Abstract
The aim of this study is to determine whether the creative arts program (HA) is effective in preventing the onset of Posttraumatic stress disorder (PTSD). PTSD develops in 10-20% of motor vehicle accident survivors (MVAs). MVAs in the initial months after the accident were randomly assigned to receive 8-week HA intervention (n = 26) or wait the list (WL, n = 26). The arts program consisted of writing and drawing. PTSD severity was assessed at 2, 6, and 12 months post injury with a clinical interview (Clinician-Administered PTSD Scale, CAPS) and self-report instrument (Impact of Event Scale-Revised, IES-R). Secondary outcomes were post-traumatic growth (PTG), depression and anxiety symptoms. Repeated measures analysis of variance indicated that both HA and WL group exhibited a significant effect of time (P < 0.01) on CAPS, but no significant group differences over time. There were no group differences on depression or anxiety over time. Pessimists did not benefit more from attending the HA than they did from attending the WL. Our results fail to support the hypothesis that the creative arts program is effect in avoiding MVA-related PTSD symptoms. But it only seems to be a short-term, rather than a long-term effect.
Keywords: Art therapy, life orientation, motor vehicle accidents, posttraumatic stress disorder
Introduction
According to the report from the Division of Public Health Supervision in the Ministry of Health in China, there are almost 100,000 death casualties, and 500,000 injured cases in motor vehicle accidents (MVA) every year in China. Surviving an accident and subsequent hospitalization may leave a person prone to experiencing anxiety, depressive disorders, and posttraumatic stress disorder (PTSD) [1-3]. Full recovery from injury may be hampered by both physical ailments and psychological distress. Reported prevalence of PTSD after MVA ranged from 8.5% to 23.1% [3]. Research has shown that MVAs are the leading cause of PTSD in Western society [4], but much less attention has been given to its presentation, prevention and prevalence in China, particularly among MVAs to date.
PTSD is a psychiatric syndrome that can progress after exposure to a traumatic event-either immediately or even long after the original event. The MVA survivors with PTSD had lower scores in personal strength than MVA survivors without PTSD [5]. Characterized by the frequent re-experiencing of the traumatic event, it is accompanied by all kinds of dysphoric, cognitive and autonomic symptoms [6]. The symptoms of PTSD regularly appear with a long latency, from 15 to 30 years after the traumatic events [7]. Even though some children and adolescents appear to be unaffected or only slightly affected by such events, more others suffer severe acute or long-term psychological consequences [8]. In consequence, the need to prevent or reduce psychological harm is critical.
Traditional psychotherapy treatment for PTSD patients involves encouraging the patient to “talk through” the problem. However, it will become quite difficult for a patient with aphasia, while art therapy has a unique contribution in this situation [9,10]. Art therapy (HA) is a form of psychotherapy that has been practiced for over 60 years, aiding people who may find it difficult to express themselves verbally to engage in psychological treatment [11]. It allows the trauma to “speak” in its own language-the visual form and creates a situation in which survivors feel free to display the horrors they have experienced among various age groups. During the last decade, increasing attention has been focused on whether art therapy can result in beneficial or constructive consequences [12].
In a randomized controlled trial, Sloan and associates confirmed that participants assigned to written exposure therapy showed significant reductions in MVA-related PTSD symptom severity at 6- and 18- week post-baseline, relative to a waitlist (WL) participants, with large between-group effect sizes [13]. Research showed that HA could help the patients cope with PTSD, who survived Nazi concentration camps [14]. Beside, art program may foster positive growth and spirituality after traumatic life experiences in cancer outpatients [15].
The study examined the efficacy of HA as an intervention for individuals to prevent the onset of MVA-related PTSD and to test the stability of the improvements 6 months, and 12 months after MVA. We expected that participants who were randomly assigned to HA would show clinically significant improvements in PTSD symptom severity. Because of the brevity of treatment, we expected a low treatment dropout rate associated with HA.
