Abstract
The flexible laryngeal mask airway (FLMA) is becoming more and more popular in general anesthesia during surgery of head, neck and upper chest. But very limited information has been published about whether muscle relaxant was necessary or not for anesthesia with FLMA. To investigate whether low-dose muscle relaxant is necessary in preventing ventilation leak of FLMA in radical mastectomy, forty-eight female patients undergoing radical mastectomy were enrolled in the study. They were randomly divided into low-dose muscle relaxant (LD-MR) group and non-muscle relaxant (non-MR) group. All the included patients received total intravenous anesthesia (with propofol, fentanyl and remifentanil) and controlled mechanical ventilation with FLMA during the surgery. Patients in LD-MR group received 0.4 mg/kg rocuronium during anesthesia induction, while patients in non-MR group received equivalent volumes of physiological saline. Insertion time was shorter in LD-MR group than that in non-MR group (P < 0.05). Peak airway pressures and ventilation leak volumes at 10, 20 and 30 minutes were lower in LD-MR group than those in non-MR group (P < 0.05). No difference was found between LD-MR and non-MR group in terms of emergence time, FLMA extraction time, and maximum tidal volumes before FLMA extraction. The results show that low-dose rocuronium could reduce the ventilation leak for mechanical ventilation with FLMA during radical mastectomy without prolonging the emergence time.
Keywords: Rocuronium, flexible laryngeal mask airway, radical mastectomy
Introduction
As a supraglottic device, laryngeal mask airway (LMA) is becoming more and more popular in general anesthesia. Compared with endotracheal intubation, LMA has more favorable hemodynamic profile and lower risk of airway complications including laryngospasm during emergence, postoperative hoarse voice, and coughing [1-4]. In our hospital, radical mastectomies for breast cancers were mainly conducted with LMA Proseal, Supreme and i-gel for the past three years. But LMA Proseal faded away from the stage of history because of the possibility of iatrogenic infection. While the rigid ventilation tube of LMA Supreme and i-gel may interfere the surgical field, and accidental dislocation of LMA may occur due to surgeon’s maneuver. The flexible LMA (FLMA) is a modified LMA with a wire-wrapped flexible breathing tube. It was specifically designed to improve surgical access and prevent cuff displacement during surgery of head, neck and upper chest [5]. But little information has been published about whether muscle relaxant was necessary or not for anesthesia with FLMA. Previous studies have shown that the oropharyngeal leak pressure of FLMA is around 18-20 cmH2O, which is lower than that of LMA Supreme and i-gel, meaning that a slight elevation in peak airway pressure may result in airway leak [6,9]. We assumed that muscle relaxant would be necessary to prevent air leak in mechanical ventilation with FLMA. In our hospital, the operation time of radical mastectomy is around 30-40 minutes. Drug studies showed that ten percent of the recovery of the first twitch of the train-of-four response after 0.45 mg/kg rocuronium occurred in a mean time of 27 min [7]. We hypothesized that low-dose rocuronium of 0.4 mg/kg could reduce the ventilation leak of FLMA during racial mastectomy.
Materials and methods
This prospective, randomized, and single-blinded control trial was approved by the Institutional Review Board of Peking Union Medical College Hospital (PUMCH) (IRB No. S-632). Written informed consent was received from each patient during the preoperative visit. From September 2013 to March 2014, forty-eight ASA I and II female patients, aged 29 to 67 years, scheduled for elective racial mastectomy under general anesthesia with FLMA were enrolled. Patients with cardiovascular, respiratory, hepatic, renal or neuromuscular diseases were excluded from the study. Exclusion criteria also included patients with body weight < 30 kg, BMI > 40 kg·m-2, known or suspected difficult airway and history of gastroesophageal reflux or increased risk factors for aspiration. These patients were not taking drugs known or suspected to interfere with neuromuscular transmission.
