Abstract
Purpose: To analyze the causes of anisometropia. Methods: Between June 2011 and November 2012 101 participants were divided into three groups. The refraction comprising the degree of refractive errors in the presence of astigmatism which was converted into the degree of spherical equivalent as well as ocular axial length (AL), corneal curvature (CR), average corneal power (ave K) and diopters were measured. Results: The differences of ocular AL/CR and CR between two eyes were statistically significant among the three groups (P < 0.05). Standardized regression coefficients obtained by a multiple linear regression analysis indicated that AL/CR, AL and ave K differences correlated with anisometropia in descending order. Conclusion: The difference of AL/CR ratios between the eyes was the main cause for anisometropia, followed by AL and ave K values.
Keywords: Axial length, corneal curvature, diopter, anisometropia, average corneal power
Introduction
Equal refraction rates between both eyes is rare in humans and ametropia commonly results in anisometropia, but there are differences in its nature and extends. The reported incidence rate of anisometropia ranges from 4 to 35% [1-4] which not only might cause monovision and amblyopia, but also lead to stereoscopic vision in patients with developmental disabilities. The main cause of ametropia is the imbalance of various refractive components, rather than a single optical aberration and the ocular refraction state is mainly influenced the two parameters corneal refractive power and ocular axial length (AL) [5]. From birth to the adulthood, the length of the ocular eye axis increases about 8 millimeter and in case that there are no corresponding adjustments of other factors to adapt to the growth of the eye axis, the misbalance can result in up to 20.0 diopter (D) myopias. During the development of the eyes, along with the growing ocular AL, the crystalline lens and cornea curvatures (CRs) gradually become flat in order to reduce the refractive power accordingly and to contradict the increased axial refraction changes to a certain degree, finally reducing myopia severity. Although the corneal refractive power mediates about three-fourths of the total eye refraction power, a number of clinical studies have shown that the ocular AL is also an important factor, which significantly influences the refractive state. Differences of ocular ALs growth rates between both eyes have been proposed to be the main cause for anisometropia in children [6]. Other reports pointed out that the length of the vitreous chamber, which grows fast in adolescence, but grows slow after adolescence would be the main reason for myopia in case the elongation takes place to fast [7]. However, the effect of different refractive components for developing anisometropia remains uncertain.
There are different classifications of anisometropia and criteria for anisometropia definitions are not standardized. In Iran, Britain and the United States the equivalent spherical lens difference between the eyes should not be less than 1.0D [5,8,9]. The pathological state for spherical lenses is in China defined as diopter difference between the eyes of more than 1.5D and for cylinder lenses more than 1D, whereas physiological anisometropia is defined as diopter differences of less than 1.5D between the eyes for spherical lenses and less than 1D for cylinder lenses [10]. In addition, it is generally accepted that the eyes cannot integrate vision if the retinal image difference is more than 5% (binocular diopter difference of more than 2.5D). In this study, binocular anisometropia was mainly myopic anisometropia and correlations of anisometropia with axial lengths and corneal refraction states were examined in order to develop predictive models.
Patients and methods
Patients
Between June 2011 and November 2012, patients of the Department of Ophthalmology of Guangdong General Hospital with refractive errors were selected according to the following inclusion criteria: (1) no history of trauma and surgery; (2) no other organic eye disorders; (3) no manifest strabismus in cover-uncover tests; (4) diopter range: -0.50D ~ -14.00D; (5) as AL is very changeable before adulthood, we selected patients between the age of 18 ~ 30 years. 101 patients were enrolled and divided into three groups based on the difference of the spherical equivalents (SEs). Group 1 comprised 21 male and 18 female patients with a mean age of 22.69 ± 3.38 years and range of spherical equivalent difference between the two eyes of < 1D. Group 2 included 15 male and 16 female patients with mean age of 24.4 ± 3.9 years and spherical equivalent differences of 1 ~ 2.5D. Group 3 consisted of 14 males and 17 females with mean age of 24.97 ± 3.88 years and spherical equivalent differences of ≥ 2.5D between the eyes. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research.
Measurements
The cycloplegic regimen consisted of a drop of 1% cyclopentolate repeated twice in 5-minute intervals. All measurements were performed at least 30 minutes after the last eye drop instillation. Cycloplegic auto-refraction measurements were performed using a Nidek ARK-510A (Nidek Ltd, Tokyo, Japan) instrument. Axial length and keratometry in two perpendicular meridians were obtained using an optical biometer based on optical coherence interferometry (IOL Master; Carl Zeiss, Germany). AL/CR values were determined with the horizontal corneal curvature method (the ratio of the ocular axis length and the horizontal corneal curvature). Ave K was determined as averages of horizontal and vertical axis curvatures. Each measurement consisted of an average of 3-5 scans.
