Abstract
Objective: Uterine artery embolization (UAE) has been commonly used for uterine myoma with satisfactory effects, but the pain during and following the procedure with an occurrence rate in 100%. The aim of this study was to observe the effects of intermittent injection with super-low pressure on pain control during the UAE for uterine myoma. Methods: 67 subjects were divided into 2 groups with 47 in-group A and 20 in group B. A underwent UAE with the intermittent injection at super-low pressure, while B underwent routine UAE. Pain was assessed according to WHO analgesic ladder. Meanwhile, all were scored with the visual analogue scale (VAS). Results: The numbers of first, second and third step analgesic user in Group A were 21, 18 and 6, respectively, with 2 non-analgesic users, while in Group B were 4, 6 and 10, respectively without non-analgesic user (chi-square = 7.043, P = 0.008). VAS showed good pain control in 23 cases, satisfactory in 18 and poor in 6 in Group A, while in Group B, were 4, 8 and 8, respectively (chi-square = 7.329, P = 0.007). Mean follow-up was 16.5 months (range, 6-32 months). The abnormal menstruation was improved and the ultrasound examination 6 months later demonstrated a significant decrease in the diameter of myoma (from 6.65 ± 2.40 cm to 5.22 ± 1.86 cm, t = 3.186, P = 0.002). Conclusion: The application of intermittent injection with super-low pressure during UAE can decrease and possibly eliminate post-operative pain. But the procedure time was increased.
Keywords: Polyvinyl acetate, super-low pressure, uterine artery embolization, uterine myoma
Introduction
Recently, the uterine artery embolization (UAE) has been commonly used for uterine myoma with satisfactory therapeutic effects [1-6]. So far, the major side effect of UAE that has been reported was serious, or even severe long-term pain during and following the procedure with an occurrence rate in 100% of cases [7-11]. Previous reports focused on the postoperative pain control with few attempts to prevent or reduce the extent of pain during the procedure. Pain managements include oral analgesia with a combination of a NSAID (nonsteroidal anti-inflammatory drug) and an opioid, morphine intravenous patient-controlled analgesia (IVPCA), thoracic epidural analgesia, Superior hypogastric nerve block [12-15] some authors even advocated performing UAE under general anesthesia [16]. In our practice, we realized that the embolic agent injection speed might affect the degree of the postoperative pain. Thus we tried to reduce, or even eliminate the postoperative pain through controlling the embolic agent injection speed during UAE and obtained good effects on pain control.
Subjects and methods
Clinical data
This is a prospective study performed during the period from 2009-2012. UAE was performed on 67 cases with uterine myoma that had been diagnosed by both the gynecologic examination and radiographic imaging (ultrasound examination, or CT, MRI scanning). The age ranged 22-46 years with a mean of 35.8 years. Among the subjects, 55 suffered from intramural myoma, 9 with submucous myoma and 3 with subserous myoma. The tumor diameter ranged 2.2-14.3 cm, with a mean of 6.7 cm. All cases complained abnormal menstruation before UAE, including abnormal menstrual volume or cycle and painful menstruation. All the subjects were divided into 2 groups with 47 in group A and 20 in group B. The age, myoma type and size had no significant differences between the two groups. This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Nanfang Hospital, Southern Medical University. Written informed consent was obtained from all participants.
UAE methods
The interventional protocol was approved by our Hospital Ethics Committee. Written informed consent was obtained from all the patients before the procedure. The UAE procedure was performed 3-7 days following menstruation. After the puncture of the right femoral artery using Seldinger technique, a 4 F or 5 F Cobra catheter (Terumo, Japan) was used to select the bilateral internal iliac arteries sequentially, then the catheterization of both uterine arteries were completed by 3 F mico-catheter (Terumo, Japan) for angiography to determine the blood supply of the uterus and myoma. The embolization was performed with embosphere (500-700 um, Biosphere Medical, Inc, MA). The dose depended on the size and blood supply of the myoma. All UAE procedures were completed by 3 professional physicians (over 10 years interventional radiology experience).
Injection speed control during the operation
Group A was for the recent treatment. The uterine artery embolization was adopted with intermittent injection at a super-low pressure, which was different from the routine method of low-pressure flow control. The characteristics of the adopted method were: 1) the super-low pressure, namely the pressure for PVA (Polyvinyl Acetate) injection was as low as possible to just push the embolic agent out the catheter; 2) intermittent, namely after the embolic agent was completely into the focus by the fluoroscopic observation, the next injection was carried out; 3) the progressively decreased injection dose, namely the initial injection of comparatively larger dose and then decreased progressively, especially in the terminal stage of injection.
Group B was for the early-stage treatment. The PVA was injected routinely with low-pressure flow control. That was to inject the PVA through the uterine arteries in the pulsed-wave mode under the fluoroscopic monitor. The speed criteria were without the retrograding regurgitation.
