Abstract
Purpose: The treatment of posterolateral tibial plateau fracture remains controversial and challenging. Several approaches for this fracture have been applied for direct exposure and support plate fixation. However, several structures are to be at risk via posterior approach, which may affect exposure and plate application. To solve this problem, an extended anterolateral approach was developed and reported. Methods: 15 patients with posterolateral tibial plateau fractures treated with this approach were reviewed. The primary outcomes, such as Rasmussen functional score, and the secondary outcomes, such as knee deformity, postoperative infection, as well as complications were evaluated. Results: All 15 cases have been followed up for 12 to 30 months (19.7 months at average). Rasmussen functional score after surgeries was 25.0 ± 2.8 points. A score ≥ 27 points was considered as excellent (ten patients), a score of 20-26 points (four patients) was considered as good; and a score of 10-19 points (one patient) was considered as fair. Anatomic reductions were obtained in 14 patients, but a 3 mm gap was found in one patient. For all patients, there were no wound complications, nonunion, valgus knee deformities, plate loosening or breakages, or fracture re-displacements. No vascular or neural injuries occurred in any patient. Conclusion: The extended anterolateral approach provides excellent visualization, which can facilitate the internal fixation and reduction of posterolateral tibial plateau fractures, and shows encouraging results.
Keywords: Tibial fractures, therapeutics, internal fixators, surgical procedures, operative
Introduction
As the development of computer tomography technology, posterolateral tibial plateau fractures have been diagnosed with an increasing frequency. The incidence of posterolateral fractures was about 40%-50% in bicondylar tibial plateau fractures [1,2]. However, the management of posterolateral tibial plateau fractures is very difficult. It’s complicated anatomy, inadequate reduction and stabilization that may result in significant morbidity and knee flexion instability [3,4]. Because the tibial plateau fragments are often covered by the fibula head and ligamentous structures in the corner region of the popliteus muscle, the question of how to surgically address this fracture remains controversial. The anterior approaches had been favored for treating posterior tibial plateau fractures. The limitations and disadvantages in visualizing and manipulating the posterior column fracture through an anterior approach were recognized recently [5]. Luo et al [6] described an extended posteromedial approach where the posterolateral cortex of the proximal tibia could be exposed by subperiosteal dissection deeply into the popliteus muscle. Also, normal anatomic variation in the popliteal artery and its branches can, however, provide a challenge during this surgical dissection.
Besides anterior approaches, several approaches have been described for direct exposure and support plate fixation of posterolateral fractures [5,7-11]. It had been reported that two year results of seven patients with posterolateral tibial plateau fractures who had been cured by open reduction internal fixation (ORIF) via a novel posterolateral approach instead of a fibular osteotomy [7]. Articular reduction was performed in 6 of the 7 patients, whose gaps were ≤ 2 mm. Solomom et al [5] described a posterolateral trans-fibular neck approach. After surgery, there were not any signs of posterolateral or lateral instability of the knee joint or complications. In addition, differences had been found between an anterolateral indirect approach and a posterolateral direct approach in patients with fractures of unicondylar posterolateral tibial plateau [8]. It was suggested that a direct posterolateral transfibular approach to fractures of unicondylar posterolateral tibial plateau resulted in functional outcomes, stabilization as well as improved reduction at previous follow-up, when compared with an indirect anterolateral approach. However, the distance from the lateral tibial plateau to distal of the posterolateral approach was limited to as short as 27 mm. So, it should be careful to carry out dissections in this area [12]. Several structures were to be at risk during the posterior approach, which may affect the exposure and plate application. If there was a need to remove the plate during fracture, the exposure through a scarred tissue bed may also cause the risk of neurovascular structures damage.
An excellent approach should provide adequate articular visualization, combined with preservation of all vital structures and minimal soft tissue and osseous devitalization [9]. In order to solve the shortage of the above method, we developed an extended anterolateral approach [13] which might be relatively easy for reduction of fractures of the posterolateral tibial plateau without involving anterior tibial cortical.
