Abstract
Background: Child-Turcotte-Pugh (CTP) and the model for end-stage liver disease (MELD) scores have been used commonly to predict the survival in the patients with liver diseases underwent transjugular intrahepatic portosystemic shunt (TIPS). However, a debate has continued for years whether CTP could be replaced by MELD score. We performed a systematic meta-analytic review to compare the prediction capability of both scores in survival among patients with TIPS. Methods: Retrospective cohort studies among patients with TIPS were published as of May 2013 were identified by systematically searching four electronic literature database, such as Ovid Medline, PubMed, EMBASE, and ISI Web of Science. The difference of standardized mean difference (SMD) of c-statistics for the predictive accuracy of 1-, 3-, 6-, and 12-month survival for both MELD and CP scores, defined as effect size (ES), was calculated for each individual study and then pooled across studies using standard meta-analyses with a random effects model. Publication bias was evaluated using funnel plots and Kendall’s rank correlation tests. Results: 174 researches articles or conference abstracts were searched and reviewed using the combination of relevant terms in the articles. Finally, 11 articles were defined as eligible studies to evaluate simultaneously the predictive accuracy of MELD and CTP scores. In the meta-analyses, MELD score was superior to CP score in predicting 3-month survival after TIPS (mean ES, 0.63; 95% confidence interval [CI], 0.13-1.14; P=0.01), but the predictive capability in 1-month, 6-month, and 12-month survival was not significant (1-month: mean ES, 0.79; 95% CI, -0.24-1.83; P=0.13; 6-month: mean ES, 0.46; 95% CI, -2.46-3.37; P=0.76; 12-month: mean ES, 0.36; 95% CI, -0.25-0.96; P=0.25). Conclusions: No enough evidence are confirmed so far that MELD score is better than CTP score to assess the overall prognosis after TIPS, especially long-term predictions, but 3-month predictive capability of MELD score significantly outperform CTP score.
Keywords: Transjugular intrahepatic portosystemic shunt (TIPS), the model for end-stage liver disease (MELD) score, Child-Turcotte-Pugh (CTP) score, systematic review, meta-analysis
Introduction
Transjugular intrahepatic portosystemic shunt (TIPS) has been demonstrated as an effective procedure to treat esophageal variceal hemorrhage and refractory ascites due to portal hypertension [1,2], compared with medical treatment and endoscopic treatment. The patient prognosis of TIPS placement was improved significantly along with the development from bare stents to covered stents, such as the FLUENCY expanded, polytetrafluoroethylene (PTFE) -covered stents in the past two decades [3-5]. However, TIPS techniques were not perfect because of its potential dysfunction and costs of re-intervention [6,7]. Hence, careful selection of patients is crucial to increase the success rate and cost-effectiveness of TIPS replacement.
Several scoring systems have been developed to identify suitable patients for TIPS [8,9]. Of these, Child-Turcotte-Pugh (CTP) and the model of end-stage liver diseases (MELD) scores were the most common to predict the survival in patients underwent TIPS, which were validated using several individual studies across US, Europe and Asia [8-19]. Child and Turcotte [20] first proposed a score to assess and classify the risk in cirrhotic patients in 1964, which were modified by Pugh and his colleagues in 1973 [21]. Subsequently, this classification was defined as Child-Turcotte-Pugh (CTP) score, which was more and more to be used to predict the outcome of cirrhosis patients with or without surgery due to its convenience and reliable classification, including liver-transplantation and TIPS [22-24]. Because of its reproducibility and objectivity, MELD score was reported as a novel and better prognostic score superior to the CTP score in some studies, especially short-term survival [10,11,14,15,17].
However, results from single studies have remained inconclusive and study results have been reported in a very heterogeneous manner. Based on a systematic review published in 2005, MELD scores did not performed better than CTP scores in predicting the survival among patients underwent TIPS, but no meta-analyses were conducted [25]. In addition, several recent studies [8,9,15-19] were reported after this systematic review [25]. To our knowledge, this is the first to perform a meta-analysis for assessing the difference of predictive accuracy between MELD and CTP scores in survival among patients after TIPS.
Methods
Literature search and study selection
The PRISMA statement for reporting systematic reviews and meta-analyses of studies was used for our study [26]. A systematic literature search was performed to identify retrospective cohort studies that evaluate the predictive capability of both MELD and CTP scores using c-statistics based on the area under the Receiver Operator Characteristic (ROC) curve in survival among patients underwent TIPS placement. We searched Ovid Medline (Ovid Technologies, Inc., New York, 1946-May 20, 2015), PubMed (National Center for Biotechnology Information (NCBI) at the U.S. National Library of Medicine (NLM), the National Institutes of Health (NIH), up to May 20, 2015), EMBASE (Elsevier, Amsterdam, the Netherlands, 1980-May 19, 2015), ISI Web of Science (Thomson Scientific Technical Support, New York, 1956-May 20, 2008) databases for relevant articles by the following combinations of relevant terms in the article: (Transjugular intrahepatic portosystemic shunt OR TIPS OR transjugular intrahepatic portosystemic stent-shunt OR TIPSS) AND (Child-Pugh OR Child-Turcotte-Pugh) AND (Model For End Stage Liver Disease Score OR MELD). All publications were imported into an Endnote file (Endnote X4, Thomson Reuters, San Francisco, CA), and the duplicates were deleted. Each title and abstract was checked for relevance. The full text was reviewed if the abstract indicated that the article reported predictive values of both MELD and CTP scores for the survival among patients after TIPS. Cross-referencing was employed to complement the study identification process.