Evaluation of the postoperative pain
The self-related pain duration of each subject was recorded after discharge. The rank of the analgesic user was determined according to WHO analgesic ladder. The users who had used the third step analgesic were considered with the intense pain, the second step with the median pain and the first step with the light pain (e.g. the first step is to use mezolin or aspirin, the second step is to use tramadol hydrochloride sustained release tablets and the third step is to use morphine sulfate tablets). Meanwhile, the subjects in both groups received the visual analogue scale (VAS), with which the subjects had to move the sign (0-100, 0 as without pain and 100 as the intense pain) to signify the pain severity and the overall mental impact of the pain. The detailed criteria were as the follows: 1) 0 meant no pain when turning the body over with coughing; 2) 10 meant no pain in quiet supine lying and with pain when turning the body over with coughing; 3) 20 meant with pain when coughing but no pain when deeply breathing; 4) 30 meant no pain when quiet supine lying but pain when coughing and deeply breathing; 5) 40 meant intermittent pain when lying quiet and supine; 6) 50 meant continuous pain when lying quiet and supine; 7) 60 meant intense pain when lying quiet and supine; 8) 70 meant obvious pain; 9) 80 meant the unbearable continuous pain and overall sweating; 10) 90-100 meant unbearable intense pain. In that, less than 30 VAS score meant good, 30-50 VAS score satisfactory and more than 50 meant poor.
Following-up
All the subjects underwent a follow-up pelvic ultrasound 6 months after the operation to re-examine the changes of the uterine myoma. The symptomatic changes were also recorded. The follow-up was conducted for 6-32 months, with a mean of 16.5 months.
Statistical analysis
SPSS version 13.0 software was achieved for this term and a P value < 0.05 was considered statistically significant.
Results
Postoperation pain
All UAEs were completed successfully without complications. The postoperative pain occurred in a few minutes to 1d after the operation. The numbers of first, second and third step analgesic user in Group A were 21, 18 and 6, respectively, with 2 non-analgesic users, while in Group B were 4, 6 and 10, respectively without non-analgesic user (chi-square = 7.043, P = 0.008, Kruskal-Wallis T test) (Table 1). In group A, VAS showed good pain control in 23 cases, satisfactory in 18 and poor in 6, while in Group B, were 4, 8 and 8, respectively (chi-square = 7.329, P = 0.007, Kruskal-Wallis T test) (Table 2).
Table 1.
Ranks of the analgesic use among postoperative patients of both groups
| Group | First step (case) | Second step (case) | Third step (case) | Mean rank | chi-square | p value |
|---|---|---|---|---|---|---|
| A | 21 | 18 | 6 | 30.13 | 7.043 | 0.008 |
| B | 4 | 6 | 10 | 43.10 |
Table 2.
The VAS grade of both groups
| Group | Good (case) | Satisfactory (case) | Poor (case) | Mean rank | chi-square | p value |
|---|---|---|---|---|---|---|
| A | 23 | 18 | 6 | 30.09 | 7.329 | 0.007 |
| B | 4 | 8 | 8 | 43.20 |
Comparison of the therapeutic effectiveness
During the follow-up, the abnormal menstruation was improved or relieved in all cases. The 6 months ultrasound re-examination demonstrated a significant decrease in the diameter of myoma (from 6.65 ± 2.40 cm to 5.22 ± 1.86 cm, t = 3.186, P = 0.002, paired t test). There was no statistically significant difference in the diameters between the control and the experimental group (F = 134.615, P = 0.000, Analysis of Covariance).
Discussion
In 1994, UAE was firstly reported in the treatment of the uterine myoma [17]. Pain is a common side effect of UAE for leiomyomata [1,18-20]. According to our experience, the post-procedural pain is likely due to the partial tissue ischemia of the uterus and pelvis. The severity and duration of this pain is mainly due to of the ischemic range, especially the pelvic tissues [2,8,21,22]. The topography indicates that the pelvic organs, including the uterine body, ovary, cervix and bladder etc, are collected by extensive capillary networks. It can be observed from the preoperative arteriogram that with the increase of the injected contrast agent within the unit time, there is only uterine artery angiogram at first, then the retrograde showing of the periuterine arteries (Figure 1). Therefore, how to eliminate non-target artery embolization of the pelvic non-target organ is the key to the pain control post UAE.
Figure 1.