Materials and methods
From January 2011 to December 2013, 15 cases of the posterolateral tibial plateau were collected and followed up in our study, which was retrospectively. This study design was approved by Human Experimental and Ethics Committee of our hospital for institutional reviews. All patients or their relatives agreed to participate in our research. Nine male and six female patients were enrolled in this study, ranging from 23 to 70 years old (average age 38.4 ± 7.7 years). These fractures involved seven left knees and eight right knees. Injuries were caused by traffic accidents in six patients, falling from height in seven patients and falling down when walking in two patients. All patients were treated with a locking compression plate LCP (Proximal Tibial Plate, Synthes, LCP 3.5, Switzerland) via the extended anterolateral approach.
Before surgery, patients were accessed by computed tomography (CT) scans, lateral and anteroposterior radiographic views. The fractures were classified according to the following classification system and based on the results of preoperative computed tomography (CT) scan results, which were displayed in Table 1.
Table 1.
The classification of fracture types and the number of patients in each type
| Classification of fracture types | Number of patients |
|---|---|
| Computed tomographic classification [10] | |
| Type I fracture | 0 |
| Type II fracture | 1 |
| Type III fracture | 6 |
| Type IV fracture | 3 |
| Type V fracture | 5 |
| Orthopedic trauma association classification [27] | |
| Type 41-B2 fracture | 11 |
| Type 41-B3 fracture | 3 |
| Type 41-B1 fracture | 1 |
Surgical procedure
The patient was placed in the back position after general anesthesia, whose thigh was compressed by a pneumatic tourniquet, and the surgical knee was maintained in a slightly flexed position. During surgery, antibiotic prophylaxis was administered routinely with a cephalosporin antibiotic. A 13 cm “S”-shaped incision was made, starting along the leading edge of the biceps femoris (at approximately 5 cm proximal to the knee crease) and extending down to a point approximately 1 cm distal to the knee crease. After a quarter turn, the incision was transversal and anterior, crossing Gerdy’s tubercle. Finally, the incision was followed the original direction to a point 1 cm lateral to the tibial tubercle and was extended distally (Figure 1A). The backside of the iliotibial band was cut and opened to separate the distal fiber bundles from Gerdy’s tubercle. Then, the knee was flexed to peel the iliotibial band along the upper edge of the fibular head. The lateral joint capsule and the patello-tibial ligament between the area below the meniscus and the tibial platform were cut and opened, and the lateral meniscus was lifted. The lateral collateral ligament and the popliteal tendon were pulled back to protect the peroneal nerve, while cutting the posterolateral joint capsule was not necessary. After checking the anterior, lateral, posterolateral, and entire lateral articular surfaces, the lower extremity was stretched straightly, with varus and internal rotations of the knee, to clearly expose the posterolateral tibial plateau fracture.
Figure 1.
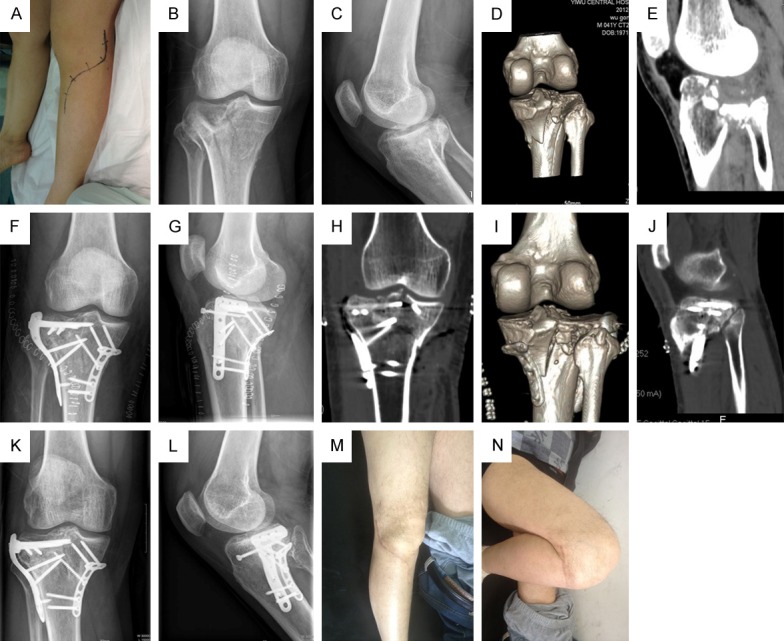
A: Incision of the extended anterolateral approach; B, C: Anteroposterior and lateral x-ray image of posterolateral tibial plateau fracture before surgery; D, E: CT films of obviously posterolateral tibial plateau fracture before surgery; F, G: Anteroposterior and lateral x-ray image of satisfied reduction of posterolateral tibial plateau fracture via extended anterolateral approach after surgery; H-J: CT films of anatomical reduction of posterolateral tibial plateau fracture after surgery; K, L: No fracture displacements during one year follow-up period after surgery; M, N: Satisfied flex function in the re-examination one year later after surgery.
