Abstract
T-cell prolymphocytic leukemia (T-PLL) is an aggressive mature T cell neoplasm that typically involves peripheral blood, bone marrow, lymph nodes and spleen. It is a rare disease that comprises 2-5% of mature lymphocytic leukemia in adults. Here we present a T-PLL patient with CNS involvement. A 74-year-old man admitted to a hospital in April 2014 with vomiting. He was diagnosed as chronic lymphocytic leukemia (CLL) and R-CVP (Rituximab, cyclophosphamide, vincristine and prednisolone) chemotherapy protocol was started. After the first two cycles of chemotherapy, the patient’s mental functions improved. However after the 3rd cycle of chemotherapy was given in July 2014 the general situation of the patient deteriorated and ptosis of the left eye and facial paralysis developed. Then the patient was referred to our medical center. An MR of the brain revealed linear contrast enhancement around the bilateral 3rd, 7th and 8th cranial nerves which indicated cranial involvement by the lymphoproliferative process (Figure 1). Cerebrospinal fluid cytological examination confirmed the diagnosis. Based on these and bone marrow aspiration and biopsy findings a diagnosis of T-PLL was rendered (Figure 3). In September 2014 the patient died suddenly due to a cardiac arrest. Differential diagnosis is very important in T-PLL. Both T-PLL and chronic lymphocytic leukemia (CLL) may present with splenomegaly and lymphocytosis as well as circulating prolymphocytes in blood. Typical CLL cells are like mature lymphocytes with dense nucleus and aggregated chromatin. To conclude, CNS involvement in T-PLL is a rare finding and differential diagnosis of T-PLL is very important.
Keywords: T-cell prolymphocytic leukemia, central nervous system involvement
Introduction
T-cell prolymphocytic leukemia (T-PLL) is an aggressive mature T cell neoplasm that typically involves peripheral blood, bone marrow, lymph nodes and spleen. It is a very rare disease that comprises 2-5% percent of mature lymphocytic leukemia in adults [1]. Most patients with T-PLL present with leukocytosis, hepatosplenomegaly, and generalized lymphadenopathy. On the other hand, involvement of the central nervous system (CNS) is very rarely reported mostly as an autopsy finding [2-6]. Herein, we present a T-PLL patient with CNS involvement.
Case report
A 74-year-old man applied to a hospital in April 2014 with vomiting. WBC was around 200.000/µl on admission. Within a few days WBC increased to 480.000/µl so leukapheresis was performed. Splenomegaly and intraabdominal lymphadenopathies were observed on abdominal ultrasonography. Mental functions of the patient deteriorated and he had hallucinations. He was considered to be chronic lymphocytic leukemia (CLL) and R-CVP (Rituximab, cyclophosphamide, vincristine and prednisolone) chemotherapy protocol was started. After the first two cycles of chemotherapy, the patient’s mental functions improved. However after the 3rd cycle of chemotherapy was given in July 2014 the general situation of the patient deteriorated and ptosis of the left eye and facial paralysis developed. Then the patient was referred to our medical center. Within a few days, ptosis of the other eye and restriction of the bilateral eye movements was added to the clinical picture. Electromyography revealed mixed polyneuropathy especially in lower extremities. An MR of the brain revealed linear contrast enhancement around the bilateral 3rd, 7th and 8th cranial nerves which indicated cranial involvement by the lymphoproliferative process (Figure 1). Cerebrospinal fluid cytological examination confirmed the diagnosis (Figure 2). In flow cytometry analysis of the peripheral blood, the neoplastic cells were positive for T cell markers (CD2, CD3, CD4, CD5, CD7); and negative for B-cell associated markers (CD19, CD20, CD22, CD23). Based on these and bone marrow aspiration and biopsy findings a diagnosis of T-PLL was rendered (Figure 3). In September 2014 the patient died suddenly due to cardiac arrest.
Figure 1.
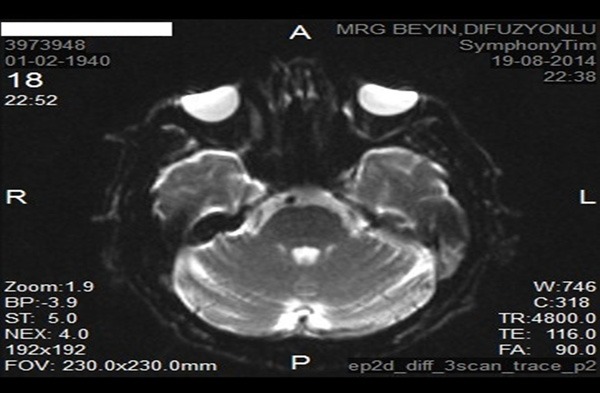
MR screen image.
Figure 2.
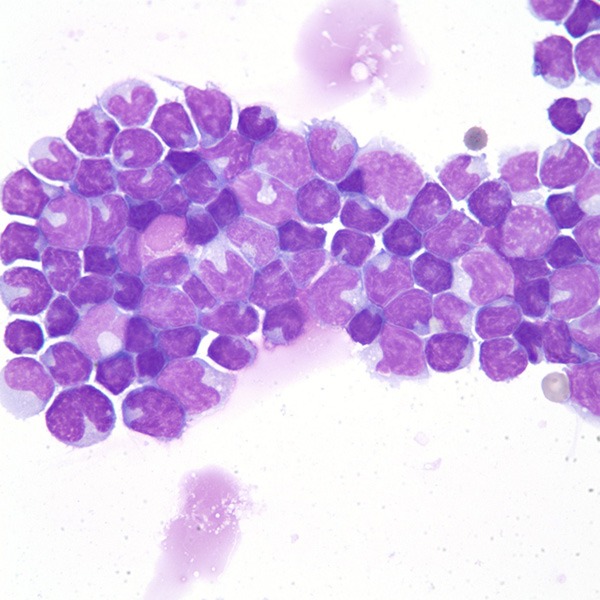
Cerebrospinal fluid cytology.
