Abstract
Relatively few studies have addressed surgical strategy for complex proximal tibial fractures by now. The purpose of this study was to assess the results of a single lateral locking plate using minimally invasive plate osteosynthesis (MIPO) for proximal tibia fractures (AO/OTA type 41-C) with diaphyseal involvement. From Jun 2009 to Jun 2014, 20 patients (fifteen women and five men, mean age 35.8 years) were managed for proximal tibial fractures which extend into the diaphyseal region of the bone, including three 41-C1, eleven 41-C2, and six 41-C3. Twelve patients were open fractures. A single lateral locking plate characterized by percutaneous technology was used with or without additional lag screws. Mobilization was started immediately after the procedure, and non-weight-bearing was maintained for at least 6 weeks, then progressively weight bearing depends on both clinical and x-ray findings. Primary union was achieved by 16 of the 20 study subjects. Early bone grafting was performed in 4 cases with a massive initial bone defect and staged bone grafting was used in one to treat nonunion. The mean articular step off was 1.0 mm (range, 0-3 mm). No patient had misalignment greater than 10°. Acceptable range of knee motion of ≥120° was achieved in sixteen, and the mean knee Hass score was 87.4 at final follow-up visits. The complications included superficial infection in one patient. In conclusion, the surgical strategy can provide favorable results in the treatment of proximal tibial fractures (AO/OTA type 41-C) with diaphyseal involvement.
Keywords: Surgical strategy, proximal, tibial fractures, minimally invasive surgical procedure, single lateral, locking plate
Introduction
Proximal tibia fractures (AO/OTA type 41-C) with diaphyseal involvement are serious injuries and present treatment challenges [1]. The management of high-energy proximal tibial fractures requires the surgeon to take very good care of the soft-tissue envelope as the anteromedial surface of the tibia is covered only with skin and subcutaneous tissues [2]. Poor bone quality and comminuted fracture patterns create difficulty in achieving stable fixation. Any surgical strategy for fracture fixation should demand the minor infection rates and high union rates without bone grafting and recover the good functional outcome.
Minimally invasive locking plate osteosynthesis (MILPO) is a burgeoning technique providing an alternative to intramedullary devices, external fixation and conventional plate osteosynthesis in complex proximal tibial fractures management [3,4]. The use of MILPO technique, which is rather flexible and allows reducing the surgical trauma. Still articular fractures seem to require precise and stable fixation [5]. The biological complication results from extensive surgical stripping of bone blood supply in an attempt to achieve perfect reduction and absolute stability. Depending on more tolerant, forgiving technologies of internal fixation, single lateral locking plate using MIPO technique has been advocated as a means of decreasing the risk of skin damage, ligament damage, and surgical site infection [6-8].
In our institutions, we have been using a single lateral locking plate system characterized by percutaneous technology. This is a better understanding of fracture healing in respect to the balance between mechano-biological tradeoffs. The purpose of this study was to evaluate the perioperative results and functional outcome following operative treatment of complex proximal tibial fractures using the surgical strategy (a single lateral locking plate/MIPO technique).
Patients and methods
This retrospective study included 15 men and 5 women who were aged from 25 to 58 years and were diagnosed as having a proximal tibial fracture with diaphyseal involvement. The fractures were stabilized with the single lateral insertion of two kinds of plate which is the less invasive stabilization system (LISS-) proximal tibia (-PT) or locking compression plate (LCP-) proximal lateral tibia (-PLT), using the percutaneous plate osteosynthesis technique at the authors’ institutions from June 2009 to June 2014.
Besides preoperative X-ray, CT-scan with three-dimensional (3D) reconstruction was obtained for further investigation in order to identify the size, location, and extension of the articular fragments [9]. Depending on more detailed information from 3D-CT, the fracture involvement area and fracture line orientation could be highly variable, and the medial articular surface may or may not have been violated. Exclusion criteria were cases that have no evidence of coronal shearing fractures in medial condyle. In clinical practice, the coronal posteromedial fragment is difficult to stabilize through a lateral less invasive approach with a single lateral locking plate [10]. According to the AO and the Orthopaedic Trauma Association (OTA) system [11], the fractures were classified as types 43-C1 (n=3), 43-C9 (n=11) and 43-C3 (n=6). The causes of injury were motor vehicle crashes (16 patients) and falls (4 patients). Open fractures were seen in twelve patients and included Gustilo-Andersen I fractures [12]. In three patients; II in four; IIIA in five. There was no major neurovascular injury. Patient and fracture characteristics are summarized in Table 1, which provides the detailed data for the 20 cases.
