Abstract
Only a few cases with unilateral internuclear ophthalmoplegia have been reported presenting vertical nystagmus, and few of them provides convincing evidence for the paramedian tract neuron to be a vertical neural integrator. We report a patient who suffered from confined dorsal mid-upper pontine infarction showing unilateral internuclear ophthalmoplegia with upbeat nystagmus in primary position. This case possibly provide evidence that paramedian tract neurons may act as a vertical neural integrator in human.
Keywords: Internuclear ophthalmoplegia, nystagmus, stroke, paramedian tract neuron
Introduction
Internuclear ophthalmoplegia (INO) occurs in a complete lesion of the medial longitudinal fasciculus (MLF). It refers to the condition in which the ipsilateral eye fails to adduct when the patient looks to the opposite side. To our best knowledge, only a few cases have been reported presenting vertical nystagmus [1]. Herein, we reported a patient who suffered from limited pontine infarction showing unilateral INO with upbeat nystagmus (UBN) in primary position. And this may prove that paramedian tract (PMT) neurons probably act as a neural integrator for vertical gaze holding in human.
Case presentation
A 51-year-old woman was admitted 4 days after a sudden onset of vertigo, double vision and vomiting. There was no history of limb paralysis, dysesthesia, visual loss, dysarthria and dysphagia. Her past medical history and life history were unremarkable. General examinations revealed normal blood pressure (121/84 mmHg) and no other abnormal findings. Neurological examination revealed an adduction deficit in the right eye (Figure 1) and, as expected, horizontal nystagmus in the left eye on leftward gaze. Noteworthily, bilateral upbeat nystagmus was observed when the eyes were in the central position, and increased on downward gaze. Neither skew deviation nor head tilting was noted. The rest of the neurological examinations were unremarkable. Laboratory findings, including fasting plasma glucose and blood lipid levels, were normal. The diffusion-weighted image and fluid-attenuated inversion recovery image demonstrated a lesion around the MLF at the dorsal upper pons (Figure 2). Her upbeat nystagmus disappeared when she was discharged 11 days after symptom onset. At that time, the right INO and abduction nystagmus in left eye were still present.
Figure 1.

Adduction deficit in the right eye on leftward gaze.
Figure 2.
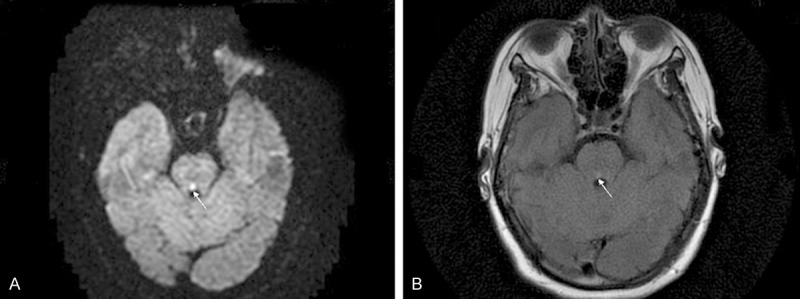
The diffusion-weighted image (A) and fluid-attenuated inversion recovery image (B) demonstrated a lesion around the right medial longitudinal fasciculus at the dorsal upper pons (arrows).
Discussion
Pontine lesions may result in horizontal eye movement disorders: INO, paramedian pontine reticular formation (PPRF) syndrome, abduction paralysis or one-and-a-half syndrome. PPRF at the level of abducens nucleus serves as the center for horizontal gaze. MLF which lies in the medial tegmentum of the brainstem connects the third and sixth nerve nuclei and connects both these nuclei with the vestibular nuclei. Via the MLF, conjugate lateral gaze under instruction of PPRF is achieved by the simultaneous innervation of the ipsilateral lateral rectus and the contralateral medial rectus. Interruption of the MLF between the midpons and the oculomotor nucleus causes a discrete adduction deficit of the eye ipsilateral to the MLF lesion, a sign called INO. Abduction nystagmus occurs in the contralesional eye during horizontal gaze. It has been hypothesized to reflect impaired inhibition in the medial rectus muscle of the abducting eye [2].
