Abstract
Objective: To investigate the efficacy and safety of tranexamic acid (TXA) injection during primary total knee arthroplasty (TKA) for reducing postoperative hemorrhage. Methods: 100 cases of patients admitted to our hospital and underwent primary unilateral TKA from January 2012 to December 2014 were enrolled in this study and they were divided randomly into two groups. For the TXA group, 1 g TXA was dissolved in 50 ml 0.9% sodium chloride solution and injected after prosthesis implantation but before cavity close. Conventional drainage clamping was carried for 4 h and the drainage tube was removed 48 h postoperative. For the control group, similar measures were taken except for that no TXA was dissolved in 0.9% sodium chloride solution. Postoperative hemoglobin, blood coagulation index, total blood loss volume, drainage volume, blood transfusion rate and lower extremity deep vein thrombosis (DVT) rate in both groups were observed and the efficacy and safety of this surgical treatment were evaluated. Results: There were no significant differences in operation time, postoperative platelet and APPT, D-dimer, lower limb venous thrombosis incidence rate 1 week after operation between the two groups. Postoperative drainage volume, hemoglobin, total blood loss and blood transfusion rate in the TXA group were significantly lower than those of the control group. Ecchymosis of lower extremity peripheral incision and its surroundings was significantly milder than that of the control group. Conclusion: Intraoperative intra-articular injection of TXA in TKA can significantly reduce the initial postoperative hemorrhage and blood transfusion rate at the early stage after operation.
Keywords: Arthroplasty, replacement, knee, hemorrhage, tranexamic acid, venous thrombosis
Introduction
Total knee arthroplasty (TKA), which is recognized by orthopedic physicians, has become the ideal method for treating knee diseases like end-stage knee osteoarthritis and rheumatoid arthritis. With the arrival of aging society, the number of patients who have received TKA operation increases greatly. However, during TKA operation, as intraoperative osteotomy is relative complex and the fibrinolysis system are activated [1], it is easy to cause large amount of blood loss and as a result the patients usually need blood transfusion. Blood transfusion can lead to great burden to both the patients’ families and the society. Orthopedics physicians have paid attention to exploratory research on many kinds of treatment in order to reduce hidden and dominant hemorrhage during the perioperative period of TKA.
At present, antifibrinolytics has been widely used in the prevention of intraoperative hemorrhage. In the recent years, a META analysis [2] confirmed that infusion of tranexamic acid (TXA) can effectively reduce TKA or total hip arthroplasty (THA) hemorrhage and reduce blood transfusion rate without increasing risks. Some scholars also point that using hemostatic drugs such as TXA at the hyperfibrinolysis stage of perioperative period can reduce postoperative hemorrhage without increasing the risk of venous thrombosis. However, some studies argue that TXA could not effectively reduce hemorrhage in the operation of TKA or THA. Moreover, it has been reported that intravenous infusion of TXA can lead to high coagulation state of the body thus increasing the risk of thrombosis [3]. As a result, some doctors have tried topical application of TXA in THA at the peri-and postoperative period to reduce hemorrhage and have achieved good effects [4]. Shen et al. [5] considered that drainage clamping for 4 h can reduce hemorrhage after operation, however, it has the potential risks of increasing intra-articular hematoma formation, lower limb ecchymosis, and deep vein thrombosis (DVT) theoretically.
To date, there is no report about intraoperative intra-articular injection of TXA with temporarily closing drainage during TKA operation so as to reduce hemorrhage. In this study, the surgical method of intraoperative intra-articular injection of TXA and temporarily closing drainage for reducing postoperative hemorrhage in TKA was performed, meanwhile, prospective randomized controlled study was used to evaluate the effectiveness and safety of this surgical method.
