Abstract
Objectives
To analyse the effect of biological agents (BAs) in terms of achieving inactive disease (ID) or clinical remission (CR) in patients with systemic juvenile idiopathic arthritis (SJIA), to describe effects of switching or discontinuing a BA and to assess the proportion of patients able to maintain ID or CR off steroids and after withdrawing BA therapy.
Methods
Retrospective study in a French paediatric rheumatology reference centre using the CEMARA (CEntre des MAladies RAres) register.
Results
Seventy-seven patients were included with a cumulative follow-up of 245.5 patient-years (median 1.1, range 0.5–8.0). On a first BA, ID was achieved in 37 patients, including 1 patient out of 12 patients on etanercept, 26 patients out of 51 on anakinra and 7 out of 10 on canakinumab. One patient on abatacept and two patients on tocilizumab also achieved ID. Switching of BA was common. The switch to a second (n=34), third (n=18) or fourth (n=4) BA resulted in ID in a further 13 patients, either on canakinumab (n=6) or tocilizumab (n=7). At last follow-up, 40 patients were in CR (27 patients off steroids, 5 patients having never received steroid treatment), either on (n=29) or off (n=11) BA.
Conclusions
In this series of patients with SJIA, interleukin-1 inhibitors were associated with a higher proportion of ID than tumour necrosis factor inhibitors when used as first BA. Switching allowed some patients to achieve ID when treated with canakinumab or tocilizumab. CR was eventually achieved in more than half of the patients.
Keywords: Juvenile Idiopathic Arthritis, DMARDs (biologic), Outcomes research, TNF-alpha
Key messages.
What is already known on this subject?
Achievement of inactive disease and clinical remission (CR) has become a realistic goal for the treatment of systemic juvenile idiopathic arthritis.
What does this study add?
Introducing an IL-1 or an IL-6 inhibitor as a first biologic treatment dramatically increases the chances of SJIA patients to ever achieve CR, as compaired to TNF-alpha inhibitors, even if some patients may achieve CR on canakinumab or tocilizumab as second or third line biologic agents.
How might this impact on clinical practice?
In biologic-naive SJIA patients, any IL-1 or an IL-6 inhibitor may be recommended in a treat-to-target approach aiming to achieve inactive disease within a few months; in non-biologic naive SJIA patients, canakinumab and tocilizumab seem the best options to try and obtain complete remission.
Introduction
Systemic-onset juvenile idiopathic arthritis (SJIA) is characterised by spiking fever, evanescent rash, hepatosplenomegaly, serositis, lymphadenopathy and arthritis. According to the International League Against Rheumatism (ILAR) criteria, it has been classified as a subtype of juvenile idiopathic arthritis.1 However, it presents major differences in comparison to other subtypes. Key players of the innate immunity system are involved in its pathophysiology, supporting that SJIA is an autoinflammatory syndrome.2 3
Several biological agents (BAs) have become available for the treatment of SJIA over the last decade. The first available and studied BA in JIA with polyarticular course was etanercept, a tumour necrosis factor (TNF)–α receptor antagonist. Several reports showed a resounding efficacy in non-systemic JIA, but less consistent effect in SJIA.4 5
Anti-interleukin (IL)-1 and IL-6 therapies have proven efficacy in clinical trials. Anakinra, the first IL-1 receptor antagonist, was shown to be effective in SJIA, with evidence of dramatic responses in subgroups of patients with SJIA.2 6–11 Canakinumab, an anti-IL-1 antibody, and tocilizumab, an anti-IL-6 receptor antibody, demonstrated efficacy in SJIA treatment.12 13 Another anti-IL-1 fusion protein, rilonacept, was evaluated in a phase III trial.14
However, the choice of a BA may be difficult. Prescription strategies have to take into account several factors, including the heterogeneity of the disease course, the availability of BAs and treatment guidelines with change over time15 16 or national marketing authorisation restrictions. Data from observational studies, in this situation, provide important information for the clinician's decision on starting a specific BA or switching to another in case of lack of effectiveness, loss of response or adverse events.
We therefore conducted a retrospective study addressing drug survival, achievement of inactive disease and reason for switching of BA in SJIA.
Patients and methods
Study design
This was a retrospective study in Necker Enfants-Malades Hospital, Paris, France, the French reference centre for rare paediatric rheumatological and inflammatory diseases (CERHUMIP); the study used the CEMARA (CEntre des MAladies RAres) register, a nationwide information system for rare diseases.17 The CEMARA register includes all patients with rare diseases. The data that are entered represent core information allowing the identification of the patient, details of medical history, diagnosis and treatment. After extraction of CEMARA data, the medical records were fully reviewed. The CEMARA system benefits from an agreement with the French National Committee on Informatics and Liberty (CNIL). According to the French legislation, patients and parents were informed but no informed consent form was required for a retrospective analysis.
Patients and treatment
For this study, we identified all patients with a diagnosis of SJIA based on ILAR criteria who started their first BA therapy between 1 January 2005 and 30 June 2012. Patients having been treated with BA before the study period were excluded. Follow-up of at least 6 months after BA treatment initiation had to be accomplished in our centre. The last follow-up registered was on 31 December 2012. The choice of a specific BA treatment was not restricted in our centre.
