Abstract
Uric acid stone is the most comment radiolucent renal stone with high recurrence rate, which would further cause acute upper urinary tract obstruction and kidney failure. Here we report two cases of renal uric acid stone from December 2012 to April 2013. One 43-year-old male patient suffered from chronic uric acid nephrolithiasis caused by the long-term indwelling of bilateral double-J stent. Another 69-year-old patient was also diagnosed with uric acid nephrolithiasis at the right kidney. Both patients were first treated with extracorporeal shock wave lithotripsy (ESWL), followed by 1.5% sodium bicarbonate dissolution therapy. After a week of the treatment, the uric acid stones in both patients were completely dissolved without retrograde infection. In summary, the use of ESWL and sodium bicarbonate dissolution therapy as a combined modality is a safe, effective, inexpensive treatment for uric acid nephrolithiasis.
Keywords: Renal acid stone, extracorporeal shock wave lithotripsy, uric acid nephrolithiasis, sodium bicarbonate
Introduction
Uric acid stone is the most common radiolucent renal stone with high recurrence rate, which would further cause acute upper urinary tract obstruction and kidney failure. Previous clinical studies have shown that urine alkalinization with potassium citrate or sodium bicarbonate was a highly effective non-surgical treatment for dissolving uric acid stones [1,2]. Herein we have demonstrated the treatment effects of ESWL combined with sodium bicarbonate dissolution therapy on two patients diagnosed with renal uric acid stones from December 2011 to April 2013.
Case reports
Case I
A 43-year-old male was admitted to our hospital with a 5-month history of bilateral loin pain. Five months ago, he was first hospitalized for chronic bilateral loin pain and anuria for two days. He was later diagnosed with acute obstructive renal failure caused by renal and ureteral calculi. Ureteroscopic lithotripsy and ureteral stenting (double-J stent) were performed. Six days after the first treatment, the patient’s creatinine level was back to normal, and he was advised to go through percutaneous nephrolithotomy. However, the patient refuse any further treatment due to the personal financial condition, and did not return later for the double-J stent removal or further renal stone treatment as suggested. At the end of November 2011, the patient was hospitalized again for chronic loin pain; cystoscopy reading indicated that large bladder stones were formed at the end of the double-J stent, and thus the stent could not be removed; Renal color Doppler ultrasound also revealed the bilateral renal calculi and the uric acid stones at the tips of the stent in the renal pelvis. The patient was then transferred to our hospital. His physical examination on admission showed the following: no renal distention, tenderness or percussion pain; no tenderness at both upper and middle ureter; no bladder distention or tenderness. Renal color Doppler ultrasound result suggested bilateral renal calculi, as one hyper-echoic mass (31 mm × 14 mm) in the lower calyx of the left kidney and another hyper-echoic mass (45 mm × 15 mm) located in the pelvis of the right kidney were observed, with acoustic shadow; right kidney showed mild hydronephrosis with dilatation (≤14 mm); the indwelling double-J stent was also clearly observed. Computed Tomography (CT) scanning indicated the stent placement at the renal pelvis and upper ureter with higher dense rim, and renal calculi at the lower calyx of the right kidney (Figure 1). Intravenous Pyelogram (IVP) result also suggested mild hydronephrosis of right kidney with normal kidney function, yet no radiopaque calculus was observed. Among the laboratory tests, blood uric acid (BUA) was 617.4 μmol/L, creatinine was 119 mol/L, and urine pH was 5.0, which suggested renal uric acid stone. Therefore, our final diagnosis was uric acid nephrolithiasis in both kidneys including the tips of the inserted double-J stent. On November 30 of 2011, after ultrasonic localization, the patient underwent ESWL using the lithotripter purchased from Zhanjiang Haibin Medical Equipment Co., Ltd (model: HB-ESWL-V). During one session of ESWL, 2500 shock waves (energy range of 7~9 kV) were delivered for 30 mins. The uric acid stones were partly disintegrated and the small fragments were discharged through the ureter right after the lithotripsy. Two days after the ESWL, the stent located at the left kidney was successfully removed by performing cystoscopy, yet the stent at the right kidney could not be removed due to the large size of the residual fragments. Thus a retrograde ureteral stenting was performed and an F5 ureteral catheter was inserted to the right renal pelvis, followed by another session of ESWL. After the ESWL, 1.5% sodium bicarbonate solution was then steadily dripped into the ureteral catheter for urine alkalization. The follow-up renal ultrasonography on December 7of 2011 showed no evidence of stone fragments, and the stent indwelled in the right kidney was also successfully removed (Figure 2).