Figure 3.
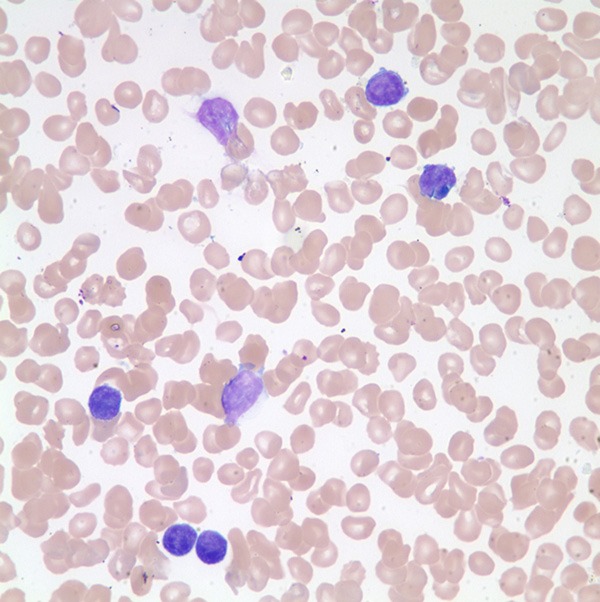
Bone marrow aspiration.
Discussion
Herein we report a rare disease with an unusual clinical manifestation. T-PLL is a very aggressive disease with a median survival of less than 1 year [2]. In only very few cases an indolent clinical course has been reported [7]. Our case survived only 5 months after the symptoms had developed. It is known that in T-PLL leucocyte count is usually above 200.000/µl [1]. Similarly our case hada WBC that reached 480000/µl. Most T-PLL patients have hepatosplenomegaly and generalized lymphadenopathies [1]. Our case had splenomegaly and intraabdominal lymphadenopathies as well. However invasion of the CNS by T-PLL is extremely rare. There are different clinical manifestations reported in leukemic meningitis but most cases with CNS involvement are asymptomatic and diagnosis is usually made by autopsy [8]. However as described, our patient had a symptomatic CNS disease. CNS involvement of T-PLL is considered as incurable and had very poor prognosis. Also differential diagnosis is very important in T-PLL. Both T-PLL and chronic lymphocytic leukemia (CLL) may present with splenomegaly and lymphocytosis as well as circulating prolymphocytes in blood. Typical CLL cells are like mature lymphocytes with dense nucleus and aggregated chromatin. The most important difference is that CLL expresses B cell associated antigens (CD19, 20, 23) and T cell antigen CD5; T-PLL does not express any B cell associated antigens. To conclude, CNS involvement in T-PLL is a very rare finding and differential diagnosis of T-PLL is very important.
Disclosure of conflict of interest
None.
References
- 1.Swerdlow SH, Campo E, Harris NL, editors. World Health Organization Classification of Tumours of Haematopoietic and Lymphoid Tissues. Lyon: IARC Press; 2008. [Google Scholar]
- 2.Garderet L, Bittencourt H, Kaliski A, Daniel M, Ribaud P, Socié G, Gluckman E. Treatment of T-prolymphocytic leukemia with nonmyeloablative allogeneicstem cell transplantation. Eur J Haematol. 2001;66:137–9. doi: 10.1034/j.1600-0609.2001.00377.x. [DOI] [PubMed] [Google Scholar]
- 3.Kuwabara H, Kanamori H, Takasaki H, Takayabayashi M, Yamaji S, Tomita N, Fujimaki K, Fujisawa S, Ishigatsubo Y. Involvement of central nervous system in prolymphocytoid transformation of chronic lymphocytic leukemia. Leuk Lymphoma. 2003;44:1235–1237. doi: 10.1080/1042819031000079177. [DOI] [PubMed] [Google Scholar]
- 4.Pamuk GE, Puyan FO, Unlu E, Oztürk E, Demir M. The first case of de novo B-cell prolymphocytic leukemia with central nervous system involvement: description of an unreported complication. Leuk Res. 2009;33:864–867. doi: 10.1016/j.leukres.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 5.Wang ML, Shih LY, Dunn P, Kuo MC. Meningeal involvement in B-cell chronic lymphocytic leukemia: report of twocases. J Formos Med Assoc. 2000;99:775–778. [PubMed] [Google Scholar]
- 6.Brito-Babapulle F, Huang D, Lavender P, Galton D, Catovsky D. Regression of intracerebral lesions in T prolymphocytic leukemia treated with intravenous deoxycoformycin. Eur J Haematol. 1988;40:185–187. doi: 10.1111/j.1600-0609.1988.tb00819.x. [DOI] [PubMed] [Google Scholar]
- 7.Garand R, Goasguen J, Brizard A, Buisine J, Charpentier A, Claisse JF, Duchayne E, Lagrange M, Segonds C, Troussard X, Flandrin G. Indolentcourse as a relativelyfrequentpresentation in T-prolymphocyticleukaemia. Groupe Françaisd' Hématologie Cellulaire. Br J Haematol. 1998;103:488–94. doi: 10.1046/j.1365-2141.1998.00977.x. [DOI] [PubMed] [Google Scholar]
- 8.Denier C, Tertian G, Ribrag V, Lozeron P, Bilhou-Nabera C, Lazure T, Abbed K, Lacroix C, Adams D. Multifocal deficits due to leukemic meningoradiculitis in chronic lymphocytic leukemia. J Neurol Sci. 2009;277:130–2. doi: 10.1016/j.jns.2008.11.003. [DOI] [PubMed] [Google Scholar]