Clinical assessment
Baseline patient characteristics included gender, age at first symptoms and age at diagnosis. Evaluation of medications included previous and concomitant treatments, including changes of corticosteroid dosage under BA treatment.
Clinical evaluation was assessed by the following variables: active joint count, limited joint count, morning stiffness, fever, rash, hepatosplenomegaly, generalised lymphadenopathy, serositis, history of macrophage activation syndrome and other comorbidity. Laboratory evaluation included complete blood count, erythrocyte sedimentation rate, C reactive protein and ferritin (if available).
Clinical evaluations of patients were recorded at the start of a new BA, in a time window of 2–5 months after starting a new BA and at last assessment under BA therapy, which could be either at last follow-up or at last assessment before switching to another BA. Drug survival was assessed at month 3, month 12, month 24 and at last follow-up, respectively.
Inactive disease required the absence of systemic symptoms, active joints and morning stiffness, with a physician's assessment that did not exceed 10/100 on the physician visual analogue scale (VAS), as proposed by Wallace et al.18 Owing to the retrospective setting, childhood health assessment questionnaire (CHAQ) and parent/patient assessment of disease activity were not included as supplementary criteria. Achievement of clinical remission on treatment was defined as inactive disease for >6 months under DMARD, steroids or BA therapy. Remission off treatment was defined as >12 months remission after withdrawing any disease-targeting medication.19
Follow-up, switch of BA and long-term outcome
We classified reasons for switching to a second, third or fourth BA into the following categories: adverse events, ineffectiveness, loss of response, convenience of use and patient's wish. Follow-up time under a BA was calculated from start of BA treatment until a switch to another BA treatment, the last follow-up visit or 31 December 2012, whichever occurred first.
Long-term outcome was evaluated with the following items: loss of articular function, short stature (defined as <2 SDs below the 50th centile), growth hormone treatment and disease-related surgery.
Safety
Safety was assessed by recording all serious adverse events (SAEs), including medical events of special interest (severe infection, malignancy or organ dysfunction). Adverse events in immediate relation to a drug administration were recorded separately with differentiation into allergic reaction, infusion reaction or other.
Data analysis
Descriptive statistical analysis was reported as absolute frequencies. Mean values were given with the SD, median values were given with the range. One-way analysis of variance was used for comparison of baseline characteristics at start of first biological therapy. Fisher's exact test was used to compare achievement of inactive disease. To describe differences in drug discontinuation, a log-rank test based on Kaplan-Meier survival was performed. p Values less than 0.05 were considered statistically significant with a two-sided test performed.
Statistical analysis was performed with SPSS Statistical software, V.22 (IBM, USA).
Results
Patients and first-line BA therapy
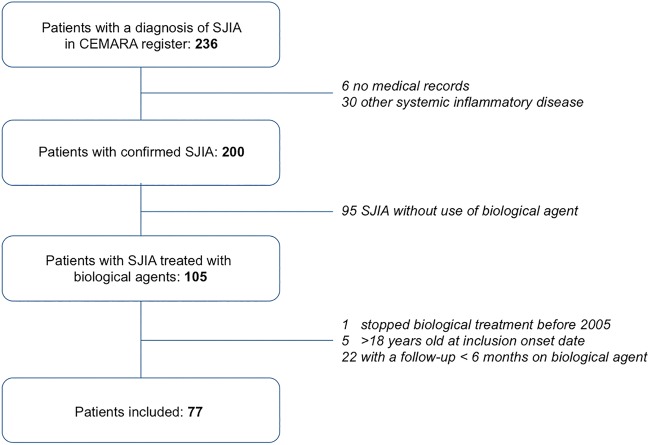
Out of 236 patients included in CEMARA with a diagnosis of SJIA, 77 were included (figure 1) with a cumulative follow-up duration on BA of 245.5 patient-years. Patients’ characteristics at start of first BA therapy are described in table 1. Full disease activity and laboratory parameters were available for 66 patients.
Figure 1.
Flow chart (CEMARA, CEntre des MAladies RAres; SJIA, systemic juvenile idiopathic arthritis).
Table 1.