Materials and methods
Patients’ data
A total of 100 cases of patients admitted to our hospital and underwent primary unilateral TKA from January 2012 to December 2014 were enrolled in this study. They were randomly divided equally into experimental group (TXA group) and control group (placebo group). The exclusion criteria was as follows: (1) patients with preoperative anemia or coagulopathy; (2) patients with infectious active diseases like lower limb infection or systemic infection disease; (3) patients with TXA contraindications; (4) patients with a history of venous thromboembolic disease or thromboembolic disorders; (5) patients with clotting problem like liver tumor or cirrhosis; (6) patients intended to participate in autologous blood transfusion; (7) incompatibility patients. Prior written and informed consent were obtained from all patients and the study was approved by the ethics review board of the Shandong Provincial Hospital.
Operation method and postoperative treatment
Discontinuation of aspirin and warfarin was taken at least 7 days before operation and the operation was performed by the same surgeon (Professor Shui Sun). All patients were treated with patellar medial approach, and the implants were CR knee bone cement prosthesis Gemini MKII (Waldemar Link GmbH & Co, Hamburg, Deutschland). For TXA group, 1 g TXA was dissolved in 50 ml 0.9% sodium chloride solution and injected after prosthesis implantation and before cavity close. Conventional pipe clamping was carried for 4 h and the drainage tube was removed 48 h postoperative. For the control group, similar measures were taken except for that no TXA was dissolved in 50 ml 0.9% sodium chloride solution. Anticoagulant therapy of 5000 iu low molecular weight heparin was applied to both groups 8 h after operation. Transfusion therapy was carried for patients with hemoglobin (Hb) less than 70 g/L blood, appropriate transfusion was carried for patients with Hb of 70-90 g/L according to the general conditions, and no blood transfusion was carried for patients with Hb higher than 90 g/L. Autologous blood transfusion was not performed in both groups intraoperative.
One week after operation, ultrasound screening was carried out in order to detect lower limb venous thrombosis occurrence, and after the diagnosis subcutaneous injection of low molecular weight heparin with the amount of 5000 iu was carried every 12 h in patients with thrombosis. Oral rivaroxaban was applied for anticoagulation until the patients discharged and warfarin for anticoagulation was then continued after the patients discharged. The patients were followed up regularly and International Normalized Ratio (INR) value was monitored and the drugs were stopped after INR value returned to normal (2-2.5).
Postoperative conditions observation
A series of conventional indexes were observed after operation. Total drainage volume was observed and recorded in patients in both groups postoperative. Hb and red blood cell specific volume (Hct) of preoperative, 1 d, 3 d and 5 d after operation were monitored and recorded so as to calculate total blood loss volume according to Nadler et al. [6]. Meanwhile, the number of blood transfusion cases in both groups was recorded. For calculating related parameters, the following formulas were used. Total blood loss volume (ml) = preoperative blood volume (preoperative Hct-postoperative Hct); preoperative blood volume = K1 × height3 (m) + K2 × weight (kg) + K3; total blood loss volume of peri operation period = Total blood loss volume + allogeneic blood transfusion volume (for male, K1 = 0.3669, K2 = 0.03219, K3 = 0.6041; for female, K1 = 0.3561 K2 = 0.03308, K3 = 0.1833) Preoperative and 24 h.
postoperative values of coagulation indexes of D-dimer, platelet count, and activated partial thromboplastin time (APTT) were observed and recorded. Autologous blood transfusion was not performed in both groups and the rate of blood transfusion was calculated. Lower extremity venous color Doppler ultrasound screening was carried preoperative and 1 week after surgery to detect the occurrence of DVT, additionally, the incidence of venous thrombosis of lower extremity was recorded. General conditions of wound healing, skin ecchymosis, hematoma and whether adverse reactions such as postoperative nausea, vomiting and allergies appeared in TXA group 3 days after operation were recorded.
Statistical analysis
All the statistical analyses were performed using SPSS version 17.0 (SPSS Inc, Chicago, IL, USA) for Windows. Measurement data were expressed as Mean ± SD. Measurement data fitting the normal distribution were analyzed by t test. Counting data were compared by Chi-square test between the two groups. P < 0.05 was considered as statistically significant.
