Abstract
This study was conducted to investigate the effect of uterine artery embolization for the treatment of hemorrhage following second-trimester labor induction for women with scarred uterus. Two cases of second-trimester abortion were retrospectively reviewed, both of which had a history of caesarean delivery and were complicated by gestational anemia. One was at 18 weeks’ gestation and presented with persistent vaginal bleeding for two months resulting in relatively large area of blood clot in uterine cavity. The other was at 25 weeks’ gestation with partial hydatidiform mole and presented with intermittent vaginal bleeding. Both patients presented with continuous and heavy vaginal bleeding after oral administration of mifepristone for labor induction, with one cervix left unopened, while the other cervix 3 cm left dilatation, yet felt obstructed by pregnant tissue. Both patients were immediately treated with uterine artery embolization (UAE). Both patients presented with alleviated hemorrhage and regular uterine contraction after UAE, followed by smooth induction of labor. No hemorrhage occurred since then during the follow-up. The results suggest that UAE is safe and effective for the treatment of massive hemorrhage of second-trimester abortion in women with scarred uterus. It can reduce time period of labor induction and alleviate hemorrhage, which not only rescues patients but also avoids cesarean sections and retains fertility for the pregnant.
Keywords: Uterine artery embolization (UAE), scarred uterus, second-trimester, abortion, massive hemorrhage
Introduction
There exists great risk in labor induction of second-trimester pregnant with scarred uterus, the failure of which may result in massive hemorrhage and hysterorrhexis or even cesarean section that poses a serious threat to the woman’s physical and mental health. Uterine artery embolization (UAE) is one of the interventions that could achieve good results in management of acute obstetrical hemorrhage. In 2014, two cases of pregnant women with scarred uterus receiving UAE procedure due to massive hemorrhage during second-trimester abortion were reported in our hospital, and we briefly described them as follows.
Materials and methods
Clinical information
Two patients were admitted to our hospital in 2014, with one presenting with recurrent vaginal hemorrhage that was refractory to tocolytic therapy and induction of labor was performed due to rupture of fetal membranes. The other was complicated by partial hydatidiform moles in which large area of grape-like tissues was seen in the uterine cavity (Table 1).
Table 1.
Baseline characteristics of the two cases
| Case 1 | Case 2 | |
|---|---|---|
| Age (years) | 25 | 26 |
| Cesarean delivery (times) | 1 | 1 |
| Abortion (times) | 2 | 1 |
| Gestational weeks | 22 | 26 |
| Hemoglobin level before UAE (g/L) | 93 | 90 |
| Hemoglobin level after UAE (g/L) | 83 | 81 |
| Estimated blood loss (ml) | 800 | 1000 |
| Time span from UAE to regular contraction (hours) | 5 | 1 |
| Time span from UAE to induction of labor (hours) | 16 | 4 |
| Estimated blood loss during abortion (ml) | 100 | 150 |
Case report
Case 1
A 25-year-old female patient was admitted to our hospital due to 18 weeks of amenorrhea and two hours of vaginal bleeding. She presented with slight vaginal bleeding at 50 days and 60 days of amenorrhea, which was eliminated by administration of progesterone and tocolytic therapy. The vaginal bleeding recurred at 11 weeks of amenorrhea, and she was given magnesium sulphate intermittently as a tocolytic agent. Such bleeding aggravated accompanied by abdominal pain two hours before admission. Despite tocolytic magnesium sulfate treatment and hemostasis after admission, the symptom of vaginal bleeding continued. Color doppler ultrasonography showed a viable fetus with biparietal diameter, head and abdominal circumference measuring 49 mm, 187 mm and 177 mm, respectively; posterior placenta with grade one maturity, and the maxium depth of amniotic fluid measuring 34 mm. Ultrasonography also showed a heterogeneous and relatively strong echo with an area of 73 mm × 51 mm on the top of internal cervical os and irregular shape, which was suspected as a blood clot as it presented a liquid echo with poor ultrasound penetration (Figure 1). One day after, the patient complained translucent vaginal discharge followed by light red discharge. Doppler ultrasound demonstrated that the amniotic fluid was reduced to 18 mm in maximum depth; the area of the heterogeneous and relatively strong echo between the bottom of amniotic sac and internal cervical os measured 70 mm × 30 mm. These findings highlighted the high risk of inevitable abortion. Tocolytic therapy was halted and induction of labor was conducted by oral administration of mifepristone every 12 hours, 50 mg a time. After accumulated 150 mg administration, the amount of vaginal bleeding exceeded that of menstrual bleeding, accompanied by irregular uterine contraction. Gynecologic examination suggested a soft cervix, which remained unchanged, and the orifice of cervix was as large as the circumference of a finger-tip. Massive vaginal bleeding continued. With the informed consent of the patient and her relatives, UAE was immediately performed accessed via femoral artery of both groins with contrast agent-enhanced imaging under regional anaesthesia. After UAE, vaginal bleeding was remarkably reduced and the normal frequency of uterine contractions recovered. Ten hours later, a dead infant was induced.