Baseline characteristics at start of first biological therapy
| Total | Etanercept | Anakinra | Canakinumab | Tocilizumab | |
|---|---|---|---|---|---|
| Number of patients | 77* | 12 | 51 | 10 | 2 |
| Sex, female/male† | 40/37 | 7/5 | 27/24 | 4/6 | 1/1 |
| Age at diagnosis, median years (IQR) | 3.8 (2.6–7.1) | 4.1 (3.0–6.9) | 3.6 (2.3–6.8) | 6.0 (5.0–8.4) | 3.3 (3.2–3.4) |
| Disease duration, median months (IQR) | 24.0 (7.5–53.8) | 15.7 (5.6–40.2) | 31.0 (9.3–59.1) | 6.7 (3.8–18.8) | 57.3 (35.6–78.9) |
| Previous treatments | |||||
| Number (%) using NSAIDs | 77 (100) | 12 (100) | 51 (100) | 10 (100) | 2 (100) |
| Number (%) using corticosteroids | 76 (98.7) | 12 (100) | 51 (100) | 9 (90) | 2 (100) |
| Number (%) using methotrexate | 23 (29.8) | 3 (25) | 16 (31.4) | 3 (30) | 0 (0) |
| Number (%) using other DMARDs | 4 (5.2) | 1 (8.3) | 2 (3.9) | 1 (10) | 0 (0) |
| Disease activity parameter at start of first biological agent | |||||
| Patients with available details, n (%) | 66 (86) | 10 (83.3) | 44 (86.3) | 10 (100) | 2 (100) |
| Systemic symptoms | |||||
| Fever (%) | 27 (40.9) | 5 (50) | 17 (38.6) | 4 (40) | 1 (50) |
| Rash (%) | 13 (19.7) | 2 (20) | 8 (18.2) | 3 (30) | 0 (0) |
| Number of active joints, mean (SD) | 6.3 (5.6) | 9.5 (7.1) | 5.2 (5.0) | 8.3 (7.4) | 2 (0) |
| Number of joints with limitation of motion, mean (SD) | 6.7 (6.3) | 9.9 (7.6) | 5.6 (5.2) | 9.1 (8.4) | 2 (0) |
| Laboratory parameter at start of first biological agent | |||||
| Erythrocyte sedimentation rate in mm, mean (SD) | 61.4 (29.8) | 62.2 (29.5) | 63.7 (29.3) | 61.7 (25.9) | 120 (14.1) |
| High leucocyte count‡, % | 68 | 50 | 73 | 70 | 100 |
| High thrombocyte count‡, % | 73 | 50 | 75 | 70 | 100 |
| Low haemoglobin§, % | 77 | 70 | 84 | 80 | 100 |
| Number of history of MAS | 5 | 1 | 4 | 0 | 0 |
| Concomitant treatment with first biological agent | |||||
| Number (%) using NSAIDs | 74 (96.1) | 11 (91.7) | 49 (96.1) | 10 (100) | 2 (100) |
| Number (%) using methotrexate | 9 (11.7) | 1 (8.3) | 6 (11.8) | 1 (10) | 0 (0) |
| Number (%) MTX introduced after start of BA | 6 (7.8) | 0 (0) | 6 (11.8) | 0 (0) | 0 (0) |
| Number (%) using prednisone | 64 (83.1) | 10 (83.3) | 43 (84.3) | 9 (90) | 1 (50) |
| Predniso(lo)ne dosage, median mg/kg body weight/day (IQR) | 0.50 (0.3–1.1) | 0.6 (0.3–1.2) | 0.56 (0.3–1.0) | 0.4 (0.3–0.5) | 1.5 (–) |
*One patient was started on adalimumab and one patient on abatacept.
†There were no significant differences between etanercept, anakinra and canakinumab for all variables as compared by one-way ANOVA.
‡Above upper age-corrected reference value.
§Below lower age-corrected reference value.
ANOVA, analysis of variance; BA, biological agent; DMARD, disease-modifying antirheumatic drug; MAS, macrophage activation syndrome; MTX, methotrexate; NSAID, non-steroidal anti-inflammatory drug.
The first BA was anakinra in 51 patients, etanercept in 12, canakinumab in 10, tocilizumab in 2, and adalimumab and abatacept in 1 patient each. Median follow-up duration on BA was 33.8 months (range 1.8–97.9) for the patients who did not experience a switch of BA; for switchers, median follow-up duration on BA was 6.7 months (range 0.5–55.0) under the first BA, 12.0 months (range 0.5–73.6) under the second and 10.6 months (range 2.0–56.2) under the third BA.
Effectiveness of first-line BA therapy and drug survival
Inactive disease was achieved and maintained at last follow-up in 37 patients (48.1%) without changing BA therapy. This was observed in 33 out of 61 patients on anti-IL-1 treatment, the 2 patients on tocilizumab and 1 patient on abatacept, but only in 1 of the 13 patients who received anti-TNF as first-line BA therapy.
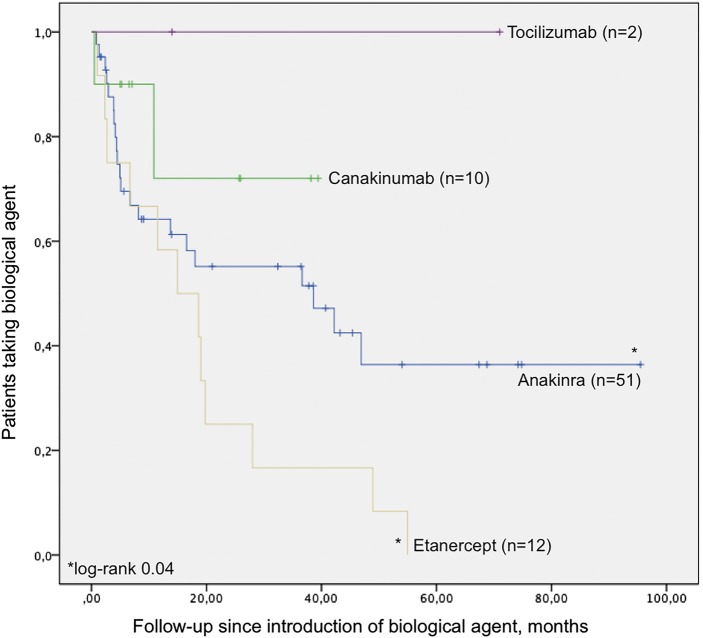
Kaplan-Meier estimates of first BA continuation until discontinuation due to ineffectiveness, adverse events, loss of response, convenience of use and patient's wish, showed significant differences in favour of anakinra as compared with etanercept (log-rank 0.04, figure 2).