Sample size was difficult to calculate because few data had been found concerning the ventilation leak volume of FLMA with/without muscle relaxant. However, within our current sample size, the statistic power to detect the differences at each time point in both airway pressure and leak volume was over 0.8. Patients were randomly allocated to low dose muscle relaxant group (LD-MR group, n = 24) or non-muscle relaxant group (non-MR group, n = 24) by a computer-generated table of random numbers immediately prior to surgery, which was sealed in opaque envelopes containing the assignment. The patients, data collectors and outcome assessors were blinded to the group assignment. In order to ensure patients’ safety, the anesthesiologist in charge of the anesthesia was not blinded to the group assignment. One experienced anesthesiologist (Yi Jie) inserted all the FLMA, and three experienced surgeons performed the radical mastectomy.
On arrival at the operating room, all patients received midazolam 0.03 mg·kg-1 as a premedication. Intraoperative monitoring included electrocardiography, noninvasive blood pressure, pulse oximetry (SpO2), capnograpy (ETCO2), gas analysis, tidal volume, airway pressure and bispectral index (BIS). Anesthesia was induced with target-controlled infusion of propofol (at effect-site concentration of 3-3.5 ug/ml) and bolus injection of fentanyl 2 ug/kg. In LD-MR group, the patients also received 0.4 mg/kg rocuronium, while in non-MR group, they received equivalent volumes of physiological saline. After induction, an adequately deflated and lubricated FLMA (LMA FlexibleTM, Laryngeal Mask Company Limited, Seychelles, Singapore) was inserted with the standard digital insertion technique. The size of FLMA was decided according to the patients’ ideal body weight (size 3 (< 50 kg), 4 (50-70 kg), or 5 (> 70 kg)). Cuff pressure of FLMA was adjusted to 40 cmH2O with a handheld aneroid manometer (VBM, Einsteinstr, Germany) and proper position was confirmed by bronchoscopy. During bronchoscopy, a visualization of more than half vocal cords was considered a proper position. The oropharyngeal leak pressure was measured after closing the adjustable pressure limiting valve with a fresh gas flow of 3 L/min-1, noting the airway pressure at equilibrium or when there was an audible air leak from the throat. The maximum pressure allowed was 40 cmH2O.
During the operation, patients were in supine position with 45-degree head inclination to the non-operational side. Systolic blood pressure fluctuations was maintained within 15% of baseline and BIS value was between 40-60 (Aspect XP, space Lab, USA) with bolus injection of fentanyl and target controlled infusions (TCI) of propofol using Graseby 3500 Anaesthesia Syringe Pump-Diprifusor (Smiths-medical, UK). When the peak airway pressure elevated despite appropriate BIS value (40-60), another bolus of rocuronium 0.1 mg/kg was given in LD-MR group or remifentanil infusion in non-MR group. Propofol infusion was discontinued around 10 minutes before the surgery was over and neostigmine 3 mg was given to antagonize the residual muscle relaxant. FLMA was extracted when the patient could follow voice commands and EtCO2 was bellow 45 mmHg on spontaneous respiration.
Insertion time (from the beginning of FLMA insertion to the completion of first satisfied ventilation) and oropharyngeal leak pressure of FLMA were recorded. Peak airway pressure, inspired and expired tidal volumes were measured at insertion, 15, 30 and 60 minutes during surgery. Ventilation leak volume is the difference between the inspired and expired tidal volume. Air leak is defined as a ventilation leak volume > 100 ml. We calculated the incidence of air leak in each group by new cases at each time point divided by patients at risk of having air leak. During the emergence, FLMA extraction time (from the withdrawal of propofol to the extraction of FLMA) and maximum tidal volume were assessed and recorded. Total dosage of fentanyl, remifentanil and rocuronium were calculated in both groups.
Statistics
SPSS software (version 13.0; SPSS, Inc., Chicago, IL, USA) was used for data analysis. Continuous data were expressed as mean ± SD. Between-group numerical data with normal distribution were analyzed with unpaired t-test. Mann-Whitney U test was used to compare ventilation leak volume. A P-value < 0.05 was considered statistically significant.