Figure 1.

Findings in color doppler ultrasonography of case 1: a heterogeneous and relatively strong echo with an area of 73.1 mm × 51.8 mm between the bottom of amniotic sac and internal os with irregular shape, indicating a blood clot as it presented a liquid echo with poor ultrasound penetration.
Case 2
A 26-year-old female patient was admitted to our hospital due to of intrauterine pregnancy for 25+6 weeks and diagnosis of partial hydatidiform mole for 2 days. She had intermittent vaginal bleeding from the 40th day of amenorrhea and was orally administered progesterone for tocolytic therapy. However, the symptom did not alleviate. At 25+4 weeks, the 4D color Doppler ultrasonography demonstrated a single viable fetus of breech presentation with biparietal diameter, head and abdominal circumference measuring 58 mm, 222 mm and 209 mm, respectively; the fetus was equal to 24+6 weeks gestation with a posterior placenta grade zero maturity; the fetal heart rate was 149 beats per minute and amniotic fluid index was 74 mm. Heterogeneous echo with an area of 282 mm × 166 mm × 85 mm was detected at the left side of uterine cavity, inside which multiple anechoic honeycomb areas of difference sizes as well as blood flow signals could be detected, with the inferior margin extending to internal cervical os. Still the patient complained of slight vaginal bleeding without abdominal pain. Her serum β subunit of human chorionic gonadotropin (β-HCG) after admission was > 200000 mIU/ml, which was suspected to be a partial hydatidiform mole. Induction of labor was carried out by oral administration of mifepristone tablets (50 mg). Massive vaginal bleeding occurred six hours later. Then UAE was immediately performed accessed via femoral artery of both groins with contrast agent-enhanced ultrasound under regional anesthesia. Methotrexate (25 mg) was administered by transcather intraarterial injection during embolization. The normal frequency of uterine contractions returned back two hours after the UAE procedure. Three hours later, a dead female infant was delivered along with cluster of grape-like tissue with intact placenta. Pathological examination confirmed the diagnosis of partial hydatidiform mole. Immunohistochemically, cell components showed the following immunoreactions: CD34 +, Ki-67 10%, P53 40%, P57 + (Figure 2).
Figure 2.

A demised fetus and plenty of moles were induced from uterus, perceivable vesicle-like tissue with 27 cm × 20 cm × 3 cm in size, of which the largest vesicle was 0.1 cm to 4 cm in diameter. A 15 cm × 9 cm × 2 cm placenta tissue was also included. The pathological findings indicated partial hydatidiform mole, and umbilical cord with mucoid degeneration.
UAE procedure
The right femoral artery was punctured in the inguinal region under regional anesthesia and the supervision of Digital Subtraction Angiography (DSA), COBRA catheter was punctured into the bilateral internal iliac artery, and then negotiated into each uterine artery for enhanced imaging. We firstly performed 500-700 micron diameter sodium alginate microsphere and gelatin sponge particle embolization then switched to gelfoam embolization for arterial trunk when blood flow slowed down and ultimately halted. During embolization, arterial infusion chemotherapy was performed when needed. Arteriography revealed that bilateral uterine arteries were completely embolized. No staining was observed in the uterus or in branches of the external iliac artery served as blood supply for uterus (Figure 3).
Figure 3.