Results
Preoperative general conditions comparison
To identify whether the patients in both groups had the same conditions, preoperative general conditions were compared. As shown in Table 1, there were no statistically significant differences between the two groups in age, gender, body mass index, operation time, preoperative Hb, platelet value before operation, preoperative APTT, D-dimer, anesthesia and prosthesis type. The results indicated that the patients in both groups had the same general conditions before operation.
Table 1.
Preoperative basic clinical data of patients in the two groups (x ± s)
| Basic data | TXA group | Control group | T (X2) value | P value |
|---|---|---|---|---|
| Age | 52.6 ± 12.4 | 53.2 ± 10.2 | 0.2642a | > 0.05 |
| Gender (male/female) | 25/25 | 22/28 | 0.3613b | > 0.05 |
| Body mass index (BMI) | 26.23 ± 2.17 | 25.62 ± 3.03 | t’ = 1.1574a | > 0.05 |
| Preoperative hemoglobin (g/L) | 126.30 ± 10.65 | 131.25 ± 12.29 | 2.1523a | > 0.05 |
| Preoperative platelet | 220 ± 67.23 | 237 ± 48.35 | t’ = 1.4516a | > 0.05 |
| Preoperative APTT | 30.24 ± 3.42 | 31.36 ± 3.78 | 1.5536a | > 0.05 |
| Preoperative D-dimer | 0.46 ± 0.03 | 0.45 ± 0.04 | t’ = 1.4142a | > 0.05 |
| Protopathy (OA/RA) | ||||
| Anesthesia (spinal/general anesthesia) | 23/27 | 24/26 | 0.0401b | > 0.05 |
| Types of prosthesis (CR/PS) | 50/0 | 50/0 | 1 |
APTT, activated partial thromboplastin time;
t test;
chi-square test.
T value is the statistic value of t test.
Postoperative data comparison
In order to evaluate the effect of TXA on the postoperative general condition, the corresponding indexes in both groups were compared. As shown in Table 2, there were no significant differences in operation time, postoperative platelet and APPT, D-dimer, lower limb venous thrombosis incidence rate 1 week after operation between the two groups. Postoperative drainage volume, hemoglobin, total blood loss and blood transfusion rate in the TXA group were significantly lower than those of the control group. Ecchymosis of lower extremity peripheral incision and its surroundings was significantly milder than that of the control group. To sum up, compared with the control group, patients in TXA group had better postoperative condition.
Table 2.
Comparison of observed postoperative indexes between TXA group and control group
| Observed indexes | TXA group | Control group | T (X2) value | P value |
|---|---|---|---|---|
| Operation time | 58.2 ± 10.63 | 60.8 ± 9.87 | 1.2674a | > 0.05 |
| Hemoglobin D-value (g/L) | 22.9 ± 8.27 | 39.73 ± 10.01 | 9.1654a | < 0.05 |
| Total blood loss (ML) | 678.45 ± 112.77 | 1136.3 ± 224.52 | -12.8856a | < 0.05 |
| Drainage volume (ML) | 389.15 ± 108.83 | 796.3 ± 212.6 | -12.0542a | < 0.05 |
| Preoperative D-dimer | 0.46 ± 0.05 | 0.47 ± 0.04 | 1.1043a | > 0.05 |
| Preoperative platelet | 236 ± 64.95 | 227 ± 59.24 | 0.7239a | > 0.05 |
| Preoperative APTT | 36.75 ± 3.31 | 35.91 ± 2.87 | 1.3558a | > 0.05 |
| Blood transfusion rate | 4% (2/50) | 18% (9/50) | 5.0051b | < 0.05 |
| Incidence of thrombosis of lower limb | 6% (3/50) | 4% (2/50) | 0.2105b | > 0.05 |
| Incidence of lower extremity petechia | 2% (1/50) | 14% (7/50) | 4.8913b | < 0.05 |
APTT, activated partial thromboplastin time;
t test;
chi-square test.
