:515–520. doi: 10.1053/euhj.1999.1699. [DOI] [PubMed] [Google Scholar]
- 40.Weil JV, Byrne-Quinn E, Sodal IE, Kline JS, McCullough RE, Grover RF, Filley GF. Ventilatory control in normal man: effects of acute exercise, chronic physical conditioning and chronic hypoxia. Chest. 1972;61(Suppl):45S–46S. doi: 10.1378/chest.61.2_supplement.45s. [DOI] [PubMed] [Google Scholar]
- 41.Papageorgiou N, Tousoulis D, Miliou A, Hatzis G, Kozanitou M, Androulakis E, Charakida M, Antonopoulos A, Antoniades C, Briasoulis A. Combined effects of fibrinogen genetic variability on atherosclerosis in patients with or without stable angina pectoris: Focus on the coagulation cascade and endothelial function. Int J Cardiol. 2013;168:4602–4607. doi: 10.1016/j.ijcard.2013.07.162. [DOI] [PubMed] [Google Scholar]
- 42.Stroncek DF, Shankar RA, Skubitz KM. The subcellular distribution of myeloid-related protein 8 (MRP8) and MRP14 in human neutrophils. J Transl Med. 2005;3:36. doi: 10.1186/1479-5876-3-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stefanadi E, Tousoulis D, Papageorgiou N, Briasoulis A, Stefanadis C. Inflammatory biomarkers predicting events in atherosclerosis. Current Medicinal Chemistry. 2010;17:1690–1707. doi: 10.2174/092986710791111288. [DOI] [PubMed] [Google Scholar]
- 44.Xu W, Hang J, Guo L, Zhao Y, Li Z, Gao W. Plasma fibrinogen: A possible link between job stress and cardiovascular disease among Chinese workers. Am J Ind Med. 2012;55:167–75. doi: 10.1002/ajim.21017. [DOI] [PubMed] [Google Scholar]
- 45.Aliberti G, Proietta M, Pulignano I, Del Porto F, Tammeo A, Trappolini M. Association between fibrinogen plasma levels and platelet counts in an outpatient population and in patients with coronary heart disease. Blood Coagulation & Fibrinolysis. 2010;21:216–220. doi: 10.1097/MBC.0b013e32833449c9. [DOI] [PubMed] [Google Scholar]
- 46.Hamsten A, Iselius L, de Faire U, Blomback M. Genetic and cultural inheritance of plasma fibrinogen concentration. Lancet. 1987;2:988–991. doi: 10.1016/s0140-6736(87)92557-8. [DOI] [PubMed] [Google Scholar]
- 47.Grebe MT, Luu B, Sedding D, Heidt MC, Kemkes-Matthes B, Schaefer CA, Tillmanns HH, Guenduez D. Fibrinogen promotes early atherosclerotic changes of the carotid artery in young, healthy adults. J Atheroscler Thromb. 2010;17:1003. doi: 10.5551/jat.3715. [DOI] [PubMed] [Google Scholar]
- 48.Reinhart WH. Fibrinogen--marker or mediator of vascular disease? Vasc Med. 2003;8:211–216. doi: 10.1191/1358863x03vm494ra. [DOI] [PubMed] [Google Scholar]
- 49.Kamath S, Lip GY. Fibrinogen: biochemistry, epidemiology and determinants. QJM. 2003;96:711–729. doi: 10.1093/qjmed/hcg129. [DOI] [PubMed] [Google Scholar]
- 50.Ping Q. A study on the relationship between plasma fibrinogen lever and coronary heart disease in patients with the metabolism syndrome. Heart. 2011;97:A142–A142. [Google Scholar]
- 51.Danesh J, Collins R, Appleby P, Peto R. Association of fibrinogen, C-reactive protein, albumin, or leukocyte count with coronary heart disease: meta-analyses of prospective studies. JAMA. 1998;279:1477–1482. doi: 10.1001/jama.279.18.1477. [DOI] [PubMed] [Google Scholar]
- 52.Panagiotakos DB, Toutouzas PK. Importance of LDL/HDL cholesterol ratio as a predictor for coronary heart disease events in patients with heterozygous familial hypercholesterolaemia: a 15-year follow-up (1987-2002) Curr Med Res Opin. 2003;19:89–94. [PubMed] [Google Scholar]