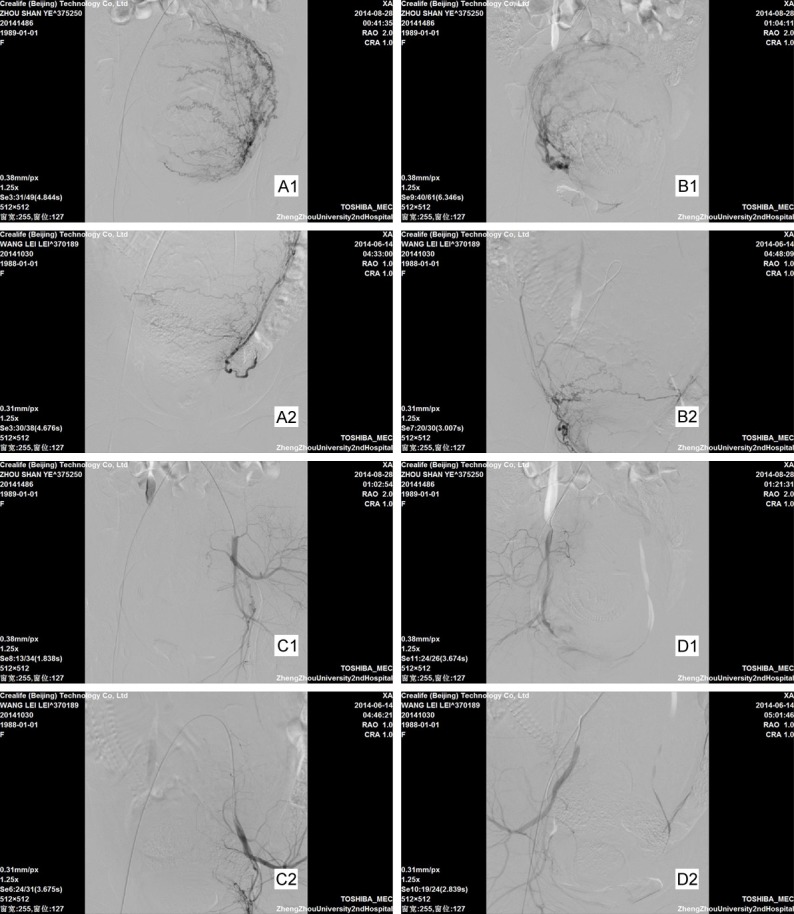
Left (A1) and right (B1) uterine angiography before embolization in case 1; Left (A2) and right (B2) uterine angiography before embolization in case 2. Enlarged and distorted uterine arteries and enlarged uteruses were seen in both cases. Left (C1) and right (D1) uterine angiography after embolization in case 1; Left (C2) and right (D2) uterine angiography after embolization in case 2. The bilateral uterine arteries were completely embolized after UAE in both cases and the other uterine vessels showed no staining.
Evaluation and follow-up of UAE
Successful hemostasis was achieved in both cases, and no recurrent bleeding occurred during follow-up. Both patients were complicated with an increased body temperature with one had reached 39°C. Body temperature reached 37.8°C in case 2 and decreased to normal after expectant treatment. Case 1 had recovered her menstrual cycle and was 12 weeks pregnant and maintained good conditions for conception. A β-HCG level maintained at 200 mIU/ml in case 2 when discharged, and increased one week later. The chest CT scan demonstrated multiple pulmonary metastatic lesions in both lungs. And she was administered with five courses of vincristine, methotrexate and paraplatin for gestational trophoblastic diseases. During the last follow-up, the serum β-HCG level was return to normal and the metastasis in chest disappeared. The patient recovered her menstrual cycle three months after the last course of treatment.
Discussion
Second-trimester is associated with various complications such as high risks of abortion, fetal malformation and other diseases. The delivery of fetus and placenta during induction of labour is similar to that of term delivery, whereas second-trimester labor induction has great risk due to its intrinsic characteristics including: 1. The progestogen secreted from the placenta antagonizes uterine contraction, meanwhile the villus invade the blood vessels. The relatively large placenta would cover the orifice of cervix. Under such circumstances, recurrent abortion or curettage would cause placenta accreta, placental adhesion or low-lying placenta, resulting in massive hemorrhage even when cervix orifice was unopened; 2. The lower uterine segment is taking shape during this period and the cervix is yet to be mature. With thin and filmy scar tissue, the muscle fibers of uterus do not have good elasticity. Therefore, when the uterine contraction becomes strong, the fetus will tend to be delivered from thin tissues, thus hysterorrhexis may occur; 3. Fetal head was larger, which would cause difficulties in curettage that. Adequate cervical dilation was required for vaginal delivery; 4. The decidua is relatively insensitive due to diminished levels of oxytocin and its receptors. Both cases were pathological second-trimester pregnancy with scarred uterus. Both patients had history of induced abortion. Case 1 was observed to have large area of blood clot, fetal membrane rupture and hematoncus beneath placenta, indicating the possibility of placenta separation. Case 2 was diagnosed with partial hydatidiform moles in the second-trimester pregnancy which is a relative rare case. She had an abnormally high β-HCG level, and the moles covered an area larger than the placenta, which was not sufficient to nourish normal fetal development. Therefore, it led to intermittent bleeding and smaller amount of amniotic fluid and high risk of fetal malformation. Case 2 had higher risk since massive hemorrhage occurred during induction of labor. Both cases were administered with mifepristone for induction, while the cervix of case 1 was not open and that of case 2 was opened to 3cm but obstructed by large amount of moles.