T value is the statistic value of t test.
Comparison of the complications
To assess the safety of intra-articular TXA application, lower extremity venous ultrasound review was performed 1 week after operation. Lower extremity venous ultrasound screening (Figure 1) at 1 week after operation showed that lower limb venous thrombosis appeared in 3 cases in TXA group and in 2 cases in control group but with no significant difference in the incidence of DVT rate (P > 0.05). During the follow-up, no pulmonary embolism, cerebral embolism and other complications were found. There were only 1 case of right leg ecchymosis in TXA group 3 days after operation while skin and thigh ecchymosis around the lower limb incision was found in 7 cases in the control group, with statistically significant difference (P < 0.05) (Figure 2). Three days after surgery, no allergy, nausea, vomiting or other adverse reactions were found in TXA group. Together, it is possible that TXA could reduce TKA perioperative bleeding without increasing the risk of short term thrombosis and had no perioperative adverse reaction.
Figure 1.
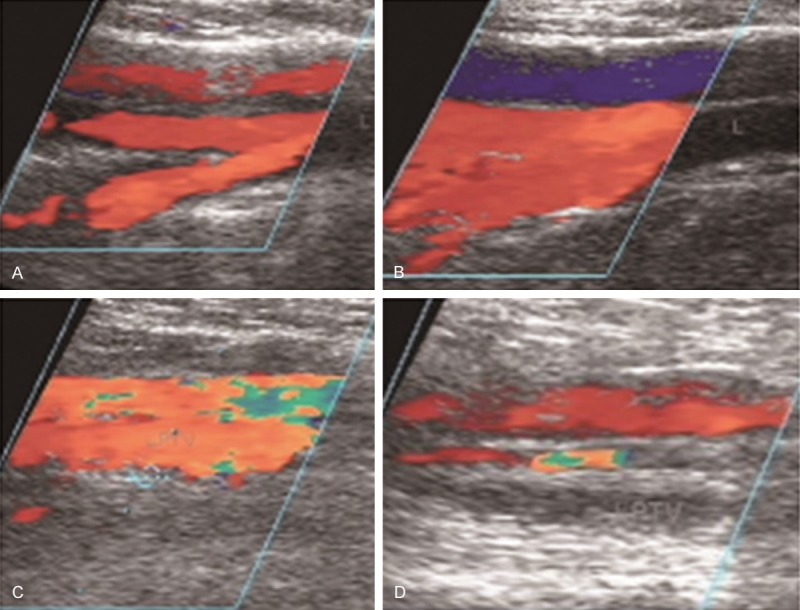
Preoperative and postoperative ultrasonography of patients in TXA and control groups. Preoperative ultrasonography of patients in TXA group (A) and control group (C). Ultrasonography of 1 week after surgery in patients of TXA group (B) and control group (D).
Figure 2.

General condition of wound healing after operation. Ecchymosis surrounding incision (A) and in the thigh (B) was found in patients of control group while no ecchymosis was found in patients in TXA group (C).
Discussion
Application of TXA includes intravenous, intramuscular injection, local joint cavity injection and oral treatment. Peng et al. [7] found that a single intravenous injection of TXA before tourniquet release can effectively reduce postoperative hidden hemorrhage and postoperative blood transfusion rate. Meanwhile, intra-articular administration can avoid the adverse reactions of systemic therapy with higher local effective medicine concentration and better effect in principle. In one study, Konig et al. [8] diluted 3 g TXA with 100 ml physiological saline and 20 ml TXA solution were used for soaking after acetabular burrs and femoral intramedullary reaming, in addition, the remaining 60 ml TXA solution was used for articular cavity soaking. They found that blood transfusion rate had decreased by 14% and bleeding volume reduced. The deficiency of this study was that the prolonged operation time can increase the infectious probability in theory. In our study, TXA was injected after prosthesis implantation and before cavity close followed by 4 h of conventional pipe clamping, without increasing the operation time. At the same time, bleeding volume, drainage volume and blood transfusion rate were reduced without increasing the incidence of postoperative venous thrombosis of lower extremity.