Statistical analyses
The differences of AL, CR, AL/CR and diopter between the two eyes among the three groups were analyzed with Wilcoxon rank sum test. Bivariate and partial correlation, multiple linear regression, linear regression analysis and curve estimation were analyzed with a significance level of P < 0.05. All statistical analyses were done with SPSS statistics for windows, version 13 (Chicago, SPSS Inc.).
Results
Differences of diopter, AL, AL/CR and ave K between two eyes of three groups
The differences of Diopter, AL, AL/CR and ave K values between the two eyes are shown in Table 1. And were statistically significant among the three groups (P < 0.05).
Table 1.
Differences of Diopter, AL, AL/CR and ave K values between the two eyes in the three groups
| Group 1 | Group 2 | Group 3 | H value | df | P value | |
|---|---|---|---|---|---|---|
| Cases | 39 | 31 | 31 | 2 | ||
| Diopter | 0.44 ± 0.15 | 1.44 ± 0.40 | 4.44 ± 2.51 | 89.196 | 2 | 0.000 |
| AL | 0.13 ± 0.16 | 0.70 ± 0.58 | 1.68 ± 0.98 | 69.433 | 2 | 0.000 |
| AL/CR | 0.02 ± 0.02 | 0.09 ± 0.07 | 0.23 ± 0.13 | 68.096 | 2 | 0.000 |
| ave K | -0.01 ± 0.06 | 0.01 ± 0.07 | -0.03 ± 0.09 | 6.299 | 2 | 0.043 |
Correlation analysis
The correlation analysis results of differences between diopter and ocular parameters are shown in Table 2. There were medium correlations between diopter and AL as well as AL/CR differences in Group 2, but strong correlations of these parameters in Group 3. The correlations between the differences of AL and ave K are shown in Table 3. As correlations between the differences of diopter and AL/CR were found in each group, a comprehensive analysis of all data confirmed that there were linear correlations between diopter and AL/CR values (see Table 4).
Table 2.
Correlation analysis of ocular components and diopter differences (Control variables: age)
| Ocular Factors | Diopter difference (Group 1) | Diopter difference (Group 2) | Diopter difference (Group 3) | |||
|---|---|---|---|---|---|---|
|
| ||||||
| r | P | r | P | r | P | |
| AL difference | 0.195 | 0.241 | 0.572 | 0.001 | 0.921 | 0.000 |
| AL/CR difference | 0.424 | 0.008 | 0.635 | 0.000 | 0.947 | 0.000 |
| Ave K difference | -0.261 | 0.113 | -0.090 | 0.635 | -0.068 | 0.722 |
Table 3.
Correlation analysis of AL and ave K differences (Control variables: age)
| Difference of ave K | AL difference | |
|---|---|---|
|
| ||
| r | P | |
| Group 1 | 0.442 | 0.005 |
| Group 2 | 0.257 | 0.171 |
| Group 3 | 0.154 | 0.418 |
Table 4.
Correlation analysis of diopter and AL/CR differences in 101 cases (Control variables: age)
| Diopter difference | ||
|---|---|---|
|
|
||
| r | P | |
| AL/CR difference | 0.938 | 0.000 |
Multiple linear regression analysis
Based on the data from 101 cases using diopter difference as dependent variable and other ocular parameters as independent variables, the standardized regression coefficients obtained by a multiple linear regression analysis indicated that three independent variables affecting the dependent variable in descending order were as follows: difference in AL/CR, difference in AL, and difference in ave K (Table 5). After regression coefficients were standardized, the standardized regression coefficients were comparable.
Table 5.
Estimation of regression equations
| Partial Regression Coefficient | Standard Error of the Partial Regression Coefficient | Standard Regression Coefficient | t | P | |
|---|---|---|---|---|---|
| Constant | 0.111 | 0.495 | 0.224 | 0.823 | |
| AL difference | -5.778 | 2.272 | -2.381 | -2.544 | 0.013 |
| AL/CR difference | 61.555 | 17.407 | 3.370 | 3.536 | 0.001 |
| ave K difference | 19.946 | 7.322 | 0.654 | 2.724 | 0.008 |
Linear regression analysis of diopter differences and AL/CR ratio
The linear regression formula of diopter difference (Y) and AL/CR difference (X) was derived from the analysis of data collected from 101 cases: Y = 0.422+10.518x+23.055x2-16.208x3 (R2 = 0.894, P = 0.000) (Figure 1).
Figure 1.