Results
A total of 45 patients were included in our final analysis. One patient from LD-MR group was excluded because of a change in the operation plan. Two patients in non-MR group were excluded because rescue muscle relaxant was used intra-operatively due to inadequate ventilation. The two groups were comparable in age, body weight, height, BMI and operative time (Table 1).
Table 1.
Demographic data
| Group LD-MR (n = 23) | Group non-MR (n = 22) | P-value | |
|---|---|---|---|
| Age (yrs) | 51.6 ± 12.3 | 49.9 ± 8.9 | 0.080 |
| Body Weight (kg) | 64.3 ± 9.2 | 63.9 ± 8.9 | 0.829 |
| Body Height (cm) | 162.8 ± 4.6 | 161.3 ± 4.1 | 0.536 |
| BMI (kg/m2) | 24.3 ± 3.4 | 24.5 ± 3.2 | 0.793 |
| Operative time (min) | 38.1 ± 12.3 | 33.0 ± 9.1 | 0.279 |
Values are means ± SDs; LD-MR, low dose muscle relaxant group; non-MR, non-muscle relaxant group.
Insertion time of FLMA was significantly shorter in LD-MR group than that in non-MR group (21.4 ± 7.0 s vs 30.4 ± 13.6 s, P = 0.013), and the OLP was comparable in LD-MR and non-MR group (21.0 ± 5.1 cmH2O vs 19.6 ± 3.9 cmH2O, P = 0.448).
The peak airway pressures at 10, 20 and 30 minutes were significantly lower in LD-MR group than those in non-MR group (14.7 ± 2.8 cmH2O vs 18.8 ± 5.5 cmH2O, P = 0.002; 14.7 ± 2.3 cmH2O vs 17.0 ± 4.2 cmH2O, P = 0.026; 14.8 ± 2.2 cmH2O vs 17.8 ± 4.6 cmH2O, P = 0.035) (Figure 1). The ventilation leak volumes at insertion, 10, 20 and 30 minutes were significantly smaller in LD-MR group than those in non-MR group: 32.0 (11.8-40.0) ml vs 45.5 (23.5-58.3) ml, P = 0.04; 35.0 (21.0-48.0) ml vs 59.0 (43.5-80.3) ml, P = 0.002; 41.0 (27.0-55.0) ml vs 65.0 (41.0-83.8) ml, P < 0.001; 30.5 (20.0-42.0) ml vs 52.0 (34.0-83.5) ml, P = 0.003; (Figure 2). At 40 minutes, although the ventilation leak volume was smaller in LD-MR group than that in non-MR group (28.0 (18.0-35.0) ml vs 40.0 (11.0-92.5) ml, P = 0.185), the difference was not statistically significant. If a ventilation leak volume > 100 ml was considered as an air leak, the incidence of air leak in non-MR group was 0, 18.2% (4/22), 13.6% (3/22), 25.0% (3/12) and 16.7% (1/6) at 0, 10, 20, 30 and 40 minutes during surgery, while there was only one case with air leak at 10 minute (∆Vt = 100 ml) in LD-MR group.
Figure 1.
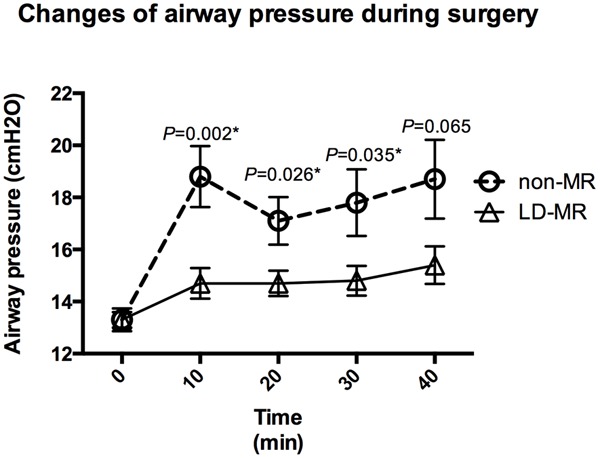
Peak airway pressures at 10, 20 and 30 minutes during the surgery were significantly lower in LD-MR group than those in non-MR group. *P < 0.05.