Figure 1.
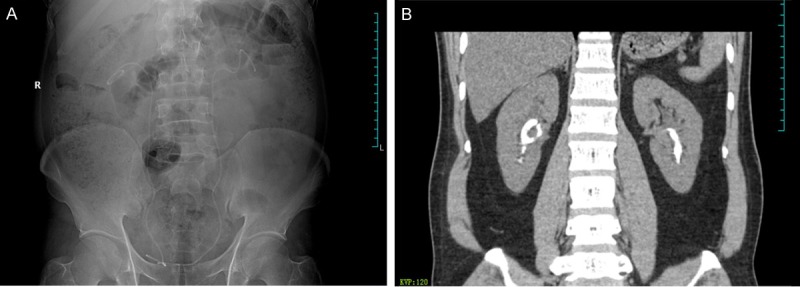
Male patient, 43 year-old, with history of renal uric acid calculi, suffered from chronic uric acid nephrolithiasis caused by the long-term (6 months) indwelling of bilateral double-J stent. A: KUB radiography result indicated that the double-J stent was in place, and no trace of renal stone. B: CT scanning indicated the bilateral renal stones at the end of the double-J stent.
Figure 2.
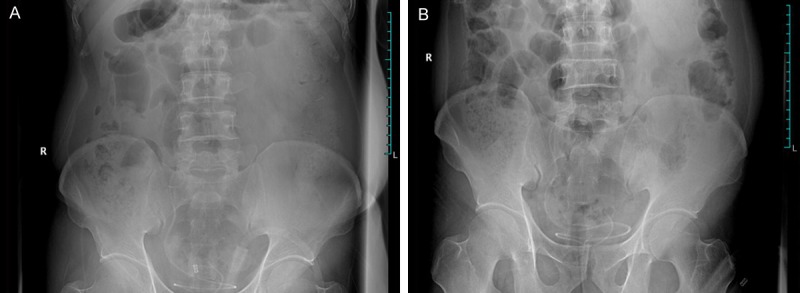
The patient underwent ESWL on November 30 of 2011. Two days after the ESWL, the stent located at the left kidney (A) was successfully removed by performing cystoscopy, yet the stent at the right kidney (B) could not be removed due to the large size of the residual fragments. An F5 ureteral catheter was inserted to the right renal pelvis, followed by another session of ESWL. After the ESWL, 1.5% sodium bicarbonate solution was then steadily dripped into the ureteral catheter for urine alkalization. The follow-up renal ultrasonography on December 7 of 2011 showed no evidence of stone fragments, and the stent left in the right kidney was also successfully removed.
Case II
A 69-year-old patient, with a 10-year history of gout, was admitted to our hospital for 2 months of chronic right loin pain. The physical examination on admission showed the following: no renal distention, tenderness or percussion pain; no tenderness at both upper and middle ureter; no bladder distention or tenderness. Renal color Doppler ultrasound suggested right renal calculi, as hyper-echoic mass was observed in the pelvis of the right kidney with acoustic shadow. CT scanning showed an irregular mass measuring 32 mm × 13 mm in size with higher density (Figure 3). The shape of both kidneys did not show up clearly in the KUB radiography; a radiolucent shadow with the size of 30 mm × 13 mm was observed in the right kidney; no evidence of radiopaque calculus shown in the left kidney. IVP result suggested mild hydronephrosis of the right kidney with normal kidney function, and also no radiopaque calculus was observed. Among the laboratory tests, BUA was 570.8 μmol/L, creatinine was 121.3 mol/L and urine pH was 5.2. The final diagnosis was nephrolith (uric acid stones) in the right kidney. On November 30 of 2011, after urinary drainage by placing a ureteral catheter and ultrasonic localization, the patient underwent ESWL using the same lithotripter with 2500 shock waves (energy range of 7~9 kV) for 30 mins. After the ESWL, 1.5% sodium bicarbonate solution was then steadily dripped into the ureteral catheter for urine alkalization. The follow-up renal ultrasonography on April 7of 2013 showed no trace of stone fragments, and the ureter catheter left in the right kidney was removed (Figure 4).