Table 1.
Fracture characteristics
| Variable | No. |
|---|---|
| Male/female | 15/5 |
| Age | 35.8 years (range, 25-58 years) |
| Right/left | 7/13 |
| Mechanism of injury | |
| Motor vehicle crash | 16 (80%) |
| Fall | 4 (20%) |
| Isolated fracture | 13 (65%) |
| Multiple fractures | 5 (25%) |
| Polytrauma | 2 (10%) |
| Fracture type | |
| 41-C1 | 3 (15%) |
| 41-C2 | 11 (55%) |
| 41-C3 | 6 (30%) |
| Distal fracture extension | |
| The proximal third of the tibial shaft | 14 (70%) |
| The middle of the tibial shaft | 6 (30%) |
| Closed | 8 (40%) |
| Open | 12 (60%) |
| Gustilo-Andersen I | 3 (15%) |
| Gustilo-Andersen II | 4 (20%) |
| Gustilo-Andersen IIIA | 5 (25%) |
In this study, the timing of surgery depended on the soft-tissue conditions, and surgery was delayed if the fractures had established severe swelling and skin blister. Patients who had open fractures underwent debridement and then MIPO after no signs of infection. Waiting for surgery, all patients were treated with transcalcaneal traction or external fixator. The mean time elapsed from injury to definitive surgical treatment was 7 days (range 0-14 days). Five patients sustained multiple fractures, which included ipsilateral ankle fractures and patellar fractures. They were successfully managed by combining internal fixation techniques frequently employed for the treatment of each of these injuries.
For surgery, patients were positioned supine on a radiolucent table. The ipsilateral iliac crest was prepared and draped for possible autogenous bone grafting.
With this surgery strategy of a single lateral locked plating/MIPO is first turned type C fracture into type A fracture by reconstructing the articular fragments as a single articular block. Then the metadiaphyseal component is bridged with submuscular plating usually from the lateral side. The typical sequence of lateral locked plating can be outlined as follows:
• Articular fracture reduction and fixation;
• Indirect reduction of the reconstructed articular block to the diaphysis;
• Percutaneous locking plate insertion and fixation.
Articular displaced split fractures were reduced indirectly by a reduction forceps under image intensifier. For centrally depressed articular fragments (when reduction was not feasible by ligamentotaxis), a window through the cortical bone was made in the subchondral metaphyseal region. For bad results closed reduction may be conducted, the articular surface was visualized with a small arthrotomy. Once the elevation of the depressed articular fragments was done and the lateral split fragment is reduced to the medial condyle, subchondral screws were placed using 3.5 mm cortex screws. In some cases, screws were not placed in the proximal part of the lateral plate to avoid interfering with the reduction and bone grafting of the depressed part of tarticular surface that was often performed via the anterolateral approach.
A lateral curved incision was made from the Gerdy tubercle extending distally for about 5.0 cm. The metaphyseal and diaphyseal component of the fracture was reduced using indirect reduction methods. The restoration of the length was the most crucial step. Otherwise, the metadiaphyseal component was reduced and aligned by manual longitudinal traction, pointed reduction forceps, collinear reduction clamp, et al. If necessary, we performed direct reduction through the open trauma wound with short extending incisions as needed for access. An acceptable alignment (less than 5° in sagittal and coronal plane, less than 10° in rotation) is achieved.