Figure 2.
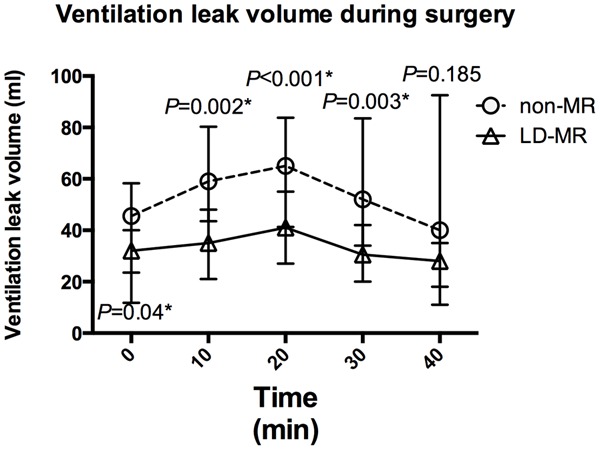
Ventilation leak volumes at 0, 10, 20 and 30 minute during the surgery were significantly smaller in LD-MR group than those in non-MR group. *P < 0.05.
There was no significant difference in the emergence (12.7 ± 4.9 s vs 11.0 ± 4.7 s, P = 0.813) and extraction time (15.3 ± 5.0 s vs 13.7 ± 4.0 s, P = 0.131) between LD-MR and non-MR group (Table 2). The maximum tidal volume of spontaneous breathing before extraction of FLMA was also comparable in LD-MR and non-MR group (558 ± 158 ml vs 516 ± 130 ml, P = 0.506, Table 2).
Table 2.
Emergence data
| Group LD-MR (n = 23) | Group non-MR (n = 22) | P-value | |
|---|---|---|---|
| Emergence Time (s) | 12.7 ± 4.9 | 11.0 ± 4.7 | 0.813 |
| Extraction Time (s) | 15.3 ± 5.0 | 13.7 ± 4.0 | 0.131 |
| Maximum Tidal Volume (ml) | 558.6 ± 158.5 | 516.4 ± 130.8 | 0.506 |
Values are means ± SDs; LD-MR, low dose muscle relaxant group; non-MR, non-muscle relaxant group.
In non-MR group, suddenly increased airway pressure (30 cmH2O and 32 cmH2O separately), massive ventilation leak (both over 300 ml) and hypercapnia (EtCO2 > 55 mmHg over 3 minutes) were noticed in two patients. Insufficient depth of anesthesia was suspected and anesthesia was deepened with propofol and remifentil. This resulted in hypotension (BP 85/56 mmHg and 90/63 mmHg, recovered with 6 mg epinephrine), but the airway pressure did not improve. Vocal cord closure was observed in one case by fibroscope. Airway pressure returned to normal levels after injection of 10 mg rocuronium in both cases.
Discussion
Low-dose rocuronium can reduce the insertion time, peak airway pressure and ventilation leak volume in patients undergoing breast surgery with FLMA, without prolonging the recovery time.