Below the depressed articular fragments, a periosteal elevator was inserted well to elevate the articular fragments carefully and gently. In the posterolateral popliteal fossa, several Kirschner wires were used to fix the fragments temporarily. All patients were received a 3.5 system lateral tibial LCP. This structure provided supporting, maintained the reduction of the articular surface, and provided resistance against local depression loads. The plate head was properly placed above the fibular head that was free from resection in all patients. Four 3.5-mm locking screws from the plate head were used to fix the fracture fragments. The meniscus was sutured with caution back to the proximal screw or its attachment. After suction, the skin and the fascia were closed. Additionally, there were five patients with combined posteromedial tibial plateau split fractures (type V). A posteromedial T-plate was added via posteromedial approach to support the medial fracture. Intraoperative fluoroscopy was utilized to evaluate the reduction. For tibial plateau depression, the pressurized bone grafting was used to reduce the postoperative displacement.
Postoperative management
After surgery, physical treatment was prescribed particularly for muscle strengthening activities, and a passive motion device was applied for several hours every day. For 8-14 weeks, weight bearing was not allowed. Every four weeks until the fracture cured as well as once a year subsequently, regular radiographic examinations were performed postoperatively. A combination of radiographic and clinical criteria was applied during fracture union. Weight-bearing was based on clinical criteria when the fracture site got pain or tenderness. Radiographic criteria were followed when taking the anteroposterior and lateral radiographic views.
Data analyses
The primary outcome was a composite of myocardial infarction, stroke, or death from cardiovascular causes. After follow-up, Rasmussen functional score [11] was used to evaluate the function of patients after surgeries. There were five parameters included for calculation: severity of pain, deformity on knee extension, walking ability, knee joint stability, and knee joint motion, with a total score of six points in each parameter. The function was classified according to the total score as poor (6-9 points), fair (10-19 points), good (20-26 points) and excellent (≥ 27 points). The secondary outcome measures included respiratory symptoms, use of health care services, and airway reactivity. The secondary outcome indices included postoperative infection, a valgus knee deformity, and common peroneal nerve injury.
Results
Follow-ups were performed on all patients with an average time of 19.7 months (12-30 months). In CT scans and lateral and anteroposterior x-rays of all patients at follow-ups, near-anatomic reductions or anatomic reductions were found. According to the CT scans at follow-ups, only a 3 mm gap was measured in one patient and anatomic reductions were detected in the other 14 patients. There were no wound complications, nonunions, plate loosening or breakages, fracture re-displacements, or valgus knee deformities in any patient. No patients had neural or vascular injuries. No arthritis was found in these patients via imaging, with knee extension of 2.1 ± 2.1 and flexion of 120.6 ± 18.9 during the whole following-up period. The average Rasmussen functional score was 25.0 ± 2.8, including one patient with 10-19 points, four patients with 20-26 points, and 10 patients with ≥ 27 points. Rasmussen functional scores ≥ 20 points were found in 93.33% patients (Figure 1B-N; Table 2).
Table 2.