Figure 2.
Kaplan-Meier estimate of drug continuation until discontinuation for tocilizumab, canakinumab, anakinra and etanercept, as a first biological agent for adverse events, ineffectiveness of treatment, loss of response, convenience of use and patient's choice. Censoring, defined as the time of discontinuation or, when a patient was still receiving the drug, the time of the last study visit, is shown by vertical lines.
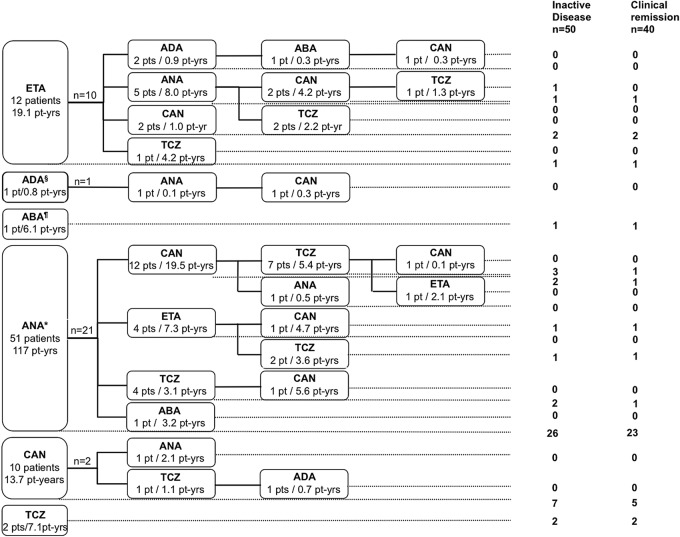
BA switching
Switching of biological therapy was common, with 34 patients (44.2%) switching to a second, 18 (23.4%) to a third and 4 (5.2%) to a fourth BA (figure 3). For all BA switches (total n=56), the reasons were lack of effectiveness in 33 patients (58.9%), loss of response in 12 (21.4%), adverse event in 7 (12.5%), and convenience of use and patient's choice in 2 patients each (3.6%).
Figure 3.
Switching of biological agents (BAs), and achievement of inactive disease and clinical remission (CR). ETA, etanercept; TCZ, tocilizumab. §The only patient on adalimumab (ADA) as first-line treatment was switched after 9.5 months to anakinra (ANA) and steroids, then canakinumab (CAN) and steroids, but arthritis persisted. ¶The only patient on abatacept (ABA) as first-line treatment initially achieved partial response and was in CR at last follow-up. *Six patients with ANA as a first BA and two patients with ANA as a second BA experienced secondary introduction of methotrexate (median delay of introduction 10.5 months after start of ANA, range 6–25 months). Four patients with ANA as a first BA achieved inactive disease that persisted at last follow-up.
Switching to a new BA was, in most cases, prescribed after a short BA-free interval. The median treatment-free interval was 0.8 months (range 0.0–34.2) between the first and the second BA, 0.2 months (range 0.0–3.7) between the second and third, and 1.9 months (range 0.5–4.8) between the third and fourth BA.
Among 51 patients on anakinra as a first BA, 21 (41%) were switched to a new BA. Out of 13 patients on anti-TNF inhibitor as a first BA, 11 (85%) switched. Of the 10 patients with canakinumab as first-line treatment, 2 experienced a switch (20%).
Inactive disease and drug survival after switching BA
Inactive disease at last follow-up was achieved in 37 patients with a first BA, 43 (55.8%) with a second BA, 49 (63.6%) with a third and 50 (64.9%) under a fourth BA.
Used either as first BA or after switch, the rate of inactive disease per treatments received was 44.1% for anakinra (59 times prescribed as a first, second, third or fourth BA), 41.9% for canakinumab (31 times prescribed) and 45% for tocilizumab (20 times prescribed). Etanercept treatment led to a significantly lower rate of inactive disease under treatment when compared with anakinra and to canakinumab (p=0.03 and p=0.04, respectively) with achievement of inactive disease only described in 1 out of 17 courses (5.9%).
Inactive disease was more difficult to achieve when any switch became necessary. Switching to canakinumab or tocilizumab as second, third or fourth BA led to inactive disease in 6 out of 19 (31.6%) and 7 out of 17 cases (41%), respectively. No patient achieved inactive disease after switching any BA to etanercept (n=5, in 2 cases despite introduction of methotrexate), adalimumab (n=3, in one case despite introduction of methotrexate) or abatacept (n=2; table 2).
Table 2.