Inclusion criteria and data extraction
Studies were defined as eligible if they 1) used prospective or retrospective cohort study design to predict the survival after TIPS replacement; 2) calculated MELD and CTP before TIPS for each patient; 3) reported c-statistics based on the area under the ROC curve for both MELD and CTP and 95% confidence intervals (CI), which are used to calculate effect size (ES) estimates in our meta-analyses; 4) published in all languages.
From eligible studies, at least two authors extracted the following data independently from each study in a standardized manner, and any disagreement was resolved by consensus: authors, publication year, country, enrollment period, characteristics of the study population, duration of follow-up, mean of MELD and CTP scores before TIPS replacement, overall mortality at the end of follow-up, as well as c-statistics and their 95% CI based on areas under the ROC curve at the various follow-up months. If such data were not explicitly reported or were presented in non-English and non-Chinese, they were derived from data provided in the articles or requested from the authors through email contacts, wherever possible [9,11,14-16,19].
CTP and MELD scores
CTP score was calculated using the five following point assignment scheme: 1) bilirubin (assigned <2 mg/dL, 2-3 mg/dL, and >3 mg/dL to 1, 2, and 3 points, respectively); 2) albumin (>3.5 g/dL: 1 point; 3.5-2.8 g/dL: 2 points; <2.8 g/dL: 3 points); 3) prothrombin time (<4 second accounted for 1 points, 4-6 second for 2 points, and >6 second for 3 points); 4) ascites (absent counted as one point, mild to moderate as two points, and severe or refractory as three points); 5) encephalopathy categorized absent, mild, and severe as 1, 2, 3 points. Five above-mentioned schemes were summed as CTP score. CTP were classified as Class A (5-6 points), Class B (7-9 points), and Class C (10-15 points) [21]. The MELD score was calculated using the total serum bilirubin, serum creatinine and international normalized ratio (INR) as the following formula: 3.78× In (bilirubin [mg/dL]) +11.2× In (INR) +9.57× In (serum creatinine [mg/dL]) +6.43 [27,28].
Rigor score
The rigor of study quality for retrospective cohort studies was evaluated using a 6-item scale and one point awarded for each of the following items: 1) follow-up rate of 80% or more after excluding death cases; 2) sample size of 200 or more; 3) means of both MELD and CTP scores before TIPS reported; 4) median duration after TIPS of 6 months or longer; 5) c-statistics and 95% CI for both MELD and CTP scores reported; 6) socio-demographic characteristics of patients before TIPS described. If any above-mentioned items were not presented in original articles or obtained via personal contacts, 0 was counted.
Statistical methods
All cohort studies that were included in our meta-analyses had the c-statistics for MELD and CTP scores at least one follow-up time point after TIPS replacement. Stratified analyses at the different follow-up time points were used to evaluate the difference of predictive accuracy between MELD and CTP scores in the short-term and long-term survival after TIPS replacement. Standard mean differences (SMD) of c-statistics between MELD and CTP scores, defined as effect size (ES), was calculated for each study and then pooled across studies using standard meta-analysis with a random effects model [29], which allow for variation of true effects across studies, were taken as “main results” [30]. Random effects estimates were derived using the DerSimonian-Laird method [31,32]. A negative value of SMD indicates that CTP score is superior to MELD, and vice versa. Standardized deleted residuals analysis was done to identify outliers. The robustness of results to this predictive difference was assessed in sensitivity analyses that removed outlier studies. Heterogeneity was additionally assessed by the I2 statistic. The funnel plot, and Begg and Mazumdar rank correlation tests were employed to assess indications of publication bias [33]. All meta-analyses were performed in the R/S plus software, version 3.2.1 [34].
Results
Results of literature search
A flow diagram of the search process is provided in Figure 1. Total searches from four electronic literature databases using targeting term combination yielded 294 entries. After excluding 121 duplicates, 173 titles and abstracts were reviewed and 122 studies appeared to be potentially relevant to our topic. 110 articles or conference abstracts were deleted due to the following reasons: no original studies but editorials, comments, reviews or meta-analyses (n=13), no relevant data were provided (n=79), no TIPS performed (n=10), repeated studies with included studies in our meta-analyses [22,35-39] (n=6), and no c-statistics for CTP were reported 40-42 (n=3). Finally, the remaining 11 studies were included in our meta-analytic review [8-11,13-19].
Figure 1.