Materials and methods
Study procedures
The local institutional review boards provided medical ethical approval. Patients were contacted in hospital within 96 hours post injury to assess eligibility. Recruitment occurred between February 2012 and January 2013. Treatment and 12-month follow-ups on all participants were completed in November 2014. After the patients have been recruited and completed the initial assessment, they were randomly allocated to one of two conditions: ① the creative arts (HA) intervention or ② a waitlist (WL) comparison condition. Patients were asked not to share information to the assessors, to ensure that they were blind to interventions. Follow-up assessments were carried out at three time points, at 2 months (T1), 6 months (T2), and 12 months (T3) after completion of the invention. The assessments took place in the hospital, or at the private home of the patient. Advanced postgraduate students in Clinical Psychology conducted all assessments after extensive training. Participants also filled out a set of questionnaires at home.
Participants
Survivors of severe MVAs were selected consecutively from the emergency department of the first affiliated hospital of Zhengzhou university, China. These patients were suspected to suffer from possible severe injuries that required specialized acute medical care. Eligible participants had to be 18-65 years older, and be able to communicate in verbal and written Chinese. Exclusion criteria were a history of neurological problems, brain surgery, brain damage, and spinal cord injuries. Besides, we excluded participants with current alcohol and/or drug abuse and current or past schizophrenic or psychotic disorders. After completion of the diagnostic interview, 52 MVA survivors finally qualified. Due to incomplete data, 6 were excluded from the data analysis. The final sample consisted of 46 MVA survivors.
Intervention: the creative arts therapy (HA)
The aim of the intervention was to provide MVAs with opportunities for self-discovery and empowerment through the creative process. The intervention consisted of 8 weekly sessions of 40 minutes in small groups of 4-6 participants in hospital led by a psychologically trained and supervised artist. The primary modalities utilized were creative writing and drawing. The theme of the first 2 weeks was “Who am I?” which involved self-exploration, and participants were requested to perform simple drawing techniques. The aim of this first phase of the program was to make people feel comfortable with the group situation and with creative working. “How am I?” was the theme for weeks 3 to 5, an exploration into present emotions and issues. Finally, the last themes focused on the question “How can I heal?”, bringing together resources moving forward. Participants will gradually start expressing their feelings, for example, by drawing their mood and by painting a self-portrait.
Outcomes
The Clinician-Administered PTSD Scale (CAPS), as defined by the DSM-IV, was used to evaluate PTSD symptom severity [16]. CAPS assess the 17 core symptoms of PTSD along with five associated features. CAPS rate the frequency and intensity of each symptom, the impact, the overall severity, and the global validity of ratings. The total score for the CAPS PTSD ratings ranges from 0 to 136 with higher scores indicating greater severity of PTSD.
We assessed self-reported PTSD severity with the Impact of Event Scale-Revised (IES-R). Three core symptoms of PTSD, namely, re-experiencing, avoidance, and hyperarousal, are measured. IES-R includes 22 items on a 5-point scale (ranging from 0 to 88). The Chinese translation of the IES-R has been demonstrated to have satisfactory reliability and validity [17].
The Hospital Anxiety and Depression Scale (HADS) was used to measure levels of anxiety and depression. The scale consists of 14 items and two subscales (anxiety and depression) with seven items in each subscale. A score of 8 or above on either the anxiety or depression subscale is indicative of clinically relevant symptoms [18].
The Posttraumatic Growth Inventory (PTGI) includes the following subscales: personal strength; spiritual change; relating to others; appreciation of life; and new possibilities. The inventory evaluates positive outcomes of traumatic events on a six-point Likert scale [19].
The Life Orientation Test-Revised (LOT-R) is a revision of the original Life Orientation Test, established to assess individual optimism/pessimism, which has been confirmed in China with high reliability [20]. The instrument contains 10 items and each item is rated on a 5-point scale. Total LOT-R scores below the median score of 18 are used to define pessimists, whereas LOT-R scores of 18 or higher belong to optimists.
Statistical analysis
Descriptive data were evaluated for normalcy and demographic variables summarized as means and medians, with standard deviations and ranges. Baseline T0 data were compared between HA and WL samples on demographics as well as time 1 psychological data to test for initial equivalency of groups using independent-samples t tests or chi-squared test squared analysis. Associations between continuous variables were analyzed using Pearson correlation coefficient.