Inactive disease under treatment at last follow-up
| First agent (%) |
Second agent (%) |
Third agent (%) |
Fourth agent (%) |
|
|---|---|---|---|---|
| Etanercept | 1/12 (8) | 0/4 (0) | – | 0/1 (0) |
| Adalimumab | 0/1 (0) | 0/2 (0) | 0/1 (0) | – |
| Abatacept | 1/1 (100) | 0/1 (0) | 0/1 (0) | – |
| Anakinra | 26/51 (51) | 0/7 (0) | 0/1 (0) | – |
| Canakinumab | 7/10 (70) | 4/14 (29) | 2/5 (40) | 0/2 (0) |
| Tocilizumab | 2/2 (100) | 2/6 (33) | 4/11 (36) | 1/1 (100) |
| Total inactive disease | 37/77 | 6/34 | 6/19 | 1/4 |
Patients who were switched to canakinumab (n=19) or tocilizumab (n=17) as second-line or third-line treatments, showed drug survivals at 3, 12 and 24 months of 95%, 63% and 53% for canakinumab and 94%, 82% and 47% for tocilizumab, respectively. When anakinra was used as a second-line or third-line treatment (n=8), drug survival at 3, 12 and 24 months was 71%, 43% and 33%, respectively.
Clinical remission off steroids, BA withdrawal and long-term outcome
Forty of the 50 patients who achieved inactive disease fulfilled the criteria of clinical remission on treatment (27 patients off steroids) at last follow-up, corresponding to 51.9% of the study population: 23 on anakinra, 10 on canakinumab, 5 on tocilizumab, 1 patient on etanercept and 1 patient on abatacept.
At initiation of the first BA, 64 patients (83.1%) had received concomitant systemic corticosteroid treatment with a median daily dose of 0.50 mg/kg/day (range 0.1–2.0); at last follow-up, systemic corticosteroids were given to 29 patients (37.7%) with a median daily dose of 0.21 mg/kg/day (range 0.05–0.8).
Among five patients who had never received corticosteroids before or during BA treatment (4 on anakinra and 1 on canakinumab as first BA; median disease duration 4.0 months, median age 3.6 years), two patients under anakinra did not switch BA treatment, one patient switched to canakinumab for convenience of use, and one patient switched from anakinra to tocilizumab for incomplete response to the first treatment. The patient under canakinumab as first BA did not switch treatment. All patients were in clinical remission at last follow-up (median treatment duration 21.1 months).
BA was stopped in 12 patients after a median of 36.7 months (range 8.9–73.6), all treated with only one BA (11 anakinra, 1 abatacept). This subpopulation did not significantly differ in any baseline characteristics from the group that continued treatment.
Four patients relapsed, two with systemic symptoms, two with arthritis; inactive disease was again achieved on non-steroidal anti-inflammatory drugs (n=2), low-dose steroids (n=1) or resuming BA treatment (n=1).
A persisting limitation or loss of normal range of articular motion of ≥1 joint was recorded in 45 of 77 patients (65.6%) at last follow-up. Fourteen patients had developed short stature at last examination, with 11 children receiving growth hormone treatment. Four patients underwent surgical intervention for long-term complications of SJIA (hip replacement, hip arthroplasty, femoral osteotomy, wrist arthrodesis (n=1 each)).
Safety
No case of cancer or death was recorded. Table 3 lists the SAEs in detail. In total, 0.09 SAE/patient-year were recorded, occurring after a median of 16 months (range 0–34). There were no significant differences in SAE frequency between the different BA treatments. Eleven out of total 24 SAE (46%) occurred under concomitant corticosteroid treatment, 1 (4%) under methotrexate, and 3 (13%) under combined corticosteroid and methotrexate treatment. Nine of the SAE were classified as non-infectious. Two cases of macrophage activation syndrome were documented. BA treatment was stopped in both patients and another BA was started afterwards. SAE led to temporary BA treatment withdrawal in 10 patients, with recurrence of systemic symptoms in 3. Reintroduction of the same BA resulted in disappearance of the systemic features. Eight SAE led to definitive withdrawal of the BA, two under etanercept, one under anakinra, one SAE under canakinumab and four under tocilizumab. Six of these eight patients were switched to a new BA after 1 (n=2), 6 (n=2), 14 or 34 months. No SAE occurred afterwards.
Table 3.
Serious adverse events and safety of switching under BA treatment
| Order of treatment | Adverse event | Duration of treatment until onset of AE, months | Concomitant medication | Severity of event* | Stop of BA treatment | Resolved without sequelae |
|---|---|---|---|---|---|---|
| Etanercept (17 patients; 28.5 patient-years) | ||||||
| 1st | Crohn's disease | 12 | – | H | No | No |
| 1st | Restrictive pulmonary syndrome | 19 | Cs | H | Yes | No |
| 1st | ANCA-positive glomerulonephritis | 34 | Cs | H | Yes | No |
| 4th | Varicella infection | 4 | Cs, MTX | H | Temporarily | Yes |
| Abatacept (3 patients; 9.6 patient-years) | ||||||
| 3rd | Pyelonephritis | 1 | – | H | Temporarily | Yes |
| Anakinra (58 patients; 127.7 patient-years) | ||||||
| 1st | Macrophage activation syndrome | 1 | Cs | H | Yes | Yes |
| 1st | Salmonella infection | 34 | Cs | N | No | Yes |
| 1st | Varicella infection | 37 | Cs | D | Temporarily | Yes |
| 1st | Varicella infection | 20 | – | H | Temporarily | Yes |
| 1st | Mycoplasma pneumonia | 4 | Cs | H | Temporarily | Yes |
| 1st | Pneumonia | 21 | – | H | Temporarily | Yes |
| Canakinumab (30 patients; 48.7 patient-years) | ||||||
| 1st | CMV infection | 23 | – | H | No | Yes |
| 1st | Lymphadenitis | 20 | – | H | No | Yes |
| 1st | Eczema | 6 | – | D | No | Yes |
| 1st | Vulvitis | 25 | Cs | D | No | Yes |
| 2nd | Lyme disease | 32 | Cs | D | Temporarily | Yes |
| 2nd | Gastroenteritis | 16 | Cs, MTX | H | Temporarily | Yes |
| 2nd | Macrophage activation syndrome | 3 | Cs | H | Yes | Yes |
| 3rd | CMV infection | 5 | MTX | N | Temporarily | Yes |
| 4th | Varicella infection | 20 | Cs, MTX | N | Temporarily | Yes |
| Tocilizumab (20 patients; 27.9 patient-years) | ||||||
| 2nd | Crohn's disease | 13 | Cs | H | Yes | No |
| 3rd | Toxidermia | 5 | Cs | H | Yes | Yes |
| 4th | Cutaneous vasculitis | 14 | – | H | Yes | No |
| 4th | Infusion reaction | 0 | Cs | H | Yes | Yes |
*Severity of event: H=hospitalisation, D=temporary disruption of otherwise executable life functions, N=not clearly specified severity in medical records.