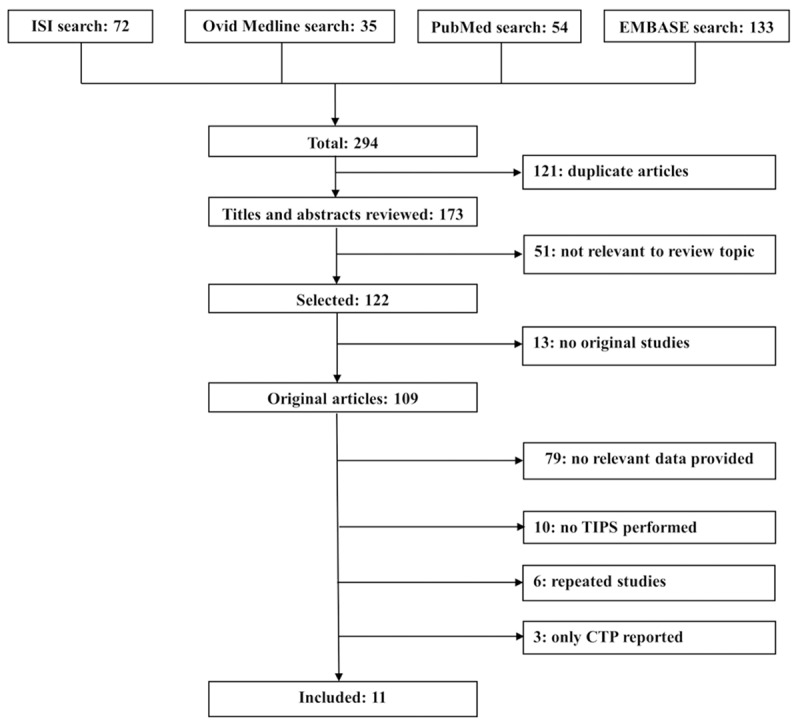
Flow diagram of the literature search process.
Characterization of Individual studies
Details on the respective study design, the study populations and the study results are shown in Table 1. Among these 11 eligible studies involving 2037 patients with TIPS replacements during 1991-2013, 5 studies were from European countries [10,11,13,15,18], three from USA [9,14,16], and three from China [8,17,19]. Overall mortality at the end of follow-up ranged from 10%-80%. Five studies reported the predictive capability of both MELD and CTP scores in 1-month survival among patients after TIPS replacement [9,11,14,15,17], seven reported for 3-month survival [9-11,13-16], two for 6-month survival [10,14], nine for 12-month survival [8,10,11,13,15-19], and one for 24-month 8 and one for 36-month survival [13]. Rigor scores were obtained, ranging from 0 to 6, with a mean of 3.6. Only one study had a full score of 6.
Table 1.
General information of included retrospective cohort studies at study enrollment
| Authors (year) | No. of patients | Country | Enrollment period | Months of follow-up | Mean patient age | Patient male % | Mean MELD | Mean CTP | Mortality (%) | Rigor score |
|---|---|---|---|---|---|---|---|---|---|---|
| Salerno et al. [10], 2002 | 140 | Italy | 1993-2000 | 23.7 (0.3-93) | 60.5 | 64.3 | 0.9 | 8.0 | 39.2 | 5 |
| Angermayr et al. [11], 2003 | 475 | Austria | 1991-2001 | 62.4 (0.04-116.4) | 56.0 | n/a | 7.0 | 8.7 | 48.4 | 3 |
| Schepke et al. [13], 2003 | 162 | Germany | 1992-2001 | 30.7±26.4 | 57.0 | 64.2 | 6.7 | 8.1 | 50.0 | 5 |
| Ferral et al. [14], 2004 | 166 | USA | 1999-2002 | 11.0 (0.1-42.8) | 52.5 | 62.7 | 15.3 | 9.3 | 71.8 | 4 |
| Fejfar et al. [15], 2006 | 110 | Czech | 1992-2003 | n/a | 55.0 | n/a | n/a | n/a | n/a | 0 |
| Stewart et al. [16], 2007 | 223 | USA | 1994-1999 | 11.9 (0-46.1) | 56.0 | n/a | 15.0 | 10.0 | 49.3 | 3 |
| Tzeng et al. [17], 2009 | 107 | China | 1995-2006 | 36 | 55.5 | 69.2 | n/a | n/a | 76.6 | 3 |
| Zipprich et al. [18], 2010 | 74 | Germany | 1995-2004 | 39 (0.5-129) | 51.0 | 62.0 | 11.9 | 8.0 | 62.0 | 4 |
| Chen et al. [19], 2013 | 210 | China | 2010-2013 | 12 | 47.2 | 69.5 | 9.9 | 7.0 | 18.1 | 4 |
| Gaba et al. [9], 2013 | 211 | USA | 1999-2011 | 3 | 54.0 | 62.0 | 17.0 | 9.0 | 29.0 | 3 |
| Zhang et al. [8], 2014 | 159 | China | 2008-2013 | 21 (1-65) | 52.0 | 71.1 | 8.9 | 6.8 | 10.7 | 6 |
Note: TIPS, transjugular intrahepatic portosystemic shunt; CTP, Child-Turcotte-Pugh; MELD, the model for end-stage liver diseases; n/a, not available.