Figure 3.
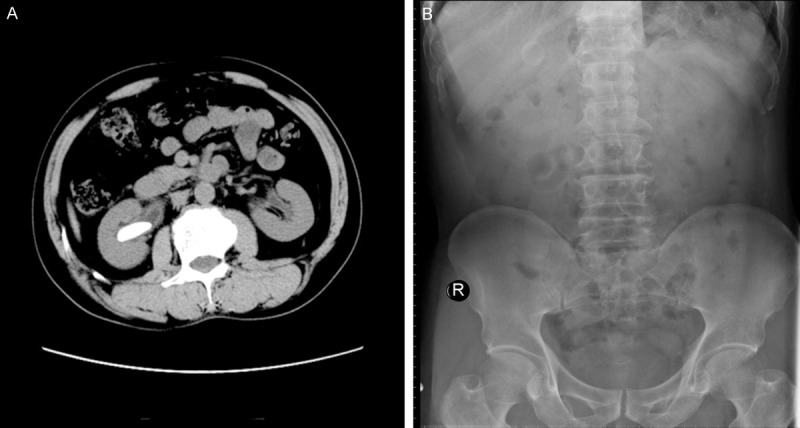
Male patient, 69 year-old. A: CT scanning showed an irregular mass measuring 32 mm × 13 mm in size with higher density. B: The shape of both kidneys did not show up clearly in the KUB radiography; a radiolucent shadow with the size of 30 mm × 13 mm was observed in the right kidney; no evidence of radiopaque calculus shown in the left kidney.
Figure 4.
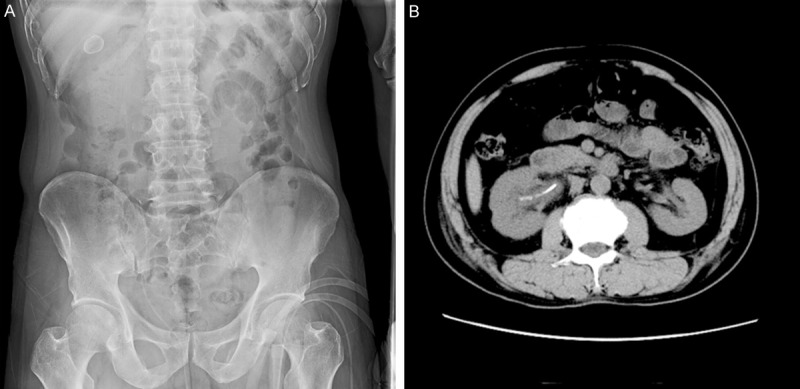
On November 30 of 2011, after placing a ureteral catheter and the ESWL, 1.5% sodium bicarbonate solution was then steadily dripped into the ureteral catheter for urine alkalization. The follow-up renal ultrasonography (A) and CT (B) on April 7 of 2013 showed no trace of stone fragments but only the ureter catheter.
Discussion
Three major types of renal stone found in patients with uric acid nephrolithiasis are: 1) pure uric acid stone; 2) mixed stone containing uric acid and some other components, such as ammonium urate and sodium urate; 3) mixed stone containing only uric acid and calcium oxalate, which formation involved the nucleation and growth of calcium oxalate monohydrate (COM) crystals. Approximately 5%~8% people were diagnosed with urolithiasis in the Western countries, versus 3%~5% in China. This number keeps going up in the past decade due to the increased intake of protein in people’s daily diet [3].
Uric acid is a weak organic acid with a pKa of 5.5. It exists in our body in two forms: non-dissociated uric acid and urate ions, which depends on the biological pH. When the blood pH is in the normal range of 7.35~7.45, it forms dissociated acid urate ions and thus prevents the formation of uric acid stone. The normal uric acid level for adult male is between 268~488 umol/L, and that for adult female before menopause is 178~378 umol/L. Urate ions can pass through the glomeruli and is re-absorbed in the proximal renal tubule. Under the normal condition, approximately 400~1000 mg of uric acid (~10%) is excreted via urination. Extra endogenous uric acid can also be degraded into carbon dioxide and ammonia and released as intestinal gas [4].