AE, adverse event; ANCA, anti-neutrophil cytoplasmic antibodies; BA, biological agent; CMV, cytomegalovirus; Cs, corticosteroids; MTX, methotrexate.
Discussion
This study describes drug survival and switch of BAs in patients with SJIA, and the achievement of inactive disease or clinical remission on different BAs in a setting of non-restricted access to different biological treatments at any point of clinical course.
In the present report, BA treatment allowed most patients to achieve inactive disease and more than half of the patients were in clinical remission at last follow-up.
Achievement of inactive disease and clinical remission has become a realistic goal for SJIA, with the increasing availability of BA. Studies addressing the clinical outcome in juvenile idiopathic arthritis that were published before introduction of BAs reported remission rates of 15–20% in SJIA.20 21 While treatment with TNF-α inhibitors showed significant improvement for patients with SJIA in terms of ACRpedi 30 or more, remission rates ranged from 13% to 38%.4 5 22 23 The introduction of IL-1 and IL-6 inhibitors increased the frequencies of ACRpedi 90 or inactive disease to about 60%, which is in accordance with our findings.5 12 14 24 25
Introducing an IL-1 or IL-6 inhibitor as the first BA appears to be the best option to increase the probability of achieving inactive disease in most patients. Early introduction of BAs may even prevent patients from receiving corticosteroids, as shown in a prospective study on 20 patients with SJIA with anakinra as first-line treatment.6 As in our study, anakinra has been most frequently used in recent years as the first BA in other observational studies.26 Anakinra, when used as a first BA, was associated with significantly longer drug survival as compared with etanercept. This is in accordance with the study of Tynjälä et al,24 who showed that a significant predictor of discontinuation of a first TNF-blocker therapy was SJIA compared with non-systemic JIA. Otten et al described significantly longer drug survival of anakinra compared with TNF blockers in SJIA when used as second BA after failure of etanercept. By contrast, drug survival of anakinra as a second/third BA was not different from etanercept as first BA.27 In our study, the response rate to anakinra was strikingly different between biological-naive and biological-experienced patients. Drug survival of anakinra as second/third BA was only 43% after 12 months of treatment, as compared with 63% on canakinumab and 82% on tocilizumab.
Switching to a second, third or fourth BA was common, and increased the frequency of inactive disease at last follow-up in two-thirds of the patients. However, in non-BA-naive patients, clinical remission was only achieved on canakinumab or tocilizumab. Also, in our study, the chance of achieving clinical remission after failing a first BA appears much lower.
Other studies addressing the effectiveness of switching to a second or third BA are scarce. In the study published by Otten et al,27 all patients with SJIA received etanercept as first BA. Switching was frequent, with 24 patients (47%) switched to a second BA (14 to anakinra, 8 on a second TNF blocker, 2 to a not further specified trial drug) and 13 patients switched to a third BA. The frequency of inactive disease was not reported. In accordance with our study, reasons for switch or discontinuation of TNF blockers were most frequently lack of effectiveness or intolerance.
In patients achieving clinical remission, withdrawing or tapering the dose of steroids was achieved in most cases. A recent study evaluating the long-term outcome of tocilizumab treatment in SJIA reported that a third of the patients were able to discontinue steroids.28 By contrast, only a few patients were able to withdraw BA treatment and maintain long-lasting clinical remission. The question of optimal tapering and eventual withdrawal of a BA in the face of inactive disease is still unanswered. De Benedetti et al reported results from an alternative dosing regimen for tocilizumab in patients with SJIA with inactive disease status and a 3-week interval followed by a 4-week interval. Twenty-six of a total 39 patients remained in clinically inactive disease during tapering, and 9 patients discontinued tocilizumab.29 In our centre, 12 out of 77 patients (15%) discontinued BA treatment for clinical remission, with 11 being treated with anakinra as the only BA.
The frequency of SAE in our study is consistent with other publications.14 30 31 No new SAE signals emerged during more than 240 patient-years under different BAs. For anakinra, canakinumab and abatacept, mainly infections were reported, whereas etanercept and tocilizumab were more frequently associated with non-infectious events in our study. Eight of nine reported non-infectious events led to BA withdrawal. Switching BA did not lead to further SAE at last follow-up.