Results of meta-analyses
The forest plots of meta-analyses on the respective difference of predictive accuracy for MELD vs. CTP scores in 1-month, 3-month, 6-month, 12-month survival among patients after TIPS replacements are shown in Figure 2. Among five individual studies reporting 1-month survival, only one study [11] reported a negative value of SMD for MELD vs. CTP scores, and other four studies indicated MELD score were superior to CTP score. A positive results was observed in pooled analyses using a random effects model, but it did not reach to statistical significance (mean ES, 0.79; 95% CI, -0.24-1.83; P=0.13). Large statistical heterogeneity among these 5 included studies was observed (I2=99.1%; P<0.01). The funnel plot did not show evidence of publication bias (Kendall’s tau=0.60; P=0.23). In standardized deleted residuals analysis, the study by Angermayr et al. [11] was identified as an outlier (Standardized deleted residual=-5.35). After excluding this study [11], the predictive accuracy of MELD score was much better than CTP score (mean ES, 1.19; 95% CI, 0.84-1.53; P<0.01) with large heterogeneity (I2=86.5%; P<0.01).
Figure 2.
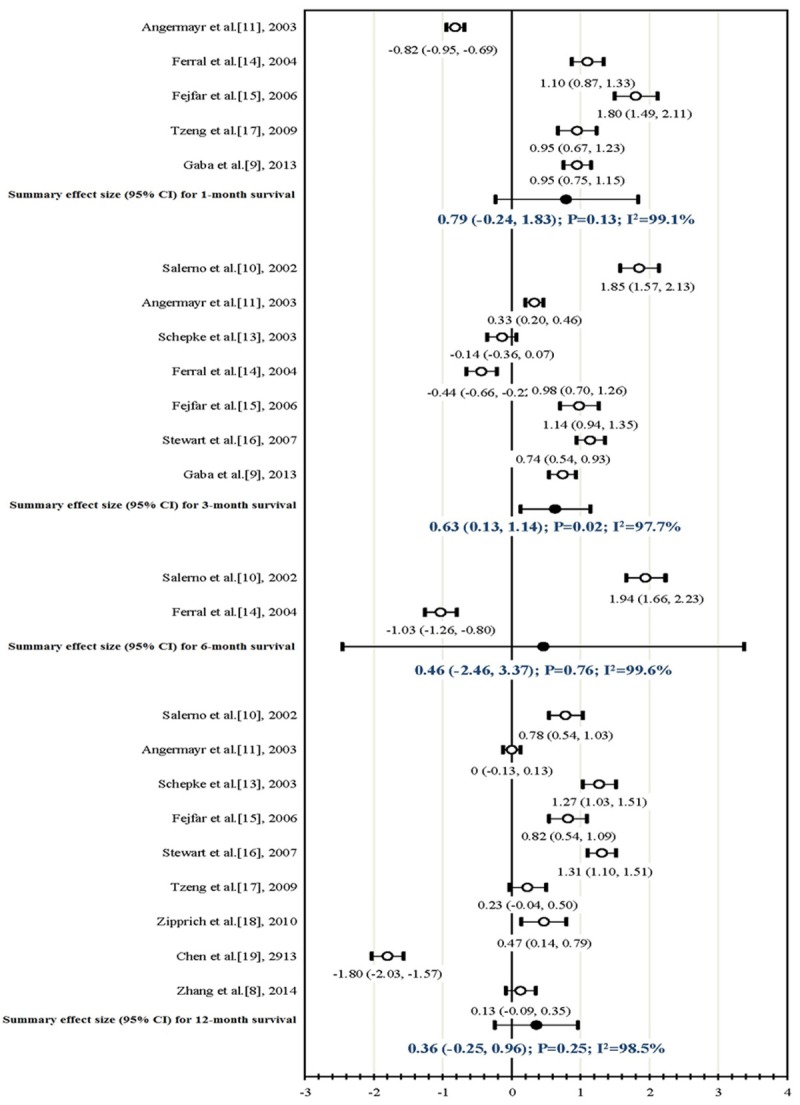
Forest plots of the comparison for the predictive accuracy of MELD and CTP scores in 1-month, 3-month, 6-month, and 12-month survival among patients underwent TIPS replacement.
Regarding 3-month survival, seven studies were used to perform a meta-analysis comparing the predictive capability of MELD and CTP scores [9-11,13-16]. Two studies observed a better predictive ability for CTP score [13,14] and other five [9-11,15,16] reported MELD outperformed. In the meta-analyses, a positive summary ES was shown (mean ES, 0.63; 95% CI, 0.13-1.14; P=0.01), and the I2 statistic indicated large statistical heterogeneity across the seven studies (I2=97.7%; P<0.01). No publication bias was found in the funnel plot (Kendall’s tau=0.24; P=0.56). One study [10] was identified as an outlier in standardized deleted residuals analysis (Standardized deleted residual=2.26). No significant difference was observed between MELD and CTP scores for predictive capability in survival among patients underwent TIPS after deleting this outlier study [10] (mean ES, 0.43; 95% CI, -0.03-0.89; P=0.06). Large heterogeneity still was obtained (I2=96.9%; P<0.01).