Currently, there are various methods regarding inducing labor for second-trimester with scarred uterus, without uniform guidelines, mainly including surgical and drug induction of labor. Surgical procedure includes hysterotomy or caesarean section, which could immediately terminate gestation and control hemorrhage, but produce severe trauma that would deprive the fertility and raise the risk of long-term complication in scarred tissues, particularly for second-trimester pregnancy. The usual practice abroad is cervix dilation combined with uterine curettage or mifepristone combined with misoprostol [1,2]. The practices in China include one or any combination of the following: amnion cavity injection of rivanol, mifepristone and misoprostol, oxytocin induction and water-cyst induction. The advantage of drug induction of labor is that it allows vaginal delivery, though severe hemorrhage might occur and surgical intervention is required if necessary. Mifepristone could antagonize progestogen and glucocorticoid and promote release of prostaglandin; while misoprostol could stimulate the uterus and soften the cervix and is more widely used in induction of labor [3,4]. Both cases in our study were in their reproductive year and had scarred uterus with large area of blood clot and grape-like tissues. The induction by administration of rivanol or oxytocin was improper, and instead, mifepristone and misoprostol were used.
UAE is characterized by fast control of bleeding, minimal invasion and shorter operation time, which has been widely applied in the management of obstetric massive hemorrhage, especially in cases complicated with placenta accrete and previa that can significant reduce cesarean section rate. Previous studies revealed that UAE had achieved an effective rate of control and prevention of bleeding more than 80% [5]. Lia Haddad et al reported a successful case employing UAE to treat massive hemorrhage during induction of labor in second-trimester pregnancy [6]. Wang et al demonstrated that the success rate of UAE procedure was almost 100% in non emergency operations and 88% in emergency operations [7]. The uterine arteries are the major source of blood supply for uterus. However, in pregnancy, the source of blood supply for uterus becomes diverse, a large portion of which are lateral branches and communicating arteries that vary in diameter, location and structure, etc. Therefore, ligature of arterial trunk alone is not adequate for complete blood control. Imaging of blood vessels during UAE enables visualization of blood supply in internal iliac artery, external iliac artery, uterine arterial trunk and lateral branches, thereby facilitating the embolization of blood vessels visually, reducing the blood supply for the uterus and placenta. Gelatin sponge particles, polyvinyl alcohol particles or coils are the three major materials for embolization. By comparison, gelatin sponge particles are more easily degraded, which prevents permanent embolization [8,9]. The chemotherapeutic agents injected via catheters, such as methotrexate and platinum, produced higher regional concentrations that can reduce the side effects of intravenous chemotherapy. Hypoxic and ischemic damage to the uterus is reduced and the fetus may have better tolerance. Then hemostasis can be achieved. Both patients had posterior placenta and were orally administered mifepristone for induction of labour. However, the cervixes were not mature and the internal cervical os were obstructed, resulting in massive hemorrhage. After UAE, the myometrium and endometrium were suffering from ischemia and hypoxia and the release of prostaglandin and endothelin increased, inducing or promoting uterine contraction. For patients complicated with partial hydatidiform moles, compared with caesarean sections, vaginal delivery after UAE not only reduces the activity of trophozoite, but also reduces metastasis through blood vessels and has minimal trauma. The time spans from completion of UAE procedure to regular uterine contraction were five hours and one hour for these two cases, respectively. However, whether UAE can effectively shorten the duration of induced labor remains to be explored.
Reported complications after UAE include: 1. Postembolization syndrome manifested with fever, abdominal pain, nausea, and vomiting etc. It usually occurs within seven days after UAE, which is normal that could be alleviated by expectant treatment, while possibility of infection should be precluded firstly; 2. Vesicoureteral and rectal injury which rarely occurs [10,11]; 3. Disruption of ovary and fertility [12,13], endometrial injury, intrauterine adhesion, premature ovarian failure and amenorrhea, etc. Though evidence is still controversial, in our study, case 1 became pregnant again and case 2 had decreased volume of menstrual fluid, whereas the relationship between UAE and impaired function of ovary or endometrium remains elusive; 4. Others such as bleeding at puncture sites, infection, allergy to contrast agent, vessel injury and embolization, etc.