Operation details and outcome details (at final follow-up)
| Patient | Surgical duration (minute) | Bone graft | Complication | Follow-up time (month) | Rasmussen functional score | Intra-operative reduction | Fracture healing (weeks) | Intraoperative blood loss (ml) | Knee extension (°) | Knee flexion (°) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 80 | Yes | No | 12 | 30 | Anatomic | 8 | 100 | 0 | 140 |
| 2 | 80 | No | No | 23 | 29 | Anatomic | 9 | 112 | 0 | 135 |
| 3 | 100 | Yes | No | 24 | 25 | Anatomic | 9 | 321 | 3 | 130 |
| 4 | 80 | Yes | No | 12 | 26 | Anatomic | 10 | 151 | 2 | 123 |
| 5 | 120 | Yes | No | 14 | 22 | Anatomic | 10 | 385 | 4 | 100 |
| 6 | 80 | Yes | No | 24 | 27 | Anatomic | 12 | 109 | 2 | 140 |
| 7 | 85 | Yes | No | 30 | 21 | Anatomic | 12 | 182 | 4 | 109 |
| 8 | 130 | Yes | Yes | 14 | 14 | 3-mm depression of joint surface | 14 | 400 | 6 | 95 |
| 9 | 80 | Yes | No | 17 | 27 | Anatomic | 10 | 178 | 0 | 101 |
| 10 | 80 | Yes | No | 19 | 28 | Anatomic | 12 | 174 | 0 | 125 |
| 11 | 85 | Yes | No | 19 | 29 | Anatomic | 10 | 240 | 0 | 130 |
| 12 | 85 | Yes | No | 20 | 29 | Anatomic | 10 | 250 | 2 | 130 |
| 13 | 80 | Yes | No | 24 | 29 | Anatomic | 11 | 130 | 2 | 120 |
| 14 | 75 | Yes | No | 26 | 29 | Anatomic | 9 | 152 | 0 | 125 |
| 15 | 75 | Yes | No | 30 | 30 | Anatomic | 12 | 135 | 2 | 140 |
| 19.7 ± 2.3 | 25.0 ± 2.8 | 10.6 ± 1.8 | 211.2 ± 114.3 | 2.1 ± 2.1 | 119.8 ± 17.2 | |||||
Discussion
According to the results, extended anterolateral approach had advantages in posterolateral tibial plateau fractures when compared with other operative procedures. The posterolateral tibial plateau fracture is a hot topic in orthopedic traumatology in recent years. In fact, posterolateral tibial plateau fractures rarely happened, accounting for 7% of the total fractures of tibial plateau [14]. As computer tomography is becoming more and more commonly used in the diagnosis and evaluation of intra-articular fractures, this kind of fracture has been found with increasing frequency, but it is still not common in lateral and bicondylar tibial plateaus. Zhu et al [2] reported that the incidence of posterolateral fractures was 44.32% (164 in 370) in bicondylar tibial plateau fractures. There was also a similar report by Sohn et al [1] showing that eighty-four out of 190 tibial plateau fractures (44.2%) had a posterolateral fragment. The management of posterolateral tibial plateau fractures is very difficult due to its complicated anatomy, inadequate reduction and stabilization, which would result in significant morbidity and knee flexion instability [3]. For those posterolateral tibial plateau fractures which are displaced, operative treatment is suggested in clinical practice. The aims of treatment are anatomical reduction of articular surface, restoration of normal alignment of the knee joint, and provision of sufficient stability to allow early movement.
The management of posterolateral tibial plateau fractures remains controversial and challenging. However, the best therapy remains unknown. Considering the complicated anatomic structure of tibial plateau, minimally invasive lateral approach was not appropriate [15]. An extensive lateral approach to the tibial plateau was described by Gossling and Peterson in 1979 [16]. In the study, the entire lateral proximal tibia was exposed: Anterior, posterior and lateral. The lateral collateral ligament and the biceps femoris tendon were detached to expose the posterior plateau, in which fixation procedure was performed in the fibular head. If this did not suffice for bony exposure, then a partial or total fibular head osteotomy was performed. When an indirect anterolateral approach was applied, internal fixation devices were inserted properly after fracture reduction. However, because of the weakness of indirect visualization, malreduction may more probably happen with a potential result of inadequate fracture fixation. In recent years, directly posterior-lateral approach was popularly applied in the therapy of posterolateral tibial plateau fractures [5,7-11]. Chang et al [11] conducted eight cases of posterolateral tibial plateau fractures with supporting plate fixation and direct open reduction via a posterolateral approach. The average score of Hospital for Special Surgery (HSS) was 98 and the average dysfunction score of Short Musculoskeletal Functional Assessment (SMFA) was 15.8. All eight patients stated they were highly satisfied. However, in an another study by Chen’s group [10], the total Rasmussen function score was 24.8 ± 2.9 points. In their study, thirty two patients of posterolateral tibial plateau fractures were managed via a posterolateral approach by ORIF, without a fibular osteotomy. The results were classified as fair in 2 patients, good in 11, and excellent in 19 patients. No fracture re-displacements, implant fractures or screw loosening, wound infections, nonunions, or deformities were seen. However, in all of the described approaches, the limitation of dissection was as far as where the anterior tibial artery perforated the interosseous membrane. Kropman et al [17] in 2011 reported 15 articles with 7671 limbs, a variation in the popliteal artery and its trifurcation was seen in almost 10%. This is a great challenge for surgeons during manipulation through the posterolateral approach. Iatrogenic injury to the anterior tibial artery can lead to ischemic muscle necrosis of the compartment and skin loss [18].