Then the locking plate was introduced submuscularly through an anterolateral approach. The position of the plate was verified with image intensifier images in both AP and lateral views along the axis of the tibia. Reconfirmation of fracture reduction was then performed with image intensifier before the plate was confirmed the plate is provisionally fixed to the bone using two 2.0 mm K-wires inserted proximally and distally. One bicortical locked screw was placed in the end hole of plate at site of insertion, and then a second screw was inserted at the opposite end of the plate through a stab incision. Check fluoroscopy images was repeated. Final fixation was achieved with locking screws at either end of the plate. A total of four or five 5.0 mm locking screws were placed to the proximal fragment and three or four screws were placed in the shaft fragment. This construct aimed for combining absolute stability by fixed angle stability and relative stability by bridging technology. After fixation, the stability of the knee joint should always be checked.
To achieve early functional restoration of the limb, both passive and active joint motion of the knee joint must be started as soon as possible. The amount of weight bearing should be tailored according to the fracture fixation construct. Usually partial weight bearing could begin around 6 weeks postoperatively and progressively increased weight bearing depends on both clinical and x-ray findings.
Results
In all cases, a MIPO technique via minimally invasive lateral incision was feasible (Figure 1 and Figure 2). However, in cases with inadequate soft tissue coverage, given the need for a brief operation due to general skin condition, and the presence of a severely contaminated wound, eighteen patients were treated by staged MIPO. The articular surface was visualized with a small arthrotomy in fourteen cases. Proximal condylar fixation and bridging of metadiaphyseal dissociation or comminution was achieved by LCP-PLT and LISS-PT in screw holes 9, 11, 13. With these large plating systems, the 5.0 mm locked screws and 4.5 mm cortex screws are used. The differences and function of large systems are summarized in Table 2. In some cases, through the percutaneous lag screw was it utilized for reduction and additional fixation though lag screws of the medial or lateral condyle and one, two or three lag screws were placed into the metadiaphysis component of the fractures. Primary bone grafting in four cases was used to reduce articular step off and increase high union rates.
Figure 1.
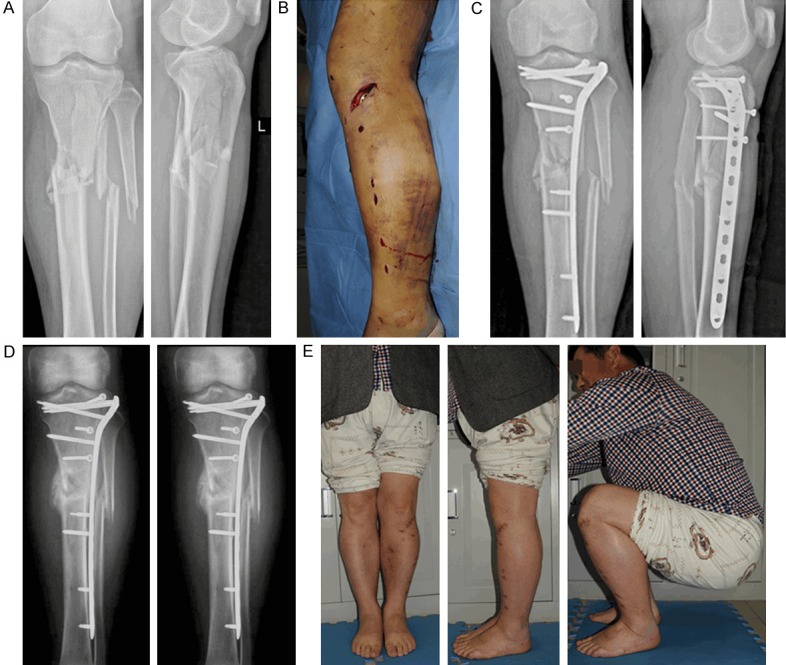
52-year-old man with a proximal tibial fracture with diaphyseal involvement (A) treated with percutaneous plating using a single locking plate on the lateral side (B). (C) After operation, good alignment was achieved on the coronal and sagittal planes. (D, E) The fracture was healed 14 weeks after surgery and the patient recovered the good functional outcome.
Figure 2.