Hidden hemorrhage refers to perioperative period hemoglobin loss caused by blood extravasation in tissue gap and missing in the joint cavity together with hemolysis. It is the D-value between total blood loss volume and the sum of intraoperative bleeding volume and postoperative drainage volume. Intraoperative hidden hemorrhage of TKA could not be ignored. Senthil et al. [9] argue that 84% postoperative hemorrhage of TKA occurs in the early 12 h after operation and in theory, closing the drainage tube at the early stage can increase the intra-articular pressure, thereby reduce bleeding and postoperative hidden hemorrhage. However, there is great dispute on drainage clamping time. Mutsuzaki et al. [10] showed that injection of TXA via the drainage duct after TKA and keeping the drainage closed for 1 h can reduce 643 ml of postoperative hemorrhage, and reduce 21% of allogeneic blood transfusion rate. However, according to Kiely et al. [11], keeping the drainage duct closed for 2 h does not influence the final hemorrhage. In this study, drainage duct was closed for 4 h and the final result showed that it was safe and effective, successfully reduced the drainage volume and total hemorrhage.
In the TKA operation, tourniquet application is relatively common so as to obtain more clear operation visual field and reduce operation time. However, Katsumata et al. [12] showed that even a short time of tourniquet using in limbs operation could activate local fibrinolysis system, leading to continued local hemorrhage after operation. As a result, application of tourniquet and multiple osteotomy in TKA operation might contribute to increased hemorrhage and postoperative local ecchymosis formation. However, intraoperative intra-articular application of TXA can inhibit fibrin decomposition induced by plasmin and decrease hemorrhage led by hyperfibrinolysis, thereby reduce the blood oozing from the wound surface, hidden hemorrhage, drainage volume, blood loss volume, blood transfusion rate and postoperative exudation, and reduce ecchymosis surrounding incision in terms of theory which was consistent with the conclusion of our research.
During the TKA operation, the maximum security concerns of the application of TXA should be that it might increase the incidence of DVT. Routine double lower limbs vein color Doppler ultrasound screening for DVT 1 weeks after operation found that the incidence of DVT in TXA group and the control group were 6% (3/50) and 4% (2/50) respectively, with no statistical significant difference. Together, we consider that intraoperative intra-articular injection of TXA can significantly reduce postoperative bleeding and blood transfusion rate without increasing the incidence of DVT in the early postoperative period.
In conclusion, intraoperative intra-articular injection of TXA during TKA can significantly reduce blood transfusion rate, postoperative drainage volume and total blood volume. No significant differences were found between the two groups in platelet count, blood coagulation index APTT and D-dimer 24 h after operation. Meanwhile, there was no significant difference in short term (1 week after surgery to discharge) lower limb venous thrombosis incidence rate, indicating that in addition to reducing TKA perioperative period hemorrhage, TXA did not increase the risk of thrombosis and reduced local skin ecchymosis after TKA. No pulmonary embolism or cerebral embolism case was found in both groups.
The results showed that this surgical method had obtained good curative effect, however, there are some shortcomings in this study. The screening time and method for DVT of lower extremity was single, although screening of preoperative and 1 week postoperative together with the long-term clinical observation were performed, there might be some missing asymptomatic DVT leading to some bias on the incidence of DVT. Moreover, drainage volume, total blood loss volume and blood transfusion volume were less than other reports, which might be related to conventional compression wounds bandaging after operation, postoperative local cold compress therapy and tourniquet set, and this still needs to be confirmed by further clinical study.