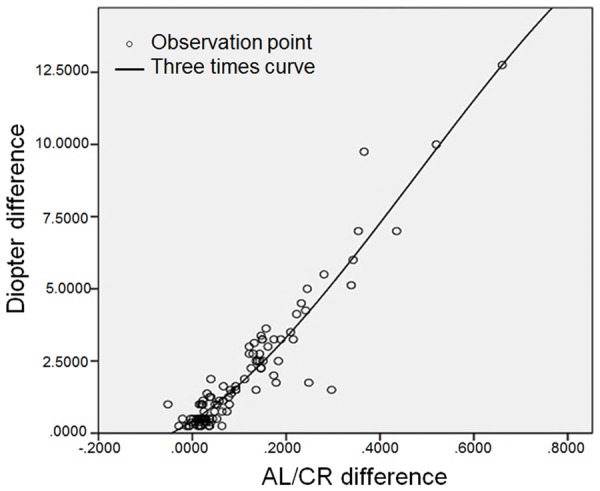
Scatter plot and curve estimation of AL/CR against diopter differences in 101 cases.
Predictive role of the linear regression equation
The regression equation Y = 0.422+10.518x+23.055x2-16.208x3 was verified with another 15 patients’ ocular parameters. The comparison between estimated Y and actual Y was perfectly consistent (R-square = 0.9697) (Figure 2).
Figure 2.
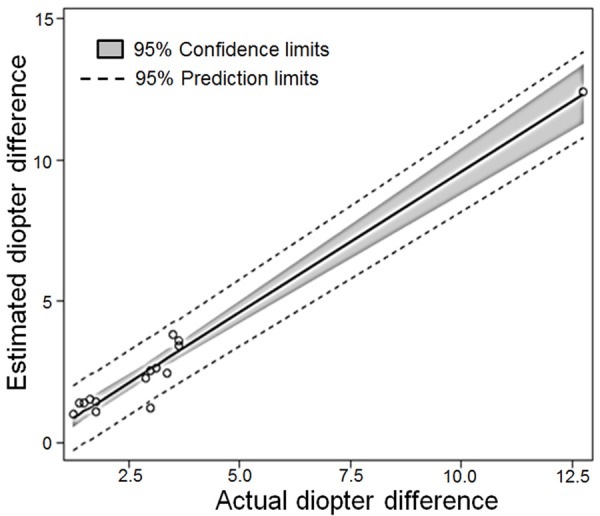
The scatter plot shows the consistency of predicted diopter difference against actual diopter difference from 15 test patients’ ocular parameters. Mean square error = 0.2584, R2 = 0.9697, adj R2 = 0.9674).
Discussion
In the current study, there were statistically significant differences of ocular AL and of CR between two eyes of patients among three groups. However, there was no correlation between diopter differences and ocular AL or CR of patients in group 1, whereas in groups 2 and 3, the linear correlation between diopter difference and ocular AL difference was increased with increasing differences of spherical equivalents; however, there was no correlation between the difference of refraction and the differences of CR. These findings suggest that the differences of ocular AL/CR ratios between both eyes were the main reason for anisometropia, while differences in corneal refractive power had little impact on the degree of anisometropia.
For all newborns, the refractive state is mostly hyperopic accompanied by some degree of astigmatism. Along with the development of the eyes, the degree of both hyperopia and astigmatism decreases gradually, and the refractive state of the eye develops to emmetropization, which is known as the “process of emmetropization”. In this process, the corresponding changes of the refractive components (cornea and/or lens) of the eye maintain the eye in an ‘emmetropia’ state. But with the increase of refraction and ocular AL, the corneal compensation decreases gradually and its emmetropization ability becomes limited in a certain range. If the development of the eyes leads to different refractive statuses or the initial refractive status is different, anisometropia may happen.
Gwiazda et al described that the degree of myopia did not differ by gender or ethnicity, but ninety-five percent of the eyes had a ratio of axial length to corneal radius higher than 3.0 [11]. Ojaimi et al reported that a peaked (leptokurtic) distribution of spherical equivalent refraction was present in a predominantly hyperopic 6-year-old children population and the distribution of ocular AL/CR ratio was peaked (leptokurtic) with a mean of 2.906 [12]. As conclusion, ocular AL/CR values higher than 3 are high-risk indicators to transform from emmetropia to myopia. Our results showed that in the process of eye emmetropization in order to achieve a binocular balance, there is a certain degree of corneal curvature compensation effect (increased radius of curvature is leading to a flattened cornea) with axial growth. If corneal compensation goes beyond the limits, unbalanced axis and corneal changes will appear and thus result in anisometropia, which is in accordance with previous literature which proposed that the best indicator of corneal emmetropization is the ratio of ocular AL/CR. If the ratio in emmetropia or mild myopia is more than 3, the compensation limit of the corneal curvature has been reached and if the axial length continues to grow the cornea cannot compensate further changes [13].
In this study, a multiple linear regression analyses showed that high ocular AL/CR values had the largest effect on refraction differences (Standard Regression Coefficient in Table 5) and can be used as an observational indicator to monitor the progress of anisometropia. Based on the data of diopter difference (Y) and ocular axis length/corneal curvature difference (X) from 101 patients, the regression formula has been calculated as Y = 0.422+10.518x+23.055x2-16.208x3. The coefficient of determination (R2) was 89.4%, which means the controllable variables were high. We also further verified the regression equation with other patients’ ocular parameters and obtained perfect consistency (R2 = 0.9697) between estimated values and actual measurements of diopter differences between the eyes, suggesting a predictive usefulness of our formula in practice.