UBN is attributed to bilateral lesions of the upward vestibulo-ocular reflex (VOR) pathway. In cases of UBN due to pontine damage, the lesions are located in the ventral tegmentum and/or the posterior basis pontis, at the upper pons level. These lesions could destroy MLF, ventral tegmental tract (VTT) or PMT cell groups that participate in oculomotor integration [1,3,4]. The interstitial nucleus of cajal (INC) situated between the red nucleus and the superior colliculus is the neural integrator for vertical gaze holding. It receives disynaptic potentials through the ipsilateral and contralateral MLF [5]. Lesions of the MLF, if bilateral, would disturb the function of this vertical integrator. In most previous cases suffered from pontine damage with UBN, lesions are usually large and bilateral [3], because vertical gaze holding may be preserved in unilateral MLF lesion. Thus, unilateral INO observed in our patient might exclude the possibility of MLF as a candidate structure for the UBN. Lee SC et al. had reported a patient that was very similar to ours and attributed the UBN to the damage of the decussation of the VTT. This decussation locates in the posterior part of the basis pontis at the level slightly above the midpons [6,7]. A relatively small unilateral paramedian lesion at the upper pons, probably involving the VTT decussation, could interupt bilateral upward VOR pathway and result in UBN. However, the pontine lesion demonstrated on the magnetic resonance imaging seems smaller in our patient than theirs. It is confined to the dorsal pontis rather than extending to the ventral tegmentum. Thus, there is little chance for the VTT decussation to be involved. Lesion in PMT cell groups may be the probable cause for UBN in our patient.
PMT cell groups scatter along the midline of the pons and medulla [8], very near to the MLF. They receive inputs from major eye movement-related structures including INC, and project to the cerebellum to provide vestibular and eye movement signals that are essential for velocity-to-position integration [4,9]. Previous report showed a case with hemorrhagic lesion within the bilateral paramedian pons. Considering the unilateral INO in this patient, the authors attributed the UBN to the PMT cells damage [9]. Nevertheless, the lesion diagnosed by the magnetic resonance imaging was so large that the ventral tegmentum had a great likelihood to be involved. Thus, the possibility of VTT impairment as a cause should not be excluded. Our patient, manifested with unilateral INO and a small, limited lesion confined to the MLF territory, may present the UBN as a result of the damage to the PMT cells instead of bilateral MLF or VTT.
In conclusion, clinical findings of our patient may have proved the importance of PMT cells in integrating vertical gaze holding.
Acknowledgements
Supported by grants from the Natural Science Foundation of Shandong Province (No. ZR2010HM101) and the Science and Technology Develop Project of Jinan (No. 201202053).
Disclosure of conflict of interest
None.
References
- 1.Lee SC, Lee SH, Lee KY, Lee YJ, Koh SH. Transient upbeat nystagmus due to unilateral focal pontine infarction. J Clin Neurosci. 2009;16:563–565. doi: 10.1016/j.jocn.2008.05.027. [DOI] [PubMed] [Google Scholar]
- 2.Srivastava AK, Tripathi M, Gaikwad SB, Padma MV, Jain S. Internuclear ophthalmoplegia and torsional nystagmus: an MRI correlate. Neurol India. 2003;51:271–272. [PubMed] [Google Scholar]
- 3.Ranalli PJ, Sharpe JA. Vertical vestibulo-ocular reflex, smooth pursuit and eye-head tracking dysfunction in internuclear ophthalmoplegia. Brain. 1988;111:1299–1317. doi: 10.1093/brain/111.6.1299. [DOI] [PubMed] [Google Scholar]
- 4.Nakamagoe K, Iwamoto Y, Yoshida K. Evidence for brainstem structures participating in oculomotor integration. Science. 2000;288:857–859. doi: 10.1126/science.288.5467.857. [DOI] [PubMed] [Google Scholar]
- 5.King WM, Precht W, Dieringer N. Synaptic organization of frontal eye field and vestibular afferents to interstitial nucleus of Cajal in the cat. J Neurophysiol. 1980;43:912–928. doi: 10.1152/jn.1980.43.4.912. [DOI] [PubMed] [Google Scholar]
- 6.Pierrot-Deseilligny C, Milea D. Vertical nystagmus: clinical facts and hypotheses. Brain. 2005;128:1237–1246. doi: 10.1093/brain/awh532. [DOI] [PubMed] [Google Scholar]
- 7.Pierrot-Deseilligny C, Milea D, Sirmai J, Papeix C, Rivaud-Pechoux S. Upbeat nystagmus due to a small pontine lesion: evidence for the existence of a crossing ventral tegmental tract. Eur Neurol. 2005;54:186–190. doi: 10.1159/000090295. [DOI] [PubMed] [Google Scholar]
- 8.Buttner-Ennever JA, Horn AK. Pathways from cell groups of the paramedian tracts to the floccular region. Ann N Y Acad Sci. 1996;781:532–540. doi: 10.1111/j.1749-6632.1996.tb15726.x. [DOI] [PubMed] [Google Scholar]
- 9.Lee H, Yi HA, Kim HA. Do the paramedian tract neurons in pons take a role as a vertical neural integrator in humans? J Neurol Sci. 2012;321:107–110. doi: 10.1016/j.jns.2012.07.039. [DOI] [PubMed] [Google Scholar]