Only two studies [10,14] reported relevant c-statistics in 6-month survival and did not indicate a significant results after combination using meta-analyses (mean ES, 0.46; 95% CI, -2.46-3.37; P=0.76). Among nine studies included in meta-analysis for 12-month survival [8,10,11,13,15-19], one study reported CTP was better than MELD 19, and one showed zero [11]. The remaining seven studies addressed a positive value, but this difference was significant in five studies [10,13,15,16,18]. However, the difference was not significant in the random effects model of meta-analysis (mean ES, 0.36; 95% CI, -0.25-0.96; P=0.25), and there were strong indications of statistical heterogeneity across studies (I2=98.5%; P<0.01). No publication bias was obtained (Kendall’s tau=0.06; P=0.92). We found an outlier study [19] in standardized deleted residuals analysis (Standardized deleted residual=-3.96). MELD score was superior to CTP score in predicting 12-month survival using sensitivity analysis without this study [19] (mean ES, 0.63; 95% CI, 0.22-1.03; P<0.01), but large heterogeneity was observed (I2=96.2; P<0.01).
Discussion
To our knowledge, this is the first meta-analytic review summarizing eleven individual studies and evaluating the difference of predictive accuracy for both MELD and CTP scores in survival among 2037 patients undergoing TIPS replacement. Like previous systematic reviews [23,25,43,44], no confirmatory evidence is shown that MELD score is superior to CTP score in predicting overall survival based on current data, though MELD score is proved 63% better in predicting 3-month survival. However, these results were not stable in the sensitivity analyses. Few studies were observed for more than one-year survival after TIPS replacement. Further predictive capabilities of MELD and CTP for longer-time survival were needed.
Along with the rapid progress of modern medicine, TIPS were widely conducted for patients with liver diseases to improve the survival and quality of life during waiting for liver transplantation. Using prognostic models or scores to select patients for TIPS became more and more important when determining the most appropriate therapeutic option for patients. Compared with empirical CTP score, MELD score calculates a more objective value using laboratory tests to evaluate the severity of liver diseases. However, ascites and hepatic encephalopathy (HE) were not taken into account into MELD, but they are components of the CTP score [25,45]. The MELD score might underestimate the risk of death when patients had developed or would develop HE [23,44]. Hence, some researchers proposed that CTP was used for individual assessment of liver disease in daily clinical practice, and MELD was best in prioritizing candidates for liver transplantation [25]. Additionally, some studies have been reported better predictive capabilities of modified MELD, such as MELD-Na and Delta MELD [40,41,44,46,47]. Further predictive evaluation should be performed using systematic meta-analyses.
Most predictive models focus on survival after TIPS replacement as an outcome index, but other end-points might be also important, such as HE, ascites, stent dysfunction, and quality of life. In the light of the covered TIPS combined with variceal embolization, the survival has been increased significantly in recent years [48,49]. Predictive accuracy of MELD and CTP scores in other outcomes among patients is more valuable in further patient selection for TIPS, though MELD might be powerless to assess quality of life in liver transplant candidates [50]. Accurate MELD classification should be further explored using more individual studies [51].
Our analysis has specific strengths and limitations. Strengths include comprehensive comparison of predictive accuracy using meta-analyses. The c-statistic represents a global estimate of predicting an event, which is derived from area under the ROC curve, ranged from 0 to 1. When a c-statistic is more than 0.8 in a prediction model, the score has strong support to its accuracy [52]. On the other hand, our analyses are limited by the data provided by the individual studies. Firstly, depending on the results reported, 95% CIs of c-statistics had to be used for pooling, but which were not provided in some studies included in our meta-analyses [9,11,14-16,19]. Mean variance of the two scores from available studies was used if authors did not response after personal email contacts, which might lead to calculation bias. Secondly, despite the lack of indication of major publication bias in the formal evaluations employed, potential publication bias is impossible to be excluded completely. Thirdly, although four databases were searched and additive checks by cross-referencing were performed, we cannot promise to have missed a relevant study. Finally, large heterogeneity was observed across individual studies, which might be related to stent types and mean MELD and CTP scores before TIPS replacement. Available articles are still sparse further in-depth subgroup analyses and moderator evaluation should be considered when more relevant studies were reported.
Disclosure of conflict of interest
None.