Hyperuricosuria, low urinary volume, and low urinary pH are three major risk factors in causing uric acid nephrolithiasis, with the latter being the most prevalent and important. As mentioned earlier, under the normal biological pH, it forms either soluble urate or insoluble uric acid. Alkalization of urine not only prevents the formation of uric acid stone but can also dissolve them, as the insoluble uric acid is transformed to the soluble urate at higher urinary pH. The standard of urinary alkalization is to achieve a pH of 6~6.5 with proper titration using pH paper until the pH of urine is stable [5]. Thus urine alkalization is considered as the effective treatment for uric acid nephrolithiasis.
Intravenous (IV) fluid therapy, urine alkalization and dilution of urine by increasing the liquid intake are the conventional treatment methods for nephrolithiasis with 47~100 % success rate [1]. However, some drugs used for dissolving renal stone have unwanted side effects and normally required long-term treatment. Some patients can not adhere to the treatment plan, and it thus eventually leads to treatment failure. For patients with acute kidney failure or urinary obstruction caused by renal stones, conservative drug treatment might worsen the course of the disease. It has been previously reported that, Percutaneous Nephrolithotomy (PNC) followed by oral dissolution therapy with 1.6% sodium bicarbonate for 12 days could cure the patients with upper ureter obstruction caused by renal stones [6-8]. In another case, a stone-free rate of 100% was achieved in 24 patients (2~12-year old) with renal uric acid stones after 3 months of combined use of ESWL and oral dissolution therapy with granule of potassium sodium hydrogen citrate [9]. However, patient undergoing PNC might have the risk of major internal bleeding or infection. Also long-termed oral dissolution treatment with alkali agents will develop serious side effects. Therefore, in this study, we have developed a procedure in which urine alkalization was achieved by injecting 1.5% sodium bicarbonate solution through the retrograde ureter catheter following the ESWL.
The first patient in this study was diagnosed with upper ureter obstruction caused by uric acid stones. Ureteroscopic lithotripsy and ureteral stenting (double-J stent) were performed to prevent the acute kidney failure. However, he failed to go back for the stent removal and treatment as required, which directly caused the deposition of the uric acid crystals on the double-J stent and eventually led to uric acid stone formation. As the crystallization and crystal nucleation proceeded, we were not able to remove the stent without a surgical procedure. However, considering the patient’s financial condition, we could only apply the non-surgical and conservative dissolution therapy. The second patient in the study also suffered from uric acid nephrolithiasis. His family did not agree on the surgical treatment considering the fact that the patient was 69-year old, and thus non-surgical dissolution therapy was the only option.
During the treatment, we first performed the ESWL and retrograde ureteral stenting with an F5 ureteral catheter inserted to the renal pelvis. 1.5% sodium bicarbonate solution was then steadily dripped into the ureteral catheter for further urine alkalization. This combination treatment has been proved to be effective in renal uric acid stone dissolution and its main advantages are: 1) As uric acid nucleation is facilitated in the presence of calcium, the surface of uric acid stone is usually covered with calcium oxalate which is hard to dissolve in the alkali solution. The ESWL prior to the urine alkalization helps to remove the calcium oxalate shield and facilitate the dissolution; 2) After the ESWL, the uric acid calculi are disintegrated into small pieces, which also facilitate the dissolving process; 3) Steady injection of 1.5% sodium bicarbonate solution to the renal pelvis helps the urine pH to remain in the optimal range; 4) The urethral opening is widened upon the ureteral catheter placement, which helps the stone excretion; 5) Injection of sodium bicarbonate solution directly increases urination, which also promotes the stone excretion.