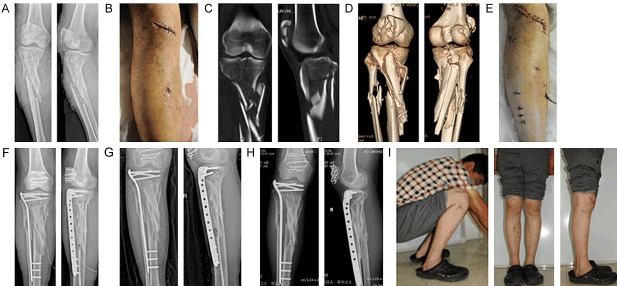
The patient is a 40 year-old man. A. Preoperative x-rays show a multifragmentary fracture of the proximal tibia involving articular and extending into the diaphysis. B. Meanwhile comminuted patellar fracture can also be seen. The first-stage operations were debridement and transcalcaneal traction. C and D. 3D-CT scans showed the extent and location of the articular fragments. Note that displacement of tibial intra-articular fracture was not obvious. E. Sutured skin incisions. The surgical strategy was a single lateral locking plate using MIPO technology in treatment of complex proximal tibial fracture. And Patellar fracture was treated by open reduction with tension band wiring fixation. F. Postoperative x-rays show good joint congruency and acceptable gross alignment but loss of reduction at the middle segment due to the coronal split at the middle segment. G. X-rays taken 6 months postoperatively show bridging callus formation along the metaphyseal area except the diaphyseal fracture site where there was a significant gap. H and I. The fracture healed in good alignment and clinical images show near full-joint motion 13 month postoperative.
Table 2.
Surgical details
| Variable | No. |
|---|---|
| Primary/staged | 2/18 |
| Pre-surgical stay | 7 days (range, 0-14 days) |
| Surgical time | 118 min (range, 70-370 min) |
| Incision size | |
| Proximal | 6 cm (range, 4-10 cm) |
| Distal | (3-4)*0.8 cm |
| LISS-PT size | |
| 9-hole | 4 (20%) |
| 11-hole | 6 (30%) |
| 13-hole | 3 (15%) |
| LCP-PLT size | |
| 9-hole | 2 (10%) |
| 11-hole | 4 (20%) |
| 13-hole | 1 (5%) |
| Lag screws | |
| Yes | 9 (45%) |
| No | 11 (55%) |
| Primary bone grafting | 4 (20%) |
| Bone grafting in the treatment of nonunion | 1 (5%) |
Table 3 reports outcomes as witnessed by final follow up in June 2014. All patients achieved union of their fracture. The mean follow-up duration for the study was 15.6 months (range, 12-42 months). Radiological criteria were represented by fracture consolidation, by signs of implant mobilization and by broken screws. Clinical criteria were represented by axial deviation (varus/valgus), by infection signs, and by range of motion (ROM) and HSS [13] scores at the final evaluation.
Table 3.
Post-operative complications and outcomes
| Variable | No. |
|---|---|
| Radiographic healing time (months) | 4±1.2 months |
| Delayed union | 3 (15%) |
| Nonunion | 1 (5%) |
| complications | |
| Radiologic Malreduction | |
| Articular step-off | 1.0 mm (range, 0-3 mm) |
| Valgus | 2 (7°, 8°) |
| Varus | 0 |
| Secondary Loss of reduction | 1 (5%) |
| screw loosening, implant failure | 0 |
| Would infection | 1 (5%) |
| Knee joint function | |
| ROM | |
| ≥120° | 16 (80%) |
| <120° | 4 (20%) |
| HSS (points) 12 months | 87.4 (range, 60-97) |
| Implants removal | 10 (50%) |
16 of 20 patients (80%) had uneventful healing of the fractures, which were considered radiographically healed at 4±1.2 months after surgery. Mean time to full weight bearing was 16±2.2 weeks.
Delayed union was seen in three patients (15%). Nonunions were established in one patient (5%). In delayed unions, the consolidation of fractures and possibility of full weight bearing were achieved by 6 to 8 months without additional intervention. In nonunion, additional surgeries were performed: bone grafting though minimally invasive incision. On the follow-up x-ray there was loss of reduction of the middle fragment in one case. Revision surgery to correct this loss of reduction was not performed because the loss of reduction did not affect the length and alignment of the tibia and the entire construct seemed to have a stable and balanced fixation. There was a significant delay in healing at the diaphyseal gap. An autogenous bone graft was performed 8 months after the initial operation. The fracture showed good healing 3 months later.