References
- 1.Colombato L. The role of transjugular intrahepatic portosystemic shunt (TIPS) in the management of portal hypertension. J Clin Gastroenterol. 2007;41(Suppl 3):S344–351. doi: 10.1097/MCG.0b013e318157e500. [DOI] [PubMed] [Google Scholar]
- 2.Corbett C, Mangat K, Olliff S, Tripathi D. The role of Transjugular Intrahepatic Portosystemic Stent-Shunt (TIPSS) in the management of variceal hemorrhage. Liver Int. 2012;32:1493–1504. doi: 10.1111/j.1478-3231.2012.02861.x. [DOI] [PubMed] [Google Scholar]
- 3.Hausegger KA, Karnel F, Georgieva B, Tauss J, Portugaller H, Deutschmann H, Berghold A. Transjugular intrahepatic portosystemic shunt creation with the Viatorr expanded polytetrafluoroethylene-covered stent-graft. J Vasc Interv Radiol. 2004;15:239–248. doi: 10.1097/01.rvi.0000116194.44877.c1. [DOI] [PubMed] [Google Scholar]
- 4.Bai M, Qi XS, Yang ZP, Yang M, Fan DM, Han GH. TIPS improves liver transplantation-free survival in cirrhotic patients with refractory ascites: an updated meta-analysis. World J Gastroenterol. 2014;20:2704–2714. doi: 10.3748/wjg.v20.i10.2704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang Z, Han G, Wu Q, Ye X, Jin Z, Yin Z, Qi X, Bai M, Wu K, Fan D. Patency and clinical outcomes of transjugular intrahepatic portosystemic shunt with polytetrafluoroethylene-covered stents versus bare stents: a meta-analysis. J Gastroenterol Hepatol. 2010;25:1718–1725. doi: 10.1111/j.1440-1746.2010.06400.x. [DOI] [PubMed] [Google Scholar]
- 6.Tan HK, James PD, Sniderman KW, Wong F. Long-term clinical outcome of patients with cirrhosis and refractory ascites treated with transjugular intrahepatic portosystemic shunt insertion. J Gastroenterol Hepatol. 2015;30:389–395. doi: 10.1111/jgh.12725. [DOI] [PubMed] [Google Scholar]
- 7.ter Borg PC, Hollemans M, Van Buuren HR, Vleggaar FP, Groeneweg M, Hop WC, Laméris JS. Transjugular intrahepatic portosystemic shunts: long-term patency and clinical results in a patient cohort observed for 3-9 years. Radiology. 2004;231:537–545. doi: 10.1148/radiol.2312021797. [DOI] [PubMed] [Google Scholar]
- 8.Zhang F, Zhuge Y, Zou X, Zhang M, Peng C, Li Z, Wang T. Different scoring systems in predicting survival in Chinese patients with liver cirrhosis undergoing transjugular intrahepatic portosystemic shunt. Eur J Gastroenterol Hepatol. 2014;26:853–860. doi: 10.1097/MEG.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 9.Gaba RC, Couture PM, Bui JT, Knuttinen MG, Walzer NM, Kallwitz ER, Berkes JL, Cotler SJ. Prognostic capability of different liver disease scoring systems for prediction of early mortality after transjugular intrahepatic portosystemic shunt creation. J Vasc Interv Radiol. 2013;24:411–420. 420.e411–414. doi: 10.1016/j.jvir.2012.10.026. quiz 421. [DOI] [PubMed] [Google Scholar]
- 10.Salerno F, Merli M, Cazzaniga M, Valeriano V, Rossi P, Lovaria A, Meregaglia D, Nicolini A, Lubatti L, Riggio O. MELD score is better than Child-Pugh score in predicting 3-month survival of patients undergoing transjugular intrahepatic portosystemic shunt. J Hepatol. 2002;36:494–500. doi: 10.1016/s0168-8278(01)00309-9. [DOI] [PubMed] [Google Scholar]
- 11.Angermayr B, Cejna M, Karnel F, Gschwantler M, Koenig F, Pidlich J, Mendel H, Pichler L, Wichlas M, Kreil A, Schmid M, Ferlitsch A, Lipinski E, Brunner H, Lammer J, Ferenci P, Gangl A, Peck-Radosavljevic M. Child-Pugh versus MELD score in predicting survival in patients undergoing transjugular intrahepatic portosystemic shunt. Gut. 2003;52:879–885. doi: 10.1136/gut.52.6.879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee DH, Son JH, Kim TW. New scoring systems for severity outcome of liver cirrhosis and hepatocellular carcinoma: current issues concerning the Child-Turcotte-Pugh score and the Model of End-Stage Liver Disease (MELD) score. Taehan Kan Hakhoe Chi. 2003;9:167–179. [PubMed] [Google Scholar]
- 13.Schepke M, Roth F, Fimmers R, Brensing KA, Sudhop T, Schild HH, Sauerbruch T. Comparison of MELD, Child-Pugh, and Emory model for the prediction of survival in patients undergoing transjugular intrahepatic portosystemic shunting. Am J Gastroenterol. 2003;98:1167–1174. doi: 10.1111/j.1572-0241.2003.07515.x. [DOI] [PubMed] [Google Scholar]