We compared the course of the 2 groups at all time points between T0 and T3 using general linear models with repeated measures analysis of variance (ANOVA), to distinguish between intrasubject effects (time effect and time-by-group interaction) and intersubject effects. To evaluate the effect size (partial η 2 score) of the results, the commonly used guidelines (0.01 = small, 0.06 = moderate, and 0.14 = large) were used. Because multiple comparisons were performed, a Bonferroni adjustment was applied to the α values for the final results. All data analyses were conducted using the Statistical Package for the Social Sciences (SPSS) version 16.0.
Results
Sample characteristics
Recruitment outcomes and study participation are depicted in CONSORT flow diagram (Figure 1). In order to assure adequacy of randomization, we compared group differences on demographics and CAPS at baseline; no substantial group difference was observed. Moreover, t-tests (age) and chi-square analyses (gender, education level) indicated no significant demographic differences between the two groups, as shown in Table 1.
Figure 1.
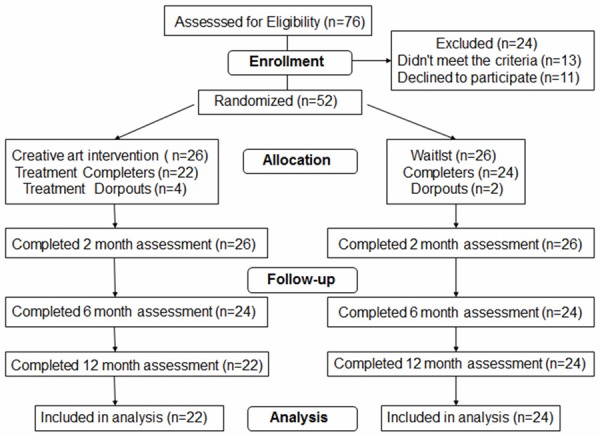
Flowchart over the selection procedure and the data collection procedure for the intervention group and the control group.
Table 1.
Participant characteristics at baseline
| Characteristic | HA | WL | P |
|---|---|---|---|
|
| |||
| n = 22 | n = 24 | ||
| Age, mean (SD) | 39.34 (14.57) | 41.23 (15.24) | 0.46 |
| Sex (female), n (%) | 13 (59.1) | 14 (58.33) | 0.67 |
| College education, n (%) | 7 (31.81) | 8 (33.33) | 0.82 |
| Jobless, n (%) | 6 (27.27) | 8 (33.33) | 0.25 |
| Married, n (%) | 12 (54.55) | 12 (50.00) | 0.26 |
| Prior traumatic events, mean (SD) | 2.87 (2.31) | 2.57 (2.18) | 0.76 |
| Hospital admission, n (%) | 18 (81.82) | 19 (79.17) | 0.54 |
| Days hospitalization, mean (SD) | 4.25 (7.36) | 4.57 (7.52) | 0.34 |
| ICU admission, n (%) | 3 (13.64) | 3 (12.50) | 0.87 |
| Trauma Severity, mean (SD) | 10.56 (8.61) | 10.38 (9.74) | 0.45 |
| Glasgow Coma Scale, mean (SD) | 14.59 (1.81) | 14.78 (1.94) | 0.12 |
Main outcomes
Table 2 shows the results of analyses for PTSD, PTGI, and HADS. Analysis of CAPS indicated a noteworthy effect of time (P < 0.05), but no significant group differences over time (12-month follow-up, HA group: estimated means 20.91; WL group: estimated means 22.21, P = 0.74). On the analysis of IES-R, we observed a similar significant time effect (P < 0.01) and no group differences over time (12-month, HA group: means 8.95; WL group: means 11.10, P = 0.68). Figure 2 displayed CAPS and IES-R means over time.
Table 2.