Acknowledgements
This work was supported by a grant from the National Natural Science Foundation of China (No. 81271966).
Disclosure of conflict of interest
None.
References
- 1.Benoni G, Lethagen S, Fredin H. The effect of tranexamic acid on local and plasma fibrinolysis during total knee arthroplasty. Thromb Res. 1997;85:195–206. doi: 10.1016/s0049-3848(97)00004-2. [DOI] [PubMed] [Google Scholar]
- 2.Yang ZG, Chen WP, Wu LD. Effectiveness and safety of tranexamic acid in reducing blood loss in total knee arthroplasty: a meta-analysis. J Bone Joint Surg Am. 2012;94:1153–1159. doi: 10.2106/JBJS.K.00873. [DOI] [PubMed] [Google Scholar]
- 3.Zufferey PJ, Miquet M, Quenet S, Martin P, Adam P, Albaladejo P, Mismetti P, Molliex S tranexamic acid in hip-fracture surgery (THIF) study. Tranexamic acid in hip fracture surgery: a randomized controlled trial. Br J Anaesth. 2010;104:23–30. doi: 10.1093/bja/aep314. [DOI] [PubMed] [Google Scholar]
- 4.Gilbody J, Dhotar HS, Perruccio AV, Davey JR. Topical tranexamic acid reduces transfusion rates in total hip and knee arthroplasty. J Arthroplasty. 2014;29:681–684. doi: 10.1016/j.arth.2013.09.005. [DOI] [PubMed] [Google Scholar]
- 5.Shen PC, Jou IM, Lin YT, Lai KA, Yang CY, Chern TC. Comparison between 4-hour clamping drainage and nonclamping drainage after total knee arthroplasty. J Arthroplasty. 2005;20:909–913. doi: 10.1016/j.arth.2005.01.017. [DOI] [PubMed] [Google Scholar]
- 6.Nadler SB, Hidalgo JH, Bloch T. Prediction of blood volume in normal human adults. Surgery. 1962;51:224–232. [PubMed] [Google Scholar]
- 7.Peng H, Weng X, Zhai J, Jin J, Lin J, Qian W, Zuo Y, Zhao L. Use of intravenous tranexamic acid combined with temporary clamping of drain reduce postoperative blood loss in total knee arthroplasty. Chinese Journal of Orthopaedics. 2014;34:400–405. [Google Scholar]
- 8.Konig G, Hamlin BR, Waters JH. Topical tranexamic acid reduces blood loss and transfusion rates in total hip and total knee arthroplasty. J Arthroplasty. 2013;28:1473–1476. doi: 10.1016/j.arth.2013.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Senthil Kumar G, Von Arx OA, Pozo JL. Rate of blood loss over 48 hours following total knee replacement. Knee. 2005;12:307–309. doi: 10.1016/j.knee.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 10.Mutsuzaki H, Ikeda K. Intra-articular injection of tranexamic acid via a drain plus drain-clamping to reduce blood loss in cementless total knee arthroplasty. J Orthop Surg Res. 2012;7:32. doi: 10.1186/1749-799X-7-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kiely N, Hockings M, Gambhir A. Does temporary clamping of drains following knee arthroplasty reduce blood loss? A randomised controlled trial. Knee. 2001;8:325–327. doi: 10.1016/s0968-0160(01)00095-3. [DOI] [PubMed] [Google Scholar]
- 12.Katsumata S, Nagashima M, Kato K, Tachihara A, Wauke K, Saito S, Jin E, Kawanami O, Ogawa R, Yoshino S. Changes in coagulation-fibrinolysis marker and neutrophil elastase following the use of tourniquet during total knee arthroplasty and the influence of neutrophil elastase on thromboembolism. Acta Anaesthesiol Scand. 2005;49:510–516. doi: 10.1111/j.1399-6576.2005.00621.x. [DOI] [PubMed] [Google Scholar]