- 14.Ferral H, Gamboa P, Postoak DW, Albernaz VS, Young CR, Speeg KV, McMahan CA. Survival after elective transjugular intrahepatic portosystemic shunt creation: prediction with model for end-stage liver disease score. Radiology. 2004;231:231–236. doi: 10.1148/radiol.2311030967. [DOI] [PubMed] [Google Scholar]
- 15.Fejfar T, Safka V, Hůlek P, Vanásek T, Krajina A, Jirkovský V. MELD score in prediction of early mortality in patients suffering refractory ascites treated by TIPS. Vnitr Lek. 2006;52:771–776. [PubMed] [Google Scholar]
- 16.Stewart CA, Malinchoc M, Kim WR, Kamath PS. Hepatic encephalopathy as a predictor of survival in patients with end-stage liver disease. Liver Transpl. 2007;13:1366–1371. doi: 10.1002/lt.21129. [DOI] [PubMed] [Google Scholar]
- 17.Tzeng WS, Wu RH, Lin CY, Chen JJ, Sheu MJ, Koay LB, Lee C. Prediction of mortality after emergent transjugular intrahepatic portosystemic shunt placement: use of APACHE II, Child-Pugh and MELD scores in Asian patients with refractory variceal hemorrhage. Korean J Radiol. 2009;10:481–489. doi: 10.3348/kjr.2009.10.5.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zipprich A, Kuss O, Rogowski S, Kleber G, Lotterer E, Seufferlein T, Fleig WE, Dollinger MM. Incorporating indocyanin green clearance into the Model for End Stage Liver Disease (MELD-ICG) improves prognostic accuracy in intermediate to advanced cirrhosis. Gut. 2010;59:963–968. doi: 10.1136/gut.2010.208595. [DOI] [PubMed] [Google Scholar]
- 19.Chen H, Bai M, Qi X, Liu L, He C, Yin Z, Fan D, Han G. Child-Na score: a predictive model for survival in cirrhotic patients with symptomatic portal hypertension treated with TIPS. PLoS One. 2013;8:e79637. doi: 10.1371/journal.pone.0079637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Child C, Turcotte J. The liver and portal hypertension. In: Child CI, editor. Surgery and Portal Hypertension. [Google Scholar]
- 21.Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646–649. doi: 10.1002/bjs.1800600817. [DOI] [PubMed] [Google Scholar]
- 22.Cejna M. Child-PUGH-vs. meld-score to predict survival after tips: the Vienna-experience with 349 patients over 10 years. J Hepatol. 2002;36:16. [Google Scholar]
- 23.Durand F, Valla D. Assessment of the prognosis of cirrhosis: Child-Pugh versus MELD. J Hepatol. 2005;42:S100–S107. doi: 10.1016/j.jhep.2004.11.015. [DOI] [PubMed] [Google Scholar]
- 24.Saad WE, Wagner CC, Al-Osaimi A, Bliebel W, Lippert A, Davies MG, Sabri SS, Turba UC, Matsumoto AH, Angle JF, Caldwell S. The Effect of Balloon-Occluded Transvenous Obliteration of Gastric Varices and Gastrorenal Shunts on the Hepatic Synthetic Function: A Comparison Between Child-Pugh and Model for End-Stage Liver Disease Scores. Vasc Endovasc Surg. 2013;47:281–287. doi: 10.1177/1538574413485646. [DOI] [PubMed] [Google Scholar]
- 25.Cholongitas E, Papatheodoridis GV, Vangeli M, Terreni N, Patch D, Burroughs AK. Systematic review: The model for end-stage liver disease--should it replace Child-Pugh’s classification for assessing prognosis in cirrhosis? Aliment Pharmacol Ther. 2005;22:1079–1089. doi: 10.1111/j.1365-2036.2005.02691.x. [DOI] [PubMed] [Google Scholar]
- 26.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1–34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 27.Montgomery A, Ferral H, Vasan R, Postoak DW. MELD score as a predictor of early death in patients undergoing elective transjugular intrahepatic portosystemic shunt (TIPS) procedures. Cardiovasc Intervent Radiol. 2005;28:307–312. doi: 10.1007/s00270-004-0145-y. [DOI] [PubMed] [Google Scholar]
- 28.Yoon CJ, Chung JW, Park JH. Transjugular intrahepatic portosystemic shunt for acute variceal bleeding in patients with viral liver cirrhosis: predictors of early mortality. AJR Am J Roentgenol. 2005;185:885–889. doi: 10.2214/AJR.04.0607. [DOI] [PubMed] [Google Scholar]
- 29.Higgins J, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1. 0 [updated March 2011] The Cochrane Collaboration. 2011. Available from: www.cochrane-handbook.org.