Comparison of mean scores between HA (n = 22) and WL (n = 24), and the effect size of the results
| Time | Effect | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||||||
| Outcome | T0 | T1 | T2 | T3 | Group | Time | Group × Time | ||||||
|
| |||||||||||||
| Mean | Mean | Mean | Mean | F | P | η 2 | F | P | η 2 | F | P | η 2 | |
| CAPS | 1.6 | 0.23 | 0.05 | 6.4 | 0.01 | 0.07 | 0.58 | 0.74 | 0.06 | ||||
| HA | 45.59 | 33.10 | 27.73 | 20.91 | |||||||||
| WL | 47.79 | 44.29 | 38.13 | 22.21 | |||||||||
| IES-R | 2.8 | 0.25 | 0.05 | 14.6 | 0.01 | 0.08 | 1.2 | 0.68 | 0.04 | ||||
| HA | 22.80 | 16.21 | 11.42 | 8.95 | |||||||||
| WL | 23.90 | 22.51 | 15.71 | 11.10 | |||||||||
| PTGI | 1.8 | 0.17 | 0.01 | 55.4 | 0.01 | 0.08 | 3.2 | 0.02 | 0.09 | ||||
| HA | 55.08 | 57.09 | 63.14 | 65.73 | |||||||||
| WL | 54.63 | 56.04 | 58.29 | 63.95 | |||||||||
| Anxiety | 0.87 | 0.11 | 0.05 | 2.3 | 0.08 | 0.06 | 0.94 | 0.36 | 0.03 | ||||
| HA | 4.62 | 4.00 | 3.90 | 4.10 | |||||||||
| WL | 4.65 | 4.45 | 4.41 | 3.85 | |||||||||
| Depression | 1.2 | 0.58 | 0.04 | 3.1 | 0.05 | 0.01 | 1.1 | 0.64 | 0.02 | ||||
| HA | 3.60 | 3.53 | 4.10 | 3.29 | |||||||||
| WL | 4.10 | 3.91 | 4.62 | 3.15 | |||||||||
Abbreviations: HA, creative art therapy intervention; WL, wait list condition.
Figure 2.
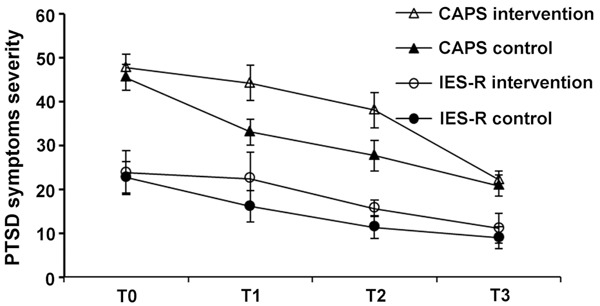
Trends in observed PTSD symptom severity (CAPS and IES-R) per intervention group.
Secondary outcomes
No significant differences were found in posttraumatic growth scores at baseline between HA and WL participants. As described in Table 2, significant changes were observed in PTGI scores for HA group over time. There was a main effect of time (F = 55.4, P = 0.01) and a significant group-by-time interaction (F = 3.2, P = 0.02). Nonetheless, after adjusting for the baseline PTGI score by setting it as a covariate, no main effect of group was found (Table 2). Repetition of the analyses using LOT-R scores as covariates generated similar results. The effect sizes of these results were moderate (Table 2). For depressive and anxiety symptoms, no effects of time or group over time was obtained in mixed-model analyses (12 month HADS-A, HA group: means 4.10; WL group: means 3.85, P > 0.05; 12 month HADS-D, HA group: means 3.29; WL group: means 3.15, P > 0.05).
Comparisons of the outcome mean scores for MVAs with pessimistic and optimistic life orientations in the 2 groups are shown in Table 3. At 2 months, optimists in the HA scored dramatically lower on IES-R than did optimists in the WL (P < 0.01). Pessimists in the HA scored considerably higher on PTGI at 6 months than did pessimists in the WL (P < 0.01). However, at 12 months, no significant differences were found.
Table 3.