Our study has several limitations. First, even when collected from a register, our data are of retrospective nature, and not all data were available at certain time points. Second, our results are mainly descriptive, as the small subsets of treatment groups without adjustments require caution when interpreting any direct comparisons. Third, CHAQ as proposed by Wallace et al,18 or other parameters of patient functional status were not systematically included. Future studies would potentially profit from the validated Juvenile Arthritis Disease Activity Score, as proposed by Consolaro et al.32 Fourth, follow-up duration was less than 1 year in some patients who switched BA, limiting long-term outcome data. Fifth, our population was followed in a tertiary centre, with a probable recruitment bias towards more severe cases.
In conclusion, IL-1 inhibitors were associated with a higher proportion of inactive disease than TNF inhibitors when used as first BA. Switching was an appropriate therapeutic approach, increasing the frequency of inactive disease and clinical remission when patients non-naïve from BA received canakinumab or tocilizumab. Complete remission was eventually achieved in more than half the patients. Long-term follow-up of patients with JIA and particularly patients with SJIA on BA will be provided by collaborative efforts such as the PharmaChild project.
Acknowledgments
The authors thank Caroline Elie, Clinical Research Unit, Hôpital Necker-Enfants Malades, Paris, France, for statistical support, and Solimda Sotou-Bere, Centre of Clinical Investigations, Hôpital Necker-Enfants Malades, Paris, France, for technical assistance.
Footnotes
Contributors: AW, BB-M and PQ were involved in study conception, design and data analysis. FU, IM and CW made contributions to data acquisition and analysis. RM made contributions to data acquisition. AW and PQ drafted the manuscript. All authors contributed in editing and reviewing the manuscript, and approved the final version of the paper.
Funding: This work was partially supported by a grant from Novartis SA, France.
Competing interests: PQ, BB-M and RM are investigators of clinical trials with etanercept, adalimumab, abatacept, tocilizumab and canakinumab. PQ received, outside the submitted work, research grants from Abbvie, BMS, Novartis, Pfizer and Roche, and speaker bureau or consultant for Abbvie, BMS, Novartis, Pfizer and Roche.
Ethics approval: French National Committee on Informatics and Liberty (CNIL).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Petty RE, Southwood TR, Manners P et al. International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol 2004;31:390–2. [PubMed] [Google Scholar]
- 2.Pascual V, Allantaz F, Arce E et al. Role of interleukin-1 (IL-1) in the pathogenesis of systemic onset juvenile idiopathic arthritis and clinical response to IL-1 blockade. J Exp Med 2005;201:1479–86. 10.1084/jem.20050473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mellins ED, Macaubas C, Grom AA. Pathogenesis of systemic juvenile idiopathic arthritis: some answers, more questions. Nat Rev Rheumatol 2011;7:416–26. 10.1038/nrrheum.2011.68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Quartier P, Taupin P, Bourdeaut F et al. Efficacy of etanercept for the treatment of juvenile idiopathic arthritis according to the onset type. Arthritis Rheum 2003;48:1093–101. 10.1002/art.10885 [DOI] [PubMed] [Google Scholar]
- 5.Horneff G, Schmeling H, Biedermann T et al. The German etanercept registry for treatment of juvenile idiopathic arthritis. Ann Rheum Dis 2004;63:1638–44. 10.1136/ard.2003.014886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vastert SJ, de Jager W, Noordman BJ et al. Effectiveness of first-line treatment with recombinant interleukin-1 receptor antagonist in steroid-naive patients with new-onset systemic juvenile idiopathic arthritis: results of a prospective cohort study. Arthritis Rheum 2014;66:1034–43. 10.1002/art.38296 [DOI] [PubMed] [Google Scholar]
- 7.Lequerre T, Quartier P, Rosellini D et al. Interleukin-1 receptor antagonist (anakinra) treatment in patients with systemic-onset juvenile idiopathic arthritis or adult onset Still disease: preliminary experience in France. Ann Rheum Dis 2008;67:302–8. 10.1136/ard.2007.076034 [DOI] [PubMed] [Google Scholar]
- 8.Nigrovic PA, Mannion M, Prince FH et al. Anakinra as first-line disease-modifying therapy in systemic juvenile idiopathic arthritis: report of forty-six patients from an international multicenter series. Arthritis Rheum 2011;63:545–55. 10.1002/art.30128 [DOI] [PubMed] [Google Scholar]
- 9.Gattorno M, Piccini A, Lasiglie D et al. The pattern of response to anti-interleukin-1 treatment distinguishes two subsets of patients with systemic-onset juvenile idiopathic arthritis. Arthritis Rheum 2008;58:1505–15. 10.1002/art.23437 [DOI] [PubMed] [Google Scholar]