Clinical examination revealed rotational malunion in two patients (7°, 9°). The mean articular step off was 1.0 mm (range, 0-3 mm). Average shortening of 1 cm was observed in two patients who had severe proximal tibial metaphyseal comminution. Misalignment exceeding 5° in the frontal plane occurred in two (10%) patients (valgus 7°, 8°). Acceptable range of knee motion of ≥120° was achieved in sixteen, one patient had fixed knee flexion with a mean of 7.6° (6-9°). And the mean HSS score was 87.4 (range, 60-97).
No deep infection was detected. In one patient (5%) the wound was reopened because of a superficial infection. The infection was cured by one revision. No patients had clinical signs of infection at the latest follow up. In addition, no screw loosening, implant failure, or other complications occurred in this series.
Discussion
The purpose of this article is to report the clinical and radiological outcome of percutaneous lateral locked plating (PLP) in the treatment of complex proximal tibial fractures which extend into the diaphyseal region of the bone. The intra-articular fractures with complete metaphyseal-diaphyseal separation are classified as type C. These fractures are more often associated with high-energy trauma, and soft tissue injury is common. Proper management of the soft tissues is imperative in injuries of the complex proximal tibia. Open fractures must be appropriately treated with emergency debridement and temporary external fixation [14]. The second stage procedure protocol using a minimally invasive plate osteosynthesis (MIPO) technique should be performed when skin conditions get better [15]. The purpose of the MIPO in the treatment of the complex proximal tibial fractures are rapid and optimal healing, minimization of any soft tissue complication and loss of function, and the prevention of non-union or malunion [2,3,16]
With the damaged soft tissue after the high energy of proximal tibial fractures, conventional open reduction and internal fixation have often resulted in significant soft-tissue complications, such as wound breakdown and deep infection [17,18]. The surgical method devitalizes soft tissues or cause further injury to surrounding structures. Intramedullary nailing is the most commonly used method of minimally invasive stabilization for long bone fractures. However, misalignments in coronal and sagittal planes are common because of the insufficient stability of the nail with regard to the geographic characteristics of proximal tibial shaft fractures [19]. The small wire external fixator is a also good option for these injuries, but the problems of nonunion and pin track infection are common [20,21]. These characteristics may make locked plating as an attractive option for treating complex fractures of the proximal tibia. Along with the development of MIPO, the popularity of locking plates for the treatment of these complex fractures has significantly increased [22]. The locking internal flxator (LIF), which includes LCP-PLT and LISS-PT, is particularly effective in severely osteoporotic bone, substantial metaphyseal-diaphyseal comminution, and larger-segment periarticular intra-articular fractures. Both of them are anatomically preshaped locking plates, are the most common implants used for MIPO on the lateral side. Percutaneous fixation of proximal tibia with the above plates has shown promising results [3,23]. Again, cases were comminuted, multilevel proximal tibia fractures with diaphyseal involvement comprising a large segmental component, so the plates of appropriate length must be chosen to achieve a mechanically sound fixation which is the key to allowing healing through callus [24].
Fixation of bicondylar tibial plateau fractures is more controversial. Stabilization can be accomplished with locking screws placed through a laterally based implant alone or stabilized with a medial plate as part of a dual plating construct (medial and lateral plate) [25-27]. Biomechanical and clinical data support both techniques. Double plate generally involves two separate incisions, which can lead to extensive soft tissue dissection and periosteal injury. This technique risks result to delayed union or non-union of proximal tibial fractures, even in the most expert hands. When displacement of the medial fragment could be avoided, lateral-only locked plates should reduce surgical time, reduce blood loss, and limit soft-tissue stripping.
Gosling T et al, in a study of 63 AO/ASIF C-type tibial plateau fractures, reported that unilateral plating with locking head screws is a reasonable option for treatment of bicondylar tibial plateau fractures [25]. As tested in Lindeque B’ study, the lateral locking plate provides rigid stability in the proximal tibia fracture and it can withstand normal physiological loading [28]. In 2012, Rosario Spagnolo et al [29] proposed the lateral locked screw plating treatment for the management of these fractures, and reported a good clinical efficacy.