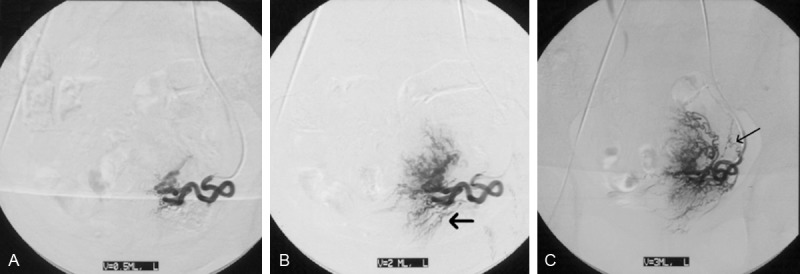
Catheter was placed in the same location of left uterine artery and the images were gained 2 s after the injection, with three injection speeds of 0.5 ml/s (A), 2 ml/s (B) and 3 ml/s (C), respectively. The injection pressures are the same of 300 psi. The higher injection speed is, the more arteries around are. The cervical branch (arrow in B) and ovarian branch (C).
Commonly, 4 F or 5 F catheters are firstly used in UAE followed by micro-catheter, which almostly occlude the uterine arteries with few blood flows. In such conditions, if the injection pressure exceeding the pressure of the capillary network, the embolic agent would flow from the uterine arteries (high pressure area) to the lateral branch of the surrounding organ (low pressure area). This situation would result in the retrograde embolization of non-target organs. But if the injection pressure were low enough, the pressure of the uterine arteries would be lower than that of lateral branch of the surrounding organ. Accordingly, the superlow pressure injection was developed.
The key points of intermittent injection with super-low pressure include the followings: 1) The injection pressure was as low as possible to just push the embolic agents out of the catheter, then be almost pushed into the uterus and myomas by the remaining blood flow of the uterine artery and the blood flow of the lateral branch, since the surrounding lateral blood vessels network was in high pressure area; 2) The injected dose of the embolic agent should be gradually decreased. With the increase of the drug deposit on the uterus and myoma vascular bed, the dose should be gradually decreased possibly to reduce the risk of non-target embolization.
Therefore, the intermittent injection with super-low pressure can eliminate non-target embolization and reduce pain and analgesia requirements.
Acknowledgements
This study was supported by Science and Technology Planning Project of Guangdong Province, China (2012B010200027); The key Technologies R&D Program of Guangzhou, China and the Presidential Foundation of the Nanfang Hospital, Southern Medical University, Guangzhou, China (No. 2011B006).
Disclosure of conflict of interest
None.
References
- 1.Hirst A, Dutton S, Wu O, Briggs A, Edwards C, Waldenmaier L, Maresh M, Nicholson A, McPherson K. A multi-centre retrospective cohort study comparing the efficacy, safety and cost-effectiveness of hysterectomy and uterine artery embolisation for the treatment of symptomatic uterine fibroids. The HOPEFUL study. Health Technol Assess. 2008;12:1–248. doi: 10.3310/hta12050. [DOI] [PubMed] [Google Scholar]
- 2.Kim MD, Lee HS, Lee MH, Kim HJ, Cho JH, Cha SH. Long-term results of symptomatic fibroids treated with uterine artery embolization: in conjunction with MR evaluation. Eur J Radiol. 2010;73:339–344. doi: 10.1016/j.ejrad.2008.10.040. [DOI] [PubMed] [Google Scholar]
- 3.Narayan A, Lee AS, Kuo GP, Powe N, Kim HS. Uterine artery embolization versus abdominal myomectomy: a long-term clinical outcome comparison. J Vasc Interv Radiol. 2010;21:1011–1017. doi: 10.1016/j.jvir.2010.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Popovic M, Berzaczy D, Puchner S, Zadina A, Lammer J, Bucek RA. Long-term quality of life assessment among patients undergoing uterine fibroid embolization. AJR Am J Roentgenol. 2009;193:267–271. doi: 10.2214/AJR.08.1841. [DOI] [PubMed] [Google Scholar]
- 5.Poulsen B, Munk T, Ravn P. Long-term follow up after uterine artery embolization for symptomatic uterine leiomyomas. Acta Obstet Gynecol Scand. 2011;90:1281–1283. doi: 10.1111/j.1600-0412.2011.01229.x. [DOI] [PubMed] [Google Scholar]
- 6.Stokes LS, Wallace MJ, Godwin RB, Kundu S, Cardella JF Society of Interventional Radiology Standards of Practice Committee. Quality improvement guidelines for uterine artery embolization for symptomatic leiomyomas. J Vasc Interv Radiol. 2010;21:1153–1163. doi: 10.1016/j.jvir.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 7.Andersen PE, Lund N, Justesen P, Munk T, Elle B, Floridon C. Uterine artery embolization of symptomatic uterine fibroid. Initial success and short-term results. Acta Radiol. 2001;42:234–238. [PubMed] [Google Scholar]