When steadily dripping the 1.5% sodium bicarbonate solution to the renal pelvis, one has to make sure both the inserted catheter and the ureter are unblocked. In case I, considering the fact that the patient had already had a double-I stent inserted, we therefore chose an F5 ureteral catheter with relatively small diameter for the dissolution therapy. Moreover, as the ureteral catheter is normally placed in the ureter for a certain period during the treatment, IV injection of antibiotics is strongly recommended along with the dissolution therapy to prevent the retrograde infection. The renal pelvis pressure should be closely monitored during the dissolution treatment as fluid overload can cause renal colic, extra liquid absorption and tissue damage. 1.5% of sodium bicarbonate is proved to be the optimal concentration for stone dissolution. If the salt concentration was too low, the dissolution process will not be efficient; On the other hand, if the salt concentration was too high, it will easily cause tissue damage and renal coli as the pH level is too high. Therefore, the treatment should be carried out with extra caution to prevent complication, such as infection and extravasations. The injection of the sodium carbonate solution should be terminated immediately when acute loin pain, fever or blood in urine was observed. The 1.5% sodium bicarbonate solution used in this study was produced by adding 150 mL of 5% sodium bicarbonate solution to 350 mL of saline solution. The injection was performed twice everyday with one session in the morning and another session in the afternoon. Both patients showed experienced renal colic at the beginning, and the symptom was relieved upon intravenous injection of scopolamine and reducing the drip rate to 30~40 drops/min. No infection was observed in both patients. The follow-up renal ultrasonography or CT scanning showed no trace of stone fragments. In order to prevent the stone recurrence after removing the catheter, patient with hyperuricemia should take allopurinol and 10% potassium citrate, also increase fluid intake to maintain the urine pH in the range of 6.0~6.5. CT scanning is strongly recommended every half year to check the signs of recurrence.
In conclusion, the use of ESWL and sodium bicarbonate dissolution therapy as a combined modality is a safe, efficacious, inexpensive non-invasive treatment for uric acid nephrolithiasis.
Disclosure of conflict of interest
None.
References
- 1.Mattle D, Hess B. Preventive treatment of nephrolithiasis with alkali citrate--a critical review. Urol Res. 2005;33:73–79. doi: 10.1007/s00240-005-0464-8. [DOI] [PubMed] [Google Scholar]
- 2.Li T, Fang Y, Wu J, Zhou X. A novel ureter dilatation method for replacing hydromantic perfusion pump during ureteroscopic lithotripsy in patients with ureteral calculi and ibroepithelial polyps. Int J Clin Exp Med. 2014;7:616–21. [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang BY, Aguilar J, Yang M, Wang P, Li B. Mucinous metaplasia in urothelial tract may be he precancerous lesion of mucinous adenocarcinoma: report of two cases and review of literature. Int J Clin Exp Med. 2014;7:285–289. [PMC free article] [PubMed] [Google Scholar]
- 4.Ghosh T, Sarkar P, Tumer AP. A novel third generation uric acid biosensor using uricase electro-activated with ferrocene on a nafion coated glassy carbon electrode. Bioelectrochemistry. 2014;102:1–9. doi: 10.1016/j.bioelechem.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 5.Cicerello E, Merlo F, Maccatrozzo L. Urinary alkalization for the treatment of uric acid nephrolithiasis. Arch Ital Urol Androl. 2010;82:145–148. [PubMed] [Google Scholar]
- 6.Pejcić T, Marković B, Djurasić L, Maksimović H, Topuzović C, Dzamić Z, Hadzi-Djokić J. The dissolution of multiple renal uric acid stones via percutaneous nephrostomy in the patient with a solitary kidney. Acta Chir Iugosl. 2012;59:93–96. doi: 10.2298/aci1203093p. [DOI] [PubMed] [Google Scholar]
- 7.Mokos I, Pasini J, Hrstić I, Stern-Padovan R, Cacic Z, Knezevic N. Extracorporeal shock wave lithotripsy of impacted radiolucent stone at the right pyeloureteric junction and oral dissolution therapy in a patient with transplanted liver: a case report. Transplant Proc. 2007;39:3533–3535. doi: 10.1016/j.transproceed.2007.09.042. [DOI] [PubMed] [Google Scholar]
- 8.Cruz-Dominguez MP, Cortes DH, Zarate A, Tapia-Gonzalez Mde L, Alvarez-Acosta S, Damasio L, Manuel-Apolinar L. Relationship of ghrelin, acid uric and proinflammatory adipocytokines in different degrees of obesity or diabetes. Int J Clin Exp Med. 2014;7:1435–1441. [PMC free article] [PubMed] [Google Scholar]
- 9.Mokhless IA, Sakr MA, Abdeldaeim HM, Hashad MM. Radiolucent renal stones in children: combined use of shock wave lithotripsy and dissolution therapy. Urology. 2009;73:772–775. doi: 10.1016/j.urology.2008.10.066. [DOI] [PubMed] [Google Scholar]