In our study, the preferred surgical strategy have been the anterolateral single incision with a lateral locking plate for stable fixation of intra-articular fractures and better fracture healing. In our experience, the fracture patterns of the medial condyle may be the main indications for this surgical strategy.
The rigidity of the lateral locked plate construct in fixation of metadiaphyseal fractures was clearly evident from a study by Naik MA. It bridges the component of metadiaphyseal comminution creating less soft-tissue damage to the surrounding soft tissue envelope than occurs with conventional plating [30]. This construct, using the natural properties of the metal strut fixed at its ends over a controlled distance is seen in ‘leaf spring’ suspension [24]. In comminuted fractures flexible fixation using the bridge plate concept without touching the fracture zone is preferred. We observed a tendency towards better healing with this method due to the improved elasticity of the bone-plate complex without any high degree of instability of the intercalary bone segment. This technique has proven advantages of undisturbed fracture healing when compared to ORIF [3,16]. Although separation of fractures was not violated using a MIPO technique, healing of the diaphyseal component of the tibial fractures may be delayed due to a significant gap, which should be prevented by using certain well-described preventative measures. Minimally invasive cerclage wiring to achieve better reduction between the diaphyseal fragments could have been carried out resulting in closing of the fracture gap as there was a coronal split of the middle fragment. A small medial plate or temporary external fixator on the medial side may be another option to prevent varus collapse.
The absence of secondary displacement of metadiaphyseal segment and of worsening of articular step-offs establishes the effectiveness of a single lateral locked plate in this indication in our study. Because of the unstable nature of the intercalary segment, reduction is frequently difficult and axial misalignment poses another potential issue. Some studies report bad outcomes after a single lateral locked plating of complex proximal tibial fractures. Malreduction rates ranged from 0% to 23% and loss-of-reduction rates from 0% to 14% [6-8,31,32]. We recorded two Valgus cases (10%) and one case (5%) of secondary displacement. Again we also found two cases occurring articular step-off, but in our experience, articular step-offs do not seem to impact the radio-clinical results in the short-term. The ROM and HSS score results in our study are highly satisfactory, and all employed patients were able to return to their previous job. In this series, wound complication was found in one patient (5%) in group, and the patients sustained open fracture injury. The rate of wound complication obviously depends on severity of initial trauma and degree of soft tissue injury. The incidence of wound infections can be reduced by performing surgery after stabilization of soft tissue status, use of prophylactic antibiotics, and maintaining complete asepsis during surgical procedure.
The limitations of the study include the following. Minimally invasive surgery is possible but is highly demanding and technically challenging in patients with complex proximal tibial fractures. Considerable experience is required. Medial fragment fixation may not rely on a single lateral locking plate to stabilize the fracture line located chiefly in the coronal plane. Many styles of bone graft requiring adequate exposure of the graft site in metadiaphyseal component is limited by minimally invasive incision in MIPO technology.
There is no comparative group, and hence, it is difficult to predict whether the surgical strategy is the better treatment or not.
Conclusion
A single lateral locking plate using MIPO technology ensured good outcomes in treatment of proximal tibial fractures (AO/OTA type 41-C) with diaphyseal involvement. The surgical strategy is useful as the imaging study results were stable over time and the short-term clinical outcomes were satisfactory. Of course, we suggest that further long-term research including large number of patients to make the conclusion further perfection.
Disclosure of conflict of interest
None.