Comparison of Pessimists and Optimists
| Optimists | Pessimists | ||||
|---|---|---|---|---|---|
|
|
|||||
| HA (n = 22) | WL (n = 24) | HA (n = 22) | WL (n = 24) | ||
| T0 | CAPS PTSD | 43.5 | 44.8 | 47.3 | 49.8 |
| IES-R PTSD | 20.2 | 20.2 | 25.0 | 27.0 | |
| Anxiety | 58.2 | 57.9 | 52.5 | 51.9 | |
| Depression | 4.1 | 4.0 | 5.1 | 5.2 | |
| PTGI | 3.3 | 3.5 | 3.9 | 4.6 | |
| T1 | CAPS PTSD | 25.3 | 29.4a | 39.6 | 56.9 |
| IES-R PTSD | 14.8 | 19.9a | 17.3 | 24.7 | |
| Anxiety | 59.1 | 58.6 | 55.4 | 53.8 | |
| Depression | 3.9 | 4.1 | 4.1 | 4.7 | |
| PTGI | 3.3 | 3.8 | 3.7 | 4.0 | |
| T2 | CAPS PTSD | 25.7 | 28.5 | 29.4 | 46.3 |
| IES-R PTSD | 11.3 | 14.8 | 11.5 | 16.5 | |
| Anxiety | 66.4 | 62.4 | 60.4 | 54.8a | |
| Depression | 3.7 | 4.1 | 4.1 | 4.7 | |
| PTGI | 3.9 | 4.3 | 4.3 | 4.9 | |
| T3 | CAPS PTSD | 18.6 | 20.2 | 22.8 | 23.9 |
| IES-R PTSD | 7.9 | 9.5 | 9.8 | 12.4 | |
| Anxiety | 66.4 | 64.5 | 65.2 | 63.5 | |
| Depression | 3.8 | 3.7 | 4.4 | 4.0 | |
| PTGI | 3.2 | 3.1 | 3.4 | 3.2 | |
Abbreviations: HA, creative art therapy intervention; WL, wait list condition.
Significance was set at P < 0.05.
Discussion
The need is great for dissemination of effective treatment approaches for MVA survivors. Such exposures are common in China and around the world. Inappropriate therapy can lead to their exacerbation. Proponents of art therapy claim that trauma is stored in memory as an image; and expressive art techniques are effective for resolving it. A randomized study by Berger et al. supported that assumption, and demonstrated that HA is effective in preventing PTSD [21]. However, evidence is still sparse and there was inconsistent evidence about the effectiveness of the art therapy. For example, weekly group sessions with art therapy failed to exhibited an effect on post-traumatic growth in patients with cancer [22].
The aim of this trial was to testify the potential effects of HA on reducing PTSD, depression, and anxiety in patients. In line with previous research, depression was the most important variable to predict PTSD [23]. Based on our results, there was no evidence of an effect of HA on PTSD. Moreover, there were no differences between groups with respect to the severity of depression and anxiety at 12 months. Art therapy was not more useful for pessimistic MVAs than optimistic MVAs. Several explanations for this finding are possible.
Firstly, the therapeutic dose (8 weekly sessions, each of 40 minutes in drawing and writing) may not have been sufficient to produce beneficial outcome. The findings about the therapeutic dose have been varied in the literature. According to Sheila’s research, art program which consists of six weekly sessions, each of 2-h duration, for a total of 12 h of contact time, may improve positive growth after traumatic life experiences. However, the intervention which consisted of 22 weekly sessions of 90 minutes in small groups failed to exhibit an effect on PTSD reported by Susanne [22]. More changes are needed for the treatment protocol in future pilot work.
Secondly, the sample size was small and the focus group was restricted to only one institution so results may not be generalizable. In addition, inclusion of participants with mild baseline PTSD symptoms may have been tricky in relation to other results of the studies. Foa and Meadows elucidate that the inclusion of such participants can result in the therapy effects being minimized as it can be difficult to detect enhancements following treatment [10].
Another explanation for not obtaining a substantial effect of the intervention may be the low PTSD symptom level. The average IES-R is 16.2 at 2 month, which declined to 8.9 at 12 months. This unpredictably low PTSD prevalence left little room for symptom enhancement for the whole group. As a clinical implication of our study, future art-based interventions should be designed with high initial symptoms. These individuals may be precisely identified within the first week following trauma with early screening tools for PTSD [24,25].
Thirdly, our program failed to use a manual to guide the whole process of the intervention. The lack of a manual is problematic in two respects. On one hand, it does not offer guarantee that the therapy was delivered in the same manner to all of the participants. On another hand, it does not permit the research to be duplicated.
Finally, it is possible that the idea of art therapy did not match the acute needs of the injury survivors, giving rise to the drop-out of some patients. Some participants in this study may not be treatment seeking. Previous studies exploring needs of victims after the September 11, 2001, terrorist attacks revealed that only very few people (< 1%) conveyed a need for specialized mental health support in the acute post-trauma phase, and most (71-87%) turned to loved ones or others for support [26,27].