With the development of surgical techniques and the progress of fixation materials, the anterolateral approach has been used by surgeons in recent years [19-24]. Sciadini et al [19] successfully used the lateral metaphyseal osteotomy technique to achieve anatomic reduction of lateral articular fractures and argued that lateral osteotomy was effective for visualization, reduction, and instrumentation of central and posterior lateral joint line impaction. Johnson et al [20] used anterolateral osteotomy for the internal fixation and reduction of lateral plateau fractures and used a bone knife to completely cut off the Gerdy’s tubercle in order to maximally expose the posterior fracture fragments. However, Frosch et al [7] reported an osteotomy for the lateral tibia plateau fracture, in which lateral buttress was more potentially inefficient and difficult. However, for fracture reduction, this significant disruption was not efficient. Hsieh et al [21] reported the therapy of posterolateral tibial plateau fractures in 15 patients with the anterior approach, 93% of which (14 patients) obtained articular reduction with satisfaction. During surgery, there were no wound complications, and no postoperative vascular or neural injuries. The average score of HSS was 92, ranging from 74 to 98. Bermudez et al [22] used an extensive anterolateral approach and tried to reconstruct and support the posterolateral bone with a horizontal plate. For posterolateral fragments, the anterolateral approach was extended so that a dissection around the biceps tendon and fibular head was possible. In order to expose the posterolateral articular surface of tibial plateau, lateral structures from the tibia and fibular head had to be detached as Z shape, and then the incision of those structures was surgically repaired before closing. Our approach was similar with them, but in our surgery there was no damage of any structures outside. So the trauma was significantly reduced.
Feasibilities of the method: 1) Our approach can clearly expose the articular surface of the lateral tibial plateau, can fully expose posterolateral tibial plateau fractures and benefit anatomical replacement through the method of rotating the knee flexion and opening the back side of the lateral collateral ligament. 2) According to anatomy, the distance between fibular head and the lateral articular surface of tibial plateau is 10.96 mm ± 3.49 mm, which can contain 3.5 system lateral tibia LCP. 3) According to the CT measurement of the lateral fracture fragment of tibial plateau, this fragment has an inverted conical shape that is a vertically oriented pattern and occupied nearly one-third of the surface area of the lateral tibial plateau, which can accommodate 3.5 system lateral tibia LCP. 4) Zhang et al [25] compared and analyzed biomechanical characteristics of four different types of internal fixation to stabilize posterolateral tibial plateau fractures. The posterolateral supporting plate could bear more load than other three groups. So, it was believed that although the supporting strength of the lateral LCP was not as strong as the direct backside steel, the stability of the fracture would not be affected under physiological load. Our clinical data also confirmed that the lateral locking plate support could fully meet the needs of clinical stability, making fixation more effective. Of all 15 patients with follow-up after surgery, there were no any cases of fixation loosening, displaced fracture fragments or collapses. 5) This method did not damage any important anatomical structures outside, protecting the stability of the knee. Without revealing the common peroneal nerve, there was no risk of peroneal nerve injury. The surgery was feasible and safe, and the removal of secondary fixation was simple, convenient and safe, without neurovascular damage complications by removing the lateral support plate out [26].
Defects of the method: 1) Preoperative CT scan should be carefully analyzed before surgery, because for those which the distance from fibular head to the articular surface of tibial plateau was less than 1 mm, it was not conducive to effective fracture fixation [13]. 2) There was not a surgery which could solve all the problems. So, for those posterolateral tibial plateau fractures which were near the middle of the tibia platform back, this method was not effective enough, making it necessary to perform an assistant lateral incision. 3) The main drawbacks of our study were retrospective with no control group, small sample population (15 patients) and short-term follow-up (12-30 months). Further random control study is necessary to determine the effect of our technique.
Conclusion
In conclusion, the extended anterolateral approach has the advantage to allow visualization of the posterolateral tibial plateau fragments with reduction facilitated. For the lateral supporting plate, adequate and safe posterior placement is ensured via the approach. Compared with an anterolateral approach, the plate can be positioned more posteriorly via this approach.