References
- 1.Savolainen VT, Pajarinen J, Hirvensalo E, Lindahl J. Hybrid external fixation in treatment of proximal tibial fractures: a good outcome in AO/ASIF type-C fractures. Arch Orthop Trauma Surg. 2010;130:897–901. doi: 10.1007/s00402-009-0931-8. [DOI] [PubMed] [Google Scholar]
- 2.Singh S, Patel PR, Joshi AK, Naik RN, Nagaraj C, Kumar S. Biological approach to treatment of intra-articular proximal tibial fractures with double osteosynthesis. Int Orthop. 2009;33:271–4. doi: 10.1007/s00264-007-0480-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oh JK, Oh CW, Jeon IH, Kim SJ, Kyung HS, Park IH, Kim PT, Ihn JC. Percutaneous plate stabilization of proximal tibial fractures. J Trauma. 2005;59:431–7. doi: 10.1097/01.ta.0000174733.67446.83. [DOI] [PubMed] [Google Scholar]
- 4.Gary JL, Sciadini MF. Injury to the anterior tibial system during percutaneous plating of a proximal tibial fracture. Orthopedics. 2012;35:e1125–8. doi: 10.3928/01477447-20120621-37. [DOI] [PubMed] [Google Scholar]
- 5.Perren SM. Fracture healing. The evolution of our understanding. Acta Chir Orthop Traumatol Cech. 2008;75:241–6. [PubMed] [Google Scholar]
- 6.Beck M, Gradl G, Gierer P, Rotter R, Witt M, Mittlmeier T. Treatment of complicated proximal segmental tibia fractures with the less invasive stabilization locking plate system. Unfallchirurg. 2008;111:493–8. doi: 10.1007/s00113-008-1427-7. [DOI] [PubMed] [Google Scholar]
- 7.Haiduewych G, Sems SA, Huebner D, Horwitz D, Levy B. Results of polyaxial locked-plate fixation of periarticular fractures of the knee. Surgical technique. J Bone Joint Surg Am. 2008;90(Suppl 2):117–34. doi: 10.2106/JBJS.G.01086. [DOI] [PubMed] [Google Scholar]
- 8.Phisitkul P, McKinley TO, Nepola JV, Marsh JL. Complications of locking plate fixation in complex proximal tibial injuries. J Orthop Trauma. 2007;21:83–91. doi: 10.1097/BOT.0b013e318030df96. [DOI] [PubMed] [Google Scholar]
- 9.Tscherne H, Lobenhoffer P. Tibial plateau fractures. Management and expected results. Clin Orthop Relat Res. 1993;292:87–100. [PubMed] [Google Scholar]
- 10.Chang SM, Zhang YQ, Yao MW, Du SC, Li Q, Guo Z. Schatzker Type IV Medial Tibial Plateau Fractures: A Computed Tomography–based Morphological Subclassification. Orthopedics. 2014;37:e699–706. doi: 10.3928/01477447-20140728-55. [DOI] [PubMed] [Google Scholar]
- 11.Fracture and dislocation compendium. Orthopaedic Trauma Association Committee for Coding and Classification. J Orthop Trauma. 1996;10(Suppl 1):v–ix. 1–154. [PubMed] [Google Scholar]
- 12.Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58:453–458. [PubMed] [Google Scholar]
- 13.Ranawat CS, Shine J. Duo condylar total knee arthroplasty. Clin Orthop. 1973;94:185–95. doi: 10.1097/00003086-197307000-00023. [DOI] [PubMed] [Google Scholar]
- 14.Krieg JC. Proximal tibial fractures: Current treatment, results, and problems. Injury. 2003;34(Suppl 1):A2–10. doi: 10.1016/s0020-1383(03)00252-3. [DOI] [PubMed] [Google Scholar]
- 15.Ma CH, Wu CH, Yu SW, Yen CY, Tu YK. Staged external and internal less-invasive stabilisation system plating for open proximal tibial fractures. Injury. 2010;41:190–6. doi: 10.1016/j.injury.2009.08.022. [DOI] [PubMed] [Google Scholar]
- 16.Farouk O, Krettek C, Miclau T, Schandelmaier P, Guy P, Tscherne H. Minimally invasive plate osteosynthesis: does percutaneous plating disrupt femoral blood supply less than the traditional technique? J Orthop Trauma. 1999;13:401–406. doi: 10.1097/00005131-199908000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Schatzker R, McBroom J. The tibial plateau fracture. Clin Orthop. 1979;138:94–104. [PubMed] [Google Scholar]