In conclusion, this is the first Chinese RCT utilizing art therapy program for MVA survivors with PTSD. Our conclusion at this point must be that there is no evidence for an effect of weekly art intervention on PTSD in MVA patients. To some extent, PTSD, depression and anxiety symptoms are attenuated after the intervention, but it seems to be a short-term effect, rather than a long-term effect.
Acknowledgements
This study was granted by the national key clinical specialist construction project, Emergency professional (2012649), the national key clinical specialist construction project, specific nursing (2011872) and the basic and advanced technology research projects of Henan Province (142300410068).
Disclosure of conflict of interest
None.
References
- 1.Barskova T, Oesterreich R. Post-traumatic growth in people living with a serious medical condition and its relations to physical and mental health: a systematic review. Disabil and Rehabil. 2009;31:1709–1733. doi: 10.1080/09638280902738441. [DOI] [PubMed] [Google Scholar]
- 2.Sun J, Zhang H, Guan L, Zhou H, Sun M. Alpha-lipolic acid attenuates trinitrobenzene sulfonic acid-induced ulcerative colitis in mice. Int J Clin Exp Med. 2015;8:358–367. [PMC free article] [PubMed] [Google Scholar]
- 3.Yasan A, Guzel A, Tamam Y, Ozkan M. Predictive factors for acute stress disorder and posttraumatic stress disorder after motor vehicle accidents. Psychopathology. 2009;42:236–241. doi: 10.1159/000218521. [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 5.Zoellner T, Rabe S, Karl A, Maercker A. Posttraumatic growth in accident survivors: openness and optimism as predictors of its constructive or illusory sides. J Clin Psychol. 2008;64:245–263. doi: 10.1002/jclp.20441. [DOI] [PubMed] [Google Scholar]
- 6.Berthold SM, Kong S, Mollica RF, Kuoch T, Scully M, Franke T. Comorbid Mental and Physical Health and Health Access in Cambodian Refugees in the US. J Community Health. 2014;39:1045–1052. doi: 10.1007/s10900-014-9861-7. [DOI] [PubMed] [Google Scholar]
- 7.Arlien-Soborg P, Simonsen L. Cerebral dysfunction occurring after years of latency. Ugeskrift for Laeger. 1999;161:578–581. [PubMed] [Google Scholar]
- 8.Ralevski E, Olivera-Figueroa LA, Petrakis I. PTSD and comorbid AUD: a review of pharmacological and alternative treatment options. Subst Abuse Rehabil. 2014;5:25–36. doi: 10.2147/SAR.S37399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Avrahami D. Visual art therapy’s unique contribution in the treatment of post-traumatic stress disorders. J Trauma Dissociation. 2005;6:5–38. doi: 10.1300/j229v06n04_02. [DOI] [PubMed] [Google Scholar]
- 10.Rolfsnes ES, dsoe T. School-based intervention programs for PTSD symptoms: a review and meta-analysis. J Trauma Stress. 2011;24:155–165. doi: 10.1002/jts.20622. [DOI] [PubMed] [Google Scholar]
- 11.Crawford MJ, Killaspy H, Barnes TR, Barrett B, Barrett B, Byford S, Clayton K, Dinsmore J. Group art therapy as an adjunctive treatment for people with schizophrenia: a randomised controlled trial (MATISSE) Health Technol Assess. 2012;16:iii–iv. 1–76. doi: 10.3310/hta16080. [DOI] [PubMed] [Google Scholar]
- 12.Crawford MJ, Patterson S. Arts therapies for people with schizophrenia: an emerging evidence base. Evid Based Ment Health. 2007;10:69–70. doi: 10.1136/ebmh.10.3.69. [DOI] [PubMed] [Google Scholar]
- 13.Sloan DM, Marx B, Bovin MJ, Feinstein BA, Gallagher MW. Written exposure as an intervention for PTSD: a randomized clinical trial with motor vehicle accident survivors. Behav Res Ther. 2012;50:627–635. doi: 10.1016/j.brat.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pachalska M, Grochmal-Bach B, MacQueen BD, Franczuk B. Post-traumatic stress disorder in Polish stroke patients who survived Nazi concentration camps. Med Sci Monit. 2006;12:CR137–149. [PubMed] [Google Scholar]