Previous studies have shown that for LMA proseal, muscle relaxant may not be necessary during insertion and mechanical ventilation [8]. According to the experience of our hospital, muscle relaxant can be spared for LMA i-gel and Supreme during radical mastectomy. But the OLP of FLMA is around 20 cmH2O, which is much lower than those of LMA Supreme, i-gel and Proseal [9]. Whether FLMA can provide an adequate seal for the patients without muscle relaxant in radical mastectomy is still unknown. This study showed that without muscle relaxant, the mean peak airway pressure was between 17.0 ± 4.2 cmH2O and 18.8 ± 5.5 cmH2O, which was very close to the OLP of FLMA (19.6 ± 3.9 cmH2O). This suggests that without muscle relaxant, airway pressure may easily exceed the OLP of FLMA, and a slight elevation in airway pressure may result in ventilation leak. Martin-Castro C. et al utilized FLMA in head and neck operation without muscle relaxants [10]. However, in order to avoid air leak, pressure controlled ventilation mode was used during the surgery. EtCO2 exceeded 44 mm H2O in 3 out of 60 patients, which indicated that ventilation was not adequate for these 3 patients during operation. These suggest that muscle relaxant may be necessary during general anesthesia with FLMA. The mechanism why low dose muscle relaxant could maintain a relatively lower airway pressure and prevent ventilation leak may be as follows: Muscle relaxant can reduce the tension of oropharyngeal muscles and prevent dislocation of FLMA resulting from contraction of oropharyngeal muscles; Muscle relaxant can improve the compliance of thorax and maintain a low airway pressure; Muscle relaxant can prevent spontaneous ventilation and patient-ventilator asynchrony. All these might contribute to less air leakage during surgery.
In this study, there were two patients in non-MR group whose peak airway pressure suddenly exceeded 30 cmH2O, and ventilation was not adequate due to severe air leak. The patients were easily ventilated after injection of 10 mg rocuronium in both cases and vocal cord closure was confirmed in one case by fibroscope. Kohno et al also reported 3 cases of sudden vocal cord closure in general anesthesia with LMA Proseal [11]. They suspected that the vocal cord closure may be ascribed to the administration of remifentanil, and suggested that supraglottic airway devices should be applied with caution during general anesthesia with remifentanil and sevoflurane without muscle relaxant. But in our cases vocal cord closure happened long after the administration of remifentanil, and sudden fierce operation stimulation seems to be the major cause. But whatever the cause is, low dose of muscle relaxant may help to alleviate the sudden vocal cord closure.
Previous studies also showed that a single intubating dose of non-depolarizing muscle relaxant with an intermediate duration of action might prolong the recovery time and cause residual muscle paralysis after surgery [12-14]. But compared with the standard intubating dose (0.6 mg/kg), low-dose rocuronium (0.45 mg/kg) could reduce the patient’s recovery time during short elective surgical procedures [13,15]. In this study, 0.4 mg/kg rocuronium was used in LD-MR group. Patient’s recovery time and maximum tidal volume at extubation were comparable to those of non-MR group. This suggests that low-dose of rocuronium rather than standard intubating dose is advisable in short surgery with FLMA.
This study has several limitations. Firstly, due to the lack of references, the sample size was not precise enough. Further large-sized randomized controlled trials were expected to confirm our results. Secondly, we found that the clinical recovery time was not prolonged in LD-MR group, but without muscle relaxation monitoring, we were not sure whether low dose muscle relaxant had resulted in residual neuromuscular blockade.
Low dose rocuronium could reduce the insertion time and prevent the ventilation leak of FLMA without prolonging the recovery time, suggesting that low dose muscle relaxant is advisable in radical mastectomy under general anesthesia with FLMA.
Discloure of conflict of interest
None.