The limitation of the current study was that the regression model was produced with a small sample size and further larger sample sizes from multi-center data are necessary to further verify the regression formula.
In summary, in our study we found that high ocular AL/CR values were the main reason for anisometropia, whereas differences in corneal refractive power had little impact on the degree of anisometropia.
Acknowledgements
The work was supported by the grants of Guangdong Science and Technology (2013-B021800178), Guangzhou Pearl River Nova of Science and Technology (2011J2200050), and National Natural Science Foundation of China (81371031).
Disclosure of conflict of interest
None.
References
- 1.de Vries J. Anisometropia in children: analysis of a hospital population. Br J Ophthalmol. 1985;69:504–507. doi: 10.1136/bjo.69.7.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu HM, Casson RJ, Newland HS, Muecke J, Selva D, Aung T. Anisometropia in an adult population in rural myanmar: the Meiktila Eye Study. Ophthalmic Epidemiol. 2008;15:162–166. doi: 10.1080/09286580701843796. [DOI] [PubMed] [Google Scholar]
- 3.Mohammadi E, Hashemi H, Khabazkhoob M, Emamian MH, Shariati M, Fotouhi A. The prevalence of anisometropia and its associated factors in an adult population from Shahroud, Iran. Clin Exp Optom. 2013;96:455–459. doi: 10.1111/cxo.12045. [DOI] [PubMed] [Google Scholar]
- 4.Zeng J, Guo H, Cui Y, Xie W, Li Z, Liao W. Early diagnosis of primary open-angle glaucoma in patients with high myopia after lase in situ keratomileusis (Chinese) Chinese Ophthalmic Research. 2010;28:441–444. [Google Scholar]
- 5.Hashemi H, Khabazkhoob M, Emamian MH, Shariati M, Abdolahi-nia T, Fotouhi A. All biometric components are important in anisometropia, not just axial length. Br J Ophthalmol. 2013;97:1586–1591. doi: 10.1136/bjophthalmol-2013-303939. [DOI] [PubMed] [Google Scholar]
- 6.Tong L, Saw SM, Chia KS, Tan D. Anisometropia in Singapore school children. Am J Ophthalmol. 2004;137:474–479. doi: 10.1016/j.ajo.2003.10.028. [DOI] [PubMed] [Google Scholar]
- 7.Wong HB, Machin D, Tan SB, Wong TY, Saw SM. Ocular component growth curves among Singaporean children with different refractive error status. Invest Ophthalmol Vis Sci. 2010;51:1341–1347. doi: 10.1167/iovs.09-3431. [DOI] [PubMed] [Google Scholar]
- 8.O’Donoghue L, Saunders KJ, McClelland JF, Logan NS, Rudnicka AR, Gilmartin B, Owen CG. Sampling and measurement methods for a study of childhood refractive error in a UK population. Br J Ophthalmol. 2010;94:1150–1154. doi: 10.1136/bjo.2009.167965. [DOI] [PubMed] [Google Scholar]
- 9.Deng L, Gwiazda JE. Anisometropia in children from infancy to 15 years. Invest Ophthalmol Vis Sci. 2012;53:3782–3787. doi: 10.1167/iovs.11-8727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Qi Y, Zhou YH. Effects of anisometropia and its correction to Binocular Vision. Journal of Capital Medical University. 2008;6:762–765. [Google Scholar]
- 11.Gwiazda J, Marsh-Tootle WL, Hyman L, Hussein M, Norton TT, Group CS. Baseline refractive and ocular component measures of children enrolled in the correction of myopia evaluation trial (COMET) Invest Ophthalmol Vis Sci. 2002;43:314–321. [PubMed] [Google Scholar]
- 12.Ojaimi E, Rose KA, Morgan IG, Smith W, Martin FJ, Kifley A, Robaei D, Mitchell P. Distribution of ocular biometric parameters and refraction in a population-based study of Australian children. Invest Ophthalmol Vis Sci. 2005;46:2748–2754. doi: 10.1167/iovs.04-1324. [DOI] [PubMed] [Google Scholar]
- 13.Yebra-Pimentel E, Giraldez MJ, Glez-Meijome JM, Cervino A, Garcia-Resua C, Parafita MA. [Changes in axial length/corneal radius ratio (AL/CR) according to refractive state of the eye. Relationship with ocular components] . Arch Soc Esp Oftalmol. 2004;79:317–324. doi: 10.4321/s0365-66912004000700004. [DOI] [PubMed] [Google Scholar]