- 8.Kim SY, Chang CH, Lee JS, Kim YJ, Kim MD, Han DW. Comparison of the efficacy of dexmedetomidine plus fentanyl patient-controlled analgesia with fentanyl patient-controlled analgesia for pain control in uterine artery embolization for symptomatic fibroid tumors or adenomyosis: a prospective, randomized study. J Vasc Interv Radiol. 2013;24:779–786. doi: 10.1016/j.jvir.2013.02.034. [DOI] [PubMed] [Google Scholar]
- 9.Martin J, Bhanot K, Athreya S. Complications and reinterventions in uterine artery embolization for symptomaticuterine fibroids: a literature review and meta analysis. Cardiovasc Intervent Radiol. 2013;36:395–402. doi: 10.1007/s00270-012-0505-y. [DOI] [PubMed] [Google Scholar]
- 10.Stampfl U, Radeleff B, Sommer C, Stampfl S, Dahlke A, Bellemann N, Kauczor HU, Richter GM. Midterm results of uterine artery embolization using narrow-size calibrated embozene microspheres. Cardiovasc Intervent Radiol. 2011;34:295–305. doi: 10.1007/s00270-010-9986-8. [DOI] [PubMed] [Google Scholar]
- 11.van der Kooij SM, Moolenaar LM, Ankum WM, Reekers JA, Mol BW, Hehenkamp WJ. Epidural analgesia versus patient-controlled analgesia for pain relief in uterine artery embolization for uterine fibroids: a decision analysis. Cardiovasc Intervent Radiol. 2013;36:1514–1520. doi: 10.1007/s00270-013-0607-1. [DOI] [PubMed] [Google Scholar]
- 12.Lampmann LE, Lohle PN, Smeets A, Boekkooi PF, Vervest H, van Oirschot CM, Bremer RC. Pain Management During Uterine Artery Embolization for Symptomatic Uterine Fibroids. Cardiovasc Intervent Radiol. 2007;30:809–811. doi: 10.1007/s00270-007-9069-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nagao T, Ohwada T, Kitazono M, Ohshima K, Shimizu H, Katayama M. Thoracic epidural analgesia is effective in perioperative pain relief for uterine artery embolization. Masui. 2005;54:156–159. [PubMed] [Google Scholar]
- 14.Rasuli P, Jolly EE, Hammond I, French GJ, Preston R, Goulet S, Hamilton L, Tabib M. Superior hypogastric nerve block for pain control in outpatient uterine artery embolization. J Vasc Interv Radiol. 2004;15:1423–1429. doi: 10.1097/01.RVI.0000137406.09852.A4. [DOI] [PubMed] [Google Scholar]
- 15.Ryan JM, Gainey M, Glasson J, Doherty J, Smith TP. Simplified pain-control protocol after uterine artery embolization. Radiology. 2002;224:610–1. doi: 10.1148/radiol.2242011954. [DOI] [PubMed] [Google Scholar]
- 16.Brunereau L, Herbreteau D, Gallas S, Cottier JP, Lebrun JL, Tranquart F, Fauchier F, Body G, Rouleau P. Uterine artery embolization in the primary treatment of uterine leiomyomas: technical features and prospective follow-up with clinical and sonographic examinations in 58 patients. AJR Am J Roentgenol. 2000;175:1267–1272. doi: 10.2214/ajr.175.5.1751267. [DOI] [PubMed] [Google Scholar]
- 17.Ravina JH, Herbreteau D, Ciraru-Vigneron N, Bouret JM, Houdart E, Aymard A, Merland JJ. Arterial embolisation to treat uterine myomata. Lancet. 1995;346:671–672. doi: 10.1016/s0140-6736(95)92282-2. [DOI] [PubMed] [Google Scholar]
- 18.Carrillo TC. Uterine Artery Embolization in the Management of Symptomatic Uterine Fibroids: An Overview of Complications and Follow-up. Semin Intervent Radiol. 2008;25:378–386. doi: 10.1055/s-0028-1102997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kahn V, Pelage JP, Marret H. Uterine artery embolization for myomas treatment. Presse Med. 2013;42:1127–1132. doi: 10.1016/j.lpm.2013.02.322. [DOI] [PubMed] [Google Scholar]
- 20.Liang E, Brown B, Kirsop R, Stewart P, Stuart A. Efficacy of uterine artery embolisation for treatment of symptomatic fibroids and adenomyosis-an interim report on an Australian experience. Aust N Z J Obstet Gynaecol. 2012;52:106–112. doi: 10.1111/j.1479-828X.2011.01399.x. [DOI] [PubMed] [Google Scholar]
- 21.Helal A, Mashaly Ael-M, Amer T. Uterine artery occlusion for treatment of symptomatic uterine myomas. JSLS. 2010;14:386–390. doi: 10.4293/108680810X12924466007403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jha RC, Ascher SM, Imaoka I, Spies JB. Symptomatic fibroleiomyomata: MR imaging of the uterus before and after uterine arterial embolization. Radiology. 2000;217:228–235. doi: 10.1148/radiology.217.1.r00se49228. [DOI] [PubMed] [Google Scholar]