References
- 1.Webster AC, Morley-Forster PK, Janzen V, Watson J, Dain SL, Taves D, Dantzer D. Anesthesia for intranasal surgery: a comparison between tracheal intubation and the flexible rein-forced laryngeal mask airway. Anesth Analg. 1999;88:421–425. doi: 10.1097/00000539-199902000-00037. [DOI] [PubMed] [Google Scholar]
- 2.Brimacombe J. The advantages of the LMA over the tracheal tube or facemask: a meta-analysis. Can J Anaesth. 1995;42:1017–1023. doi: 10.1007/BF03011075. [DOI] [PubMed] [Google Scholar]
- 3.Martin-Castro C, Montero A. Flexible laryngeal mask as an alternative to reinforced tracheal tube for upper chest, head and neck oncoplastic surgery. Eur J Anaesthesiol. 2008;25:261–266. doi: 10.1017/S0265021507002980. [DOI] [PubMed] [Google Scholar]
- 4.Yu SH, Beirne OR. Laryngeal mask airways have a lower risk of airway complications compared with endotracheal intubation: a systematic review. J Oral Maxillofac Surg. 2010;68:2359–2376. doi: 10.1016/j.joms.2010.04.017. [DOI] [PubMed] [Google Scholar]
- 5.Brimacombe JR. Flexible LMA for shared airway. In: Brimacombe JR, editor. Laryngeal Mask Anesthesia: Principles and Practice. 2nd edition. Philadelphia: WB Saunders; 2005. pp. 445–467. [Google Scholar]
- 6.Sunder RA, Sinha R, Agarwal A, Perumal BC, Paneerselvam SR. Comparison of Cobra perilaryngeal airway (CobraPLA™) with flexible laryngeal mask airway in terms of device stability and ventilation characteristics in pediatric ophthalmic surgery. J Anaesthesiol Clin Pharmacol. 2012;28:322–325. doi: 10.4103/0970-9185.98324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCoy EP, Mirakhur RK, Maddineni VR, Loan PB, Connolly F. Administration of rocuronium (Org 9426) by continuous infusion and its reversibility with anticholinesterases. Anaesthesia. 1994;49:940–945. doi: 10.1111/j.1365-2044.1994.tb04308.x. [DOI] [PubMed] [Google Scholar]
- 8.Chen BZ, Tan L, Zhang L, Shang YC. Is muscle relaxant necessary in patients undergoing laparoscopic gynecological surgery with a ProSeal LMATM? J Clin Anesth. 2013;25:32–35. doi: 10.1016/j.jclinane.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 9.Beleña JM, Núñez M, Anta D, Carnero M, Gracia JL, Ayala JL, Alvarez R, Yuste J. Comparison of Laryngeal Mask Airway Supreme and Laryngeal Mask Airway Proseal with respect to oropharyngeal leak pressure during laparoscopic cholecystectomy: a randomised controlled trial. Eur J Anaesthesiol. 2013;30:119–123. doi: 10.1097/EJA.0b013e32835aba6a. [DOI] [PubMed] [Google Scholar]
- 10.Martin-Castro C, Montero A. Flexible laryngeal mask as an alternative to reinforced tracheal tube for upper chest, head and neck oncoplasticsurgery. Eur J Anaesthesiol. 2008;25:261–266. doi: 10.1017/S0265021507002980. [DOI] [PubMed] [Google Scholar]
- 11.Kohno T, Ikoma M. Sudden vocal cord closure during general anesthesia using remifentanil. Masui. 2008;57:1213–1217. [PubMed] [Google Scholar]
- 12.Debaene B, Plaud B, Dilly MP, Donati F. Residual paralysis in the PACU after a single intubating dose of nondepolarizingmuscle relaxant with an intermediate duration of action. Anesthesiology. 2003;98:1042–1048. doi: 10.1097/00000542-200305000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Rapp HJ, Altenmueller CA, Waschke C. Neuromuscular recovery following rocuronium bromide single dose in infants. Paediatr Anaesth. 2004;14:329–335. doi: 10.1046/j.1460-9592.2003.01216.x. [DOI] [PubMed] [Google Scholar]
- 14.Gätke MR, Viby-Mogensen J, Rosenstock C, Jensen FS, Skovgaard LT. Postoperative muscle paralysis after rocuronium: less residual block when acceleromyography is used. Acta Anaesthesiol Scand. 2002;46:207–213. doi: 10.1034/j.1399-6576.2002.460216.x. [DOI] [PubMed] [Google Scholar]
- 15.Bartolek D, Jakobović J, Bartolek F, Finci D, Munjiza A. Reduced-dose rocuronium for day-case tonsillectomy in children where volatile anaesthetics are not used: operating room time saving. Paediatr Anaesth. 2010;20:47–55. doi: 10.1111/j.1460-9592.2009.03175.x. [DOI] [PubMed] [Google Scholar]