In summary, UAE is an efficient, safe, reliable and operator-friendly procedure with minimal trauma in treating hemorrhage of second-trimester labor induction for pregnant with scarred uterus, which is highly recommended.
Acknowledgements
This research was supported by Scientific and Technological Key Task Program of Henan Provincial Public Health Department (grant no. 201204037).
Disclosure of conflict of interest
None.
References
- 1.Ashok PW, Templeton A, Wagaarachchi PT, Flett GM. Mid trimester medical termination of pregnancy: a review of 1002 consecutive cases. Contraception. 2004;69:51–58. doi: 10.1016/j.contraception.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 2.Stubblefield PG, Carr-Ellis S, Borgatta L. Methods for induced abortion. Obstet Gynecol. 2004;104:174–185. doi: 10.1097/01.AOG.0000130842.21897.53. [DOI] [PubMed] [Google Scholar]
- 3.Lee VC, Ng EH, Ho PC. Issues in second trimester induced abortion (medical/surgical methods) Best Pract Res Clin Obstet Gynaecol. 2010;24:517–527. doi: 10.1016/j.bpobgyn.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 4.Hapangama D, Neilson JP. Mifepristone for induction of labour. Cochrane Database Syst Rev. 2009;3:CD002865. doi: 10.1002/14651858.CD002865.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jung HN, Shin SW, Choi SJ, Cho SK, Park KB, Park HS, Kang M, Choo SW, Do YS, Choo IW. Uterine artery embolization for emergent management of postpartum hemorrhage associated with placenta accreta. Acta Radiol. 2011;52:638–642. doi: 10.1258/ar.2011.100514. [DOI] [PubMed] [Google Scholar]
- 6.Haddad L, Delli-Bovi L. Uterine artery embolization to treat hemorrhage following second-trimester abortion by dilatation and surgical evacuation. Contraception. 2009;79:452–455. doi: 10.1016/j.contraception.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 7.Wang Z, Chen J, Shi H, Zhou K, Sun H, Li X, Pan J, Zhang X, Liu W, Yang N, Jin Z. Efficacy and safety of embolization in iatrogenic traumatic uterine vascular malformations. Clin Radiol. 2012;67:541–5. doi: 10.1016/j.crad.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 8.Fiori O, Deux JF, Kambale JC, Uzan S, Bougdhene F, Berkane N. Impact of pelvic arterial embolization for intractable postpartum hemorrhage on fertility. Am J Obstet Gynecol. 2009;200:384, e1–e4. doi: 10.1016/j.ajog.2008.11.029. [DOI] [PubMed] [Google Scholar]
- 9.Eriksson LG, Mulic-Lutvica A, Jangland L, Nyman R. Massive postpartum hemorrhage treated with transcatheter arterial embolization: technical aspects and long-term effects on fertility and menstrual cycle. Acta Radiol. 2007;48:635–642. doi: 10.1080/02841850701370683. [DOI] [PubMed] [Google Scholar]
- 10.Ducarme G, Dochez V, Vallon C, Poirier P, Jean MH. Acute rectal ischemia following failed uterine artery embolization and emergency hysterectomy for postpartum hemorrhage. Int J Gynaecol Obstet. 2015;129:81–82. doi: 10.1016/j.ijgo.2014.10.020. [DOI] [PubMed] [Google Scholar]
- 11.El-Shalakany AH, Nasr El-Din MH, Wafa GA, Azzam ME, El-Dorry A. Massive vault necrosiswith bladder fistula afteruterine artery embolisation. BJOG. 2003;110:215–216. [PubMed] [Google Scholar]
- 12.Tan G, Xiang X, Guo W, Zhang B, Chen W, Yang J. Study of the impact of uterine artery embolization (UAE) on endometrial microvessel density (MVD) and angiogenesis. Cardiovasc Intervent Radiol. 2013;36:1079–85. doi: 10.1007/s00270-013-0599-x. [DOI] [PubMed] [Google Scholar]
- 13.Vendittelli F, Savary D, Storme B, Rieud V, Chabrote P, Charpyf C, Lémerya D, Jacquetina B. Ovarian thrombosis and uterine synechiae after arterial embolization for a late postpartum haemorrhage. Case Reports in Women’s Health. 2015;5:1–4. doi: 10.1016/j.crwh.2014.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]