- 18.Lachiewicz PF, Funcik T. Factors influencing the results of open reduction and internal fixation of tibial plateau fractures. Clin Orthop. 1990;259:210–215. [PubMed] [Google Scholar]
- 19.Freedman EL, Johnson EE. Radiographic analysis of tibial fracture malalignment following intramedullary nailing. Clin Orthop. 1995;315:25–33. [PubMed] [Google Scholar]
- 20.Ali AM, Burton M, Hashmi M, Saleh M. Outcome of complex fractures of the tibial plateau treated with a beam-loading ring fixation system. J Bone Joint Surg Br. 2003;85:691–699. [PubMed] [Google Scholar]
- 21.Murphy CP, D’Ambrosia R, Dabezies EJ. The small pin circular fixator for proximal tibial fractures with soft tissue compromise. Orthopedics. 1991;14:273–280. [PubMed] [Google Scholar]
- 22.Ma CH, Wu CH, Yu SW. Minimally Invasive Plate Osteosynthesis for Open Fractures of the Proximal Tibia. Injury. 2010;41:190–6. [Google Scholar]
- 23.Lindvall E, Sanders R, Dipasquale T, Herscovici D, Haidukewych G, Sagi C. Intramedullary nailing versus percutaneous locked plating of extraarticular proximal tibia fractures: comparison of 56 cases. J Orthop Trauma. 2009;23:485–92. doi: 10.1097/BOT.0b013e3181b013d2. [DOI] [PubMed] [Google Scholar]
- 24.Williams TH, Schenk W. Bridging-minimally invasive locking plate osteosynthesis (Bridging-MILPO): Technique description with prospective series of 20 tibial fractures. Injury. 2008;39:1198–203. doi: 10.1016/j.injury.2008.05.008. [DOI] [PubMed] [Google Scholar]
- 25.Gosling T, Schandelmaier P, Muller M, Hankemeier S, Wagner M, Krettek C. Single lateral locked screw plating of bicondylar tibial plateau fractures. Clin Orthop Relat Res. 2005;439:207–214. doi: 10.1097/00003086-200510000-00036. [DOI] [PubMed] [Google Scholar]
- 26.Eastman J, Tseng S, Lo E, Li CS, Yoo B, Lee M. Retropatellar technique for intramedullary nailing of proximal tibia fractures: A cadaveric assessment. J Orthop Trauma. 2010;24:672–676. doi: 10.1097/BOT.0b013e3181c1d675. [DOI] [PubMed] [Google Scholar]
- 27.Higgins TF, Klatt J, Bachus KN. Biomechanical analysis of bicondylar tibial plateau fixation: How does lateral locking plate fixation compare to dual plate fixation? J Orthop Trauma. 2007;21:301–306. doi: 10.1097/BOT.0b013e3180500359. [DOI] [PubMed] [Google Scholar]
- 28.Lindeque B, Baldini T. Biomechanical comparison of three different lateral tibia locking plates. Orthopedics. 2010;33:18–21. doi: 10.3928/01477447-20091124-25. [DOI] [PubMed] [Google Scholar]
- 29.Spagnolo R, Pace F. Management of the Schatzker VI fractures with lateral locked screw plating. Musculoskelet Surg. 2012;96:75–80. doi: 10.1007/s12306-011-0173-0. [DOI] [PubMed] [Google Scholar]
- 30.Naik MA, Arora G, Tripathy SK, Sujir P, Rao SK. Clinical and radiological outcome of percutaneous plating in extra-articular proximal tibia fractures: a prospective study. Injury. 2013;44:1081–6. doi: 10.1016/j.injury.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 31.Higgins TF, Klatt J, Bachus KN. Biomechanical analysis of bicondylar tibial plateau fixation: how does lateral locking plate fixation compare to dual plate fixation? J Orthop Trauma. 2007;21:301–6. doi: 10.1097/BOT.0b013e3180500359. [DOI] [PubMed] [Google Scholar]
- 32.Biggi F, DiFabio S, D’Antimo C, Trevisani S. Tibial plateau fractures: internal fixation with locking plates and the MIPO techniques. Injury. 2010;41:1178–82. doi: 10.1016/j.injury.2010.08.001. [DOI] [PubMed] [Google Scholar]