- 15.Garland SN, Carlson L, Cook S, Lansdell L, Speca M. A non-randomized comparison of mindfulness-based stress reduction and healing arts programs for facilitating post-traumatic growth and spirituality in cancer outpatients. Support Care Cancer. 2007;15:949–961. doi: 10.1007/s00520-007-0280-5. [DOI] [PubMed] [Google Scholar]
- 16.Weathers FW, Keane TM, Davidson JR. Clinician-administered PTSD scale: a review of the first ten years of research. Depress Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- 17.Wang Y, Wang H, Wang J, Wu J, Liu X. Prevalence and predictors of posttraumatic growth in accidentally injured patients. J Clin Psychol Med Settings. 2013;20:3–12. doi: 10.1007/s10880-012-9315-2. [DOI] [PubMed] [Google Scholar]
- 18.Tan XF, Xia F. Long-term fatigue state in postoperative patients with breast cancer. Chin J Cancer Res. 2014;26:12–16. doi: 10.3978/j.issn.1000-9604.2014.01.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Findler L. The experience of stress and personal growth among grandparents of children with and without intellectual disability. Intellect Dev Disabil. 2014;52:32–48. doi: 10.1352/1934-9556-52.1.32. [DOI] [PubMed] [Google Scholar]
- 20.Moyer CA, Ekpo G, Calhoun CL, Greene J, Naik S, Sippola E, Stern DT, Adanu RM, Koranteng IO, Kwawukume EY, Anderson FJ. Quality of life, optimism/pessimism, and knowledge and attitudes toward HIV Screening among pregnant women in Ghana. Women’s Health Issues. 2006;18:301–309. doi: 10.1016/j.whi.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Berger R, Gelkopf M. School-based intervention for the treatment of tsunami-related distress in children: a quasi-randomized controlled trial. Psychother Psychosom. 2009;78:364–371. doi: 10.1159/000235976. [DOI] [PubMed] [Google Scholar]
- 22.Singer S, Gotze H, Buttstadt M, Ziegler C, Richter R, Brown A, Niederwieser D, Dorst J, Jakel N, Geue K. A non-randomised trial of an art therapy intervention for patients with haematological malignancies to support post-traumatic growth. J Health Psychol. 2013;18:939–949. doi: 10.1177/1359105312458332. [DOI] [PubMed] [Google Scholar]
- 23.Wang CH, Tsay SL, Bond AE. Post-traumatic stress disorder, depression, anxiety and quality of life in patients with traffic-related injuries. J Adv Nurs. 2005;52:22–30. doi: 10.1111/j.1365-2648.2005.03560.x. [DOI] [PubMed] [Google Scholar]
- 24.O’Donnell ML, Creamer MC, Parslow R, Elliott P, Holmes AC, Ellen S, Judson R, McFarlane AC, Silove D, Bryant RA. A predictive screening index for posttraumatic stress disorder and depression following traumatic injury. J Consult Clin Psychol. 2008;76:923–932. doi: 10.1037/a0012918. [DOI] [PubMed] [Google Scholar]
- 25.Sijbrandij M, Olff M, Opmeer BC, Carlier IV, Gersons BP. Early prognostic screening for posttraumatic stress disorder with the Davidson Trauma Scale and the SPAN. Depress Anxiety. 2008;25:1038–1045. doi: 10.1002/da.20441. [DOI] [PubMed] [Google Scholar]
- 26.Schuster MA, Stein BD, Jaycox L, Collins RL, Marshall GN, Elliott MN, Zhou AJ, Kanouse DE, Morrison JL, Berry SH. A national survey of stress reactions after the September 11, 2001, terrorist attacks. N Engl J Med. 2001;345:1507–1512. doi: 10.1056/NEJM200111153452024. [DOI] [PubMed] [Google Scholar]
- 27.Rubin GJ, Brewin CR, Greenberg N, Simpson J, Wessely S. Psychological and behavioural reactions to the bombings in London on 7 July 2005: cross sectional survey of a representative sample of Londoners. BMJ. 2005;331:606. doi: 10.1136/bmj.38583.728484.3A. [DOI] [PMC free article] [PubMed] [Google Scholar]