Acknowledgements
This study was supported by Key Science and Technology Program of Yiwu City (No. 2009-G3-02).
Disclosure of conflict of interest
None.
References
- 1.Sohn HS, Yoon YC, Cho JW, Cho WT, Oh CW, Oh JK. Incidence and Fracture Morphology of Posterolateral Fragments in Lateral and Bicondylar Tibial Plateau Fractures. J Orthop Trauma. 2015;29:91–7. doi: 10.1097/BOT.0000000000000170. [DOI] [PubMed] [Google Scholar]
- 2.Zhu Y, Meili S, Dong MJ, Zhai QL, Yao L, Wang JC, Hu CF, Sun H, Luo CF. Pathoanatomy and incidence of the posterolateral fractures in bicondylar tibial plateau fractures: a clinical computed tomography-based measurement and the associated biomechanical model simulation. Arch Orthop Trauma Surg. 2014;134:1369–1380. doi: 10.1007/s00402-014-2037-1. [DOI] [PubMed] [Google Scholar]
- 3.Waldrop JI, Macey TI, Trettin JC, Bourgeois WR, Hughston JC. Fractures of the posterolateral tibial plateau. Am J Sports Med. 1988;16:492–498. doi: 10.1177/036354658801600511. [DOI] [PubMed] [Google Scholar]
- 4.Madadi F, Eajazi A, Madadi F, Daftari Besheli L, Sadeghian R, Nasri Lari M. Adult tibial shaft fractures-different patterns, various treatments and complications. Med Sci Monit. 2011;17:CR640–645. doi: 10.12659/MSM.882049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Solomon LB, Stevenson AW, Baird RPV, Pohl AP. Posterolateral transfibular approach to tibial plateau fractures: technique, results, and rationale. J Orthop Trauma. 2010;24:505–514. doi: 10.1097/BOT.0b013e3181ccba4b. [DOI] [PubMed] [Google Scholar]
- 6.Luo CF, Sun H, Zhang B, Zeng BF. Three-column fixation for complex tibial plateau fractures. J Orthop Trauma. 2010;24:683–692. doi: 10.1097/BOT.0b013e3181d436f3. [DOI] [PubMed] [Google Scholar]
- 7.Frosch KH, Balcarek P, Walde T, Stürmer KM. A new posterolateral approach without fibula osteotomy for the treatment of tibial plateau fractures. J Orthop Trauma. 2010;24:515–520. doi: 10.1097/BOT.0b013e3181e5e17d. [DOI] [PubMed] [Google Scholar]
- 8.Solomon LB, Stevenson AW, Lee YC, Baird RPV, Howie DW. Posterolateral and anterolateral approaches to unicondylar posterolateral tibial plateau fractures: a comparative study. Injury. 2013;44:1561–1568. doi: 10.1016/j.injury.2013.04.024. [DOI] [PubMed] [Google Scholar]
- 9.Sun H, Luo CF, Yang G, Shi HP, Zeng BF. Anatomical evaluation of the modified posterolateral approach for posterolateral tibial plateau fracture. Eur J Orthop Surg Traumatol. 2013;23:809–818. doi: 10.1007/s00590-012-1067-z. [DOI] [PubMed] [Google Scholar]
- 10.Chen HW, Liu GD, Ou S, Zhao GS, Pan J, Wu LJ. Open reduction and internal fixation of postero-lateral tibial plateau fractures through fibula osteotomy-free postero-lateral approach. J Orthop Trauma. 2014;28:513–517. doi: 10.1097/BOT.0000000000000047. [DOI] [PubMed] [Google Scholar]
- 11.Chang SM, Zheng HP, Li HF, Jia YW, Huang YG, Wang X, Yu GR. Treatment of isolated posterior coronal fracture of the lateral tibial plateau through posterolateral approach for direct exposure and buttress plate fixation. Arch Orthop Trauma Surg. 2009;129:955–962. doi: 10.1007/s00402-009-0829-5. [DOI] [PubMed] [Google Scholar]
- 12.Heidari N, Lidder S, Grechenig W, Tesch NP, Weinberg AM. The risk of injury to the anterior tibial artery in the posterolateral approach to the tibia plateau: a cadaver study. J Orthop Trauma. 2013;27:221–225. doi: 10.1097/BOT.0b013e318271f8f0. [DOI] [PubMed] [Google Scholar]
- 13.Chen HW, Zhou SH, Liu GD, Zhao X, Pan J, Ou S, Fei J. An extended anterolateral approach for posterolateral tibial plateau fractures. Knee Surg Sports Traumatol Arthrosc. 2014:1–6. doi: 10.1007/s00167-014-3304-y. [DOI] [PubMed] [Google Scholar]