- 30.Normand SL. Meta-analysis: formulating, evaluating, combining, and reporting. Stat Med. 1999;18:321–359. doi: 10.1002/(sici)1097-0258(19990215)18:3<321::aid-sim28>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 31.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 32.Lipsey M, Wilson D. Practical meta-analysis. Thousand Oaks, CA: Sage; 2001. [Google Scholar]
- 33.Rothstein HR, Sutton AJ, Borenstein M. Publication Bias in Meta-Analysis: Prevention, Assessment and Adjustments. Chichester, England: Wiley; 2005. [Google Scholar]
- 34. The R Project for Statistical Computing, https://www.r-project.org/
- 35.Schepke M, Roth F, Brensing KA, Sudhop T, Sauerbruch T. Meld-score compared to the Child-Pugh and the Emory-score for the prediction of long-term survival in patients undergoing transjugular intrahepatic portosystemic shunting (TIPS) Hepatology. 2001;34:183A–183A. doi: 10.1111/j.1572-0241.2003.07515.x. [DOI] [PubMed] [Google Scholar]
- 36.Angermayr B. Predicting short-term survival after TIPS: MELD vs. Child-Pugh score (CPS) Gastroenterology. 2002:122, A655–A655. [Google Scholar]
- 37.Angermayr B. Creatinine-modified Child-Pugh Score (CPSC) compared with meld-score to predict survival in patients undergoing tips. Hepatology. 2002;36:378A–378A. [Google Scholar]
- 38.Gaba RC, Couture PM, Bui JT, Knuttinen MG, Walzer NM, Kallwitz ER, Berkes JL, Cotler SJ. Prognostic capability of different liver disease scoring systems for prediction of early mortality after TIPS. J Vasc Interv Radiol. 2013;24:411–20. doi: 10.1016/j.jvir.2012.10.026. [DOI] [PubMed] [Google Scholar]
- 39.Gaba RC, Shah KD, Couture PM, Parvinian A, Minocha J, Knuttinen MG, Bui JT. Within-patient temporal variance in MELD score and impact on survival prediction after TIPS creation. Ann Hepatol. 2013;12:797–802. [PubMed] [Google Scholar]
- 40.Luca A, Angermayr B, Bertolini G, Koenig F, Vizzini G, Ploner M, Peck-Radosavljevic M, Gridelli B, Bosch J. An integrated MELD model including serum sodium and age improves the prediction of early mortality in patients with cirrhosis. Liver Transpl. 2007;13:1174–1180. doi: 10.1002/lt.21197. [DOI] [PubMed] [Google Scholar]
- 41.Guy J, Somsouk M, Shiboski S, Kerlan R, Inadomi JM, Biggins SW. New Model for End Stage Liver Disease Improves Prognostic Capability After Transjugular Intrahepatic Portosystemic Shunt. Clin Gastroenterol Hepatol. 2009;7:1236–1240. doi: 10.1016/j.cgh.2009.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Parvinian A, Bui JT, Knuttinen MG, Minocha J, Gaba RC. Right atrial pressure may impact early survival of patients undergoing transjugular intrahepatic portosystemic shunt creation. Ann Hepatol. 2014;13:411–419. [PubMed] [Google Scholar]
- 43.Al Sibae MR, Cappell MS. Accuracy of MELD scores in predicting mortality in decompensated cirrhosis from variceal bleeding, hepatorenal syndrome, alcoholic hepatitis, or acute liver failure as well as mortality after non-transplant surgery or TIPS. Dig Dis Sci. 2011;56:977–987. doi: 10.1007/s10620-010-1390-3. [DOI] [PubMed] [Google Scholar]
- 44.Kim HJ, Lee HW. Important predictor of mortality in patients with end-stage liver disease. Clin Mol Hepatol. 2013;19:105–115. doi: 10.3350/cmh.2013.19.2.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wiesner RH, McDiarmid SV, Kamath PS, Edwards EB, Malinchoc M, Kremers WK, Krom RA, Kim WR. MELD and PELD: application of survival models to liver allocation. Liver Transpl. 2001;7:567–580. doi: 10.1053/jlts.2001.25879. [DOI] [PubMed] [Google Scholar]
- 46.Kamath PS, Kim WR. Is the change in MELD score a better indicator of mortality than baseline MELD score? Liver Transpl. 2003;9:19–21. doi: 10.1053/jlts.2003.50031. [DOI] [PubMed] [Google Scholar]
- 47.Ruf AE, Kremers WK, Chavez LL, Descalzi VI, Podesta LG, Villamil FG. Addition of serum sodium into the MELD score predicts waiting list mortality better than MELD alone. Liver Transpl. 2005;11:336–343. doi: 10.1002/lt.20329. [DOI] [PubMed] [Google Scholar]
- 48.Wu Q, Jiang J, He Y, Jiang T, Zhou S. Transjugular intrahepatic portosystemic shunt using the FLUENCY expanded polytetrafluoroethylene-covered stent. Exp Ther Med. 2013;5:263–266. doi: 10.3892/etm.2012.776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Qi X, Liu L, Bai M, Chen H, Wang J, Yang Z, Han G, Fan D. Transjugular intrahepatic portosystemic shunt in combination with or without variceal embolization for the prevention of variceal rebleeding: a meta-analysis. J Gastroenterol Hepatol. 2014;29:688–696. doi: 10.1111/jgh.12391. [DOI] [PubMed] [Google Scholar]
- 50.Saab S, Ibrahim AB, Shpaner A, Younossi ZM, Lee C, Durazo F, Han S, Esrason K, Wu V, Hiatt J, Farmer DG, Ghobrial RM, Holt C, Yersiz H, Goldstein LI, Tong MJ, Busuttil RW. MELD fails to measure quality of life in liver transplant candidates. Liver Transpl. 2005;11:218–223. doi: 10.1002/lt.20345. [DOI] [PubMed] [Google Scholar]
- 51.Rodrigue JR, Nelson DR, Reed AI, Hanto DW, Curry MP. Is Model for End-Stage Liver Disease score associated with quality of life after liver transplantation? Prog Transplant. 2011;21:207–214. doi: 10.1177/152692481102100305. [DOI] [PubMed] [Google Scholar]
- 52.Kamath PS, Kim WR. The model for end-stage liver disease (MELD) Hepatology. 2007;45:797–805. doi: 10.1002/hep.21563. [DOI] [PubMed] [Google Scholar]