- 14.Partenheimer A, Gösling T, Müller M, Schirmer C, Kääb M, Matschke S, Ryf C, Renner N, Wiebking U, Krettek C. Management of bicondylar fractures of the tibial plateau with unilateral fixed-angle plate fixation. Unfallchirurg. 2007;110:675–683. doi: 10.1007/s00113-007-1271-1. [DOI] [PubMed] [Google Scholar]
- 15.Liu K, Liu PC, Liu R, Wu X. Advantage of minimally invasive lateral approach relative to conventional deltopectoral approach for treatment of proximal humerus fractures. Med Sci Monit. 2015;21:496–504. doi: 10.12659/MSM.893323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gossling HR, Peterson CA. A new surgical approach in the treatment of depressed lateral condylar fractures of the tibia. Clin Orthop Relat Res. 1979;140:96–102. [PubMed] [Google Scholar]
- 17.Kropman RHJ, Kiela G, Moll FL, de Vries JP. Variations in anatomy of the popliteal artery and its side branches. Vasc Endovascular Surg. 2011;45:536–540. doi: 10.1177/1538574411409065. [DOI] [PubMed] [Google Scholar]
- 18.Gao X, Pan ZJ, Zheng Q, Li H. Morphological characteristics of posterolateral articular fragments in tibial plateau fractures. Orthopedics. 2013;36:e1256–1261. doi: 10.3928/01477447-20130920-16. [DOI] [PubMed] [Google Scholar]
- 19.Sciadini MF, Sims SH. Proximal tibial intra-articular osteotomy for treatment of complex Schatzker type IV tibial plateau fractures with lateral joint line impaction: description of surgical technique and report of nine cases. J Orthop Trauma. 2013;27:e18–e23. doi: 10.1097/BOT.0b013e31825316ea. [DOI] [PubMed] [Google Scholar]
- 20.Johnson EE, Timon S, Osuji C. Surgical technique: Tscherne-Johnson extensile approach for tibial plateau fractures. Clin Orthop Relat Res. 2013;471:2760–2767. doi: 10.1007/s11999-013-2962-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hsieh CH. Treatment of the posterolateral tibial plateau fractures using the anterior surgical approach. Int J Biomed Sci. 2010;6:316. [PMC free article] [PubMed] [Google Scholar]
- 22.Bermúdez CA, Ziran BH, Barrette Grischow MK. Use of horizontal rafting plates for posterior elements of complex tibial plateau fractures: description and case reports. J Trauma. 2008;65:1162–1167. doi: 10.1097/01.ta.0000222943.45563.b5. [DOI] [PubMed] [Google Scholar]
- 23.Fang X, Jiang L, Wang Y, Zhao L. Treatment of Gustilo grade III tibial fractures with unreamed intramedullary nailing versus external fixator: a meta-analysis. Med Sci Monit. 2012;18:RA49–56. doi: 10.12659/MSM.882610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gao YS, Li SZ, Zhu ZH, Zhang CQ, Mei J. Stabilizing severely open fractures of the tibia with a surgical suture: an alternative and feasible method for osteosynthesis. Med Sci Monit. 2010;16:CS143–147. [PubMed] [Google Scholar]
- 25.Zhang W, Luo CF, Putnis S, Sun H, Zeng ZM, Zeng BF. Biomechanical analysis of four different fixations for the posterolateral shearing tibial plateau fracture. Knee. 2012;19:94–98. doi: 10.1016/j.knee.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 26.Huang YG, Chang SM. The posterolateral approach for plating tibial plateau fractures: problems in secondary hardware removal. Arch Orthop Trauma Surg. 2012;132:733–734. doi: 10.1007/s00402-012-1459-x. [DOI] [PubMed] [Google Scholar]
- 27.Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B. Fracture and dislocation classification compendium-2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21:S1–S6. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]