- 10.Zeft A, Hollister R, LaFleur B et al. Anakinra for systemic juvenile arthritis: the Rocky Mountain experience. J Clin Rheumatol 2009;15:161–4. 10.1097/RHU.0b013e3181a4f459 [DOI] [PubMed] [Google Scholar]
- 11.Quartier P, Allantaz F, Cimaz R et al. A multicentre, randomised, double-blind, placebo-controlled trial with the interleukin-1 receptor antagonist anakinra in patients with systemic-onset juvenile idiopathic arthritis (ANAJIS trial). Ann Rheum Dis 2011;70:747–54. 10.1136/ard.2010.134254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ruperto N, Brunner HI, Quartier P et al. Two randomized trials of canakinumab in systemic juvenile idiopathic arthritis. New Engl J Med 2012;367:2396–406. 10.1056/NEJMoa1205099 [DOI] [PubMed] [Google Scholar]
- 13.De Benedetti F, Brunner HI, Ruperto N et al. Randomized trial of tocilizumab in systemic juvenile idiopathic arthritis. New Engl J Med 2012;367:2385–95. 10.1056/NEJMoa1112802 [DOI] [PubMed] [Google Scholar]
- 14.Lovell DJ, Giannini EH, Reiff AO et al. Long-term safety and efficacy of rilonacept in patients with systemic juvenile idiopathic arthritis. Arthritis Rheum 2013;65:2486–96. 10.1002/art.38042 [DOI] [PubMed] [Google Scholar]
- 15.Beukelman T, Patkar NM, Saag KG et al. 2011American College of Rheumatology recommendations for the treatment of juvenile idiopathic arthritis: initiation and safety monitoring of therapeutic agents for the treatment of arthritis and systemic features. Arthritis Care Res 2011;63:465–82. 10.1002/acr.20460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ringold S, Weiss PF, Beukelman T et al. 2013 update of the 2011 American College of Rheumatology recommendations for the treatment of juvenile idiopathic arthritis: recommendations for the medical therapy of children with systemic juvenile idiopathic arthritis and tuberculosis screening among children receiving biologic medications. Arthritis Care Res 2013;65:1551–63. 10.1002/acr.22087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Landais P, Messiaen C, Rath A et al. CEMARA an information system for rare diseases. Stud Health Technol Inform 2010;160(Pt 1):481–5. [PubMed] [Google Scholar]
- 18.Wallace CA, Giannini EH, Huang B et al. American College of Rheumatology provisional criteria for defining clinical inactive disease in select categories of juvenile idiopathic arthritis. Arthritis Care Res 2011;63:929–36. 10.1002/acr.20497 [DOI] [PubMed] [Google Scholar]
- 19.Wallace CA, Huang B, Bandeira M et al. Patterns of clinical remission in select categories of juvenile idiopathic arthritis. Arthritis Rheum 2005;52:3554–62. 10.1002/art.21389 [DOI] [PubMed] [Google Scholar]
- 20.Lomater C, Gerloni V, Gattinara M et al. Systemic onset juvenile idiopathic arthritis: a retrospective study of 80 consecutive patients followed for 10 years. J Rheumatol 2000;27:491–6. [PubMed] [Google Scholar]
- 21.Oen K. Long-term outcomes and predictors of outcomes for patients with juvenile idiopathic arthritis. Best Pract Res Clin Rheumatol 2002;16:347–60. 10.1016/S1521-6942(02)90233-0 [DOI] [PubMed] [Google Scholar]
- 22.Kimura Y, Pinho P, Walco G et al. Etanercept treatment in patients with refractory systemic onset juvenile rheumatoid arthritis. J Rheumatol 2005;32:935–42. [PubMed] [Google Scholar]
- 23.Prince FH, Twilt M, ten Cate R et al. Long-term follow-up on effectiveness and safety of etanercept in juvenile idiopathic arthritis: the Dutch national register. Ann Rheum Dis 2009;68:635–41. 10.1136/ard.2007.087411 [DOI] [PubMed] [Google Scholar]
- 24.Tynjälä P, Vahasalo P, Honkanen V et al. Drug survival of the first and second course of anti-tumour necrosis factor agents in juvenile idiopathic arthritis. Ann Rheum Dis 2009;68:552–7. 10.1136/ard.2007.087130 [DOI] [PubMed] [Google Scholar]
- 25.Singh-Grewal D, Schneider R, Bayer N et al. Predictors of disease course and remission in systemic juvenile idiopathic arthritis: significance of early clinical and laboratory features. Arthritis Rheum 2006;54:1595–601. 10.1002/art.21774 [DOI] [PubMed] [Google Scholar]
- 26.Otten MH, Anink J, Prince FHM et al. Trends in prescription of biological agents and outcomes of juvenile idiopathic arthritis: results of the Dutch national Arthritis and Biologics in Children Register. Ann Rheum Dis 2014. Published Online First: 18 Mar 2014. doi: 10.1136/annrheumdis-2013-204641 10.1136/annrheumdis-2013-204641 [DOI] [PubMed] [Google Scholar]
- 27.Otten MH, Prince FH, Anink J et al. Effectiveness and safety of a second and third biological agent after failing etanercept in juvenile idiopathic arthritis: results from the Dutch National ABC Register. Ann Rheum Dis 2013;72:721–7. 10.1136/annrheumdis-2011-201060 [DOI] [PubMed] [Google Scholar]
- 28.Yokota S, Imagawa T, Mori M et al. Longterm safety and effectiveness of the anti-interleukin 6 receptor monoclonal antibody tocilizumab in patients with systemic juvenile idiopathic arthritis in Japan. J Rheumatol 2014;41:759–67. 10.3899/jrheum.130690 [DOI] [PubMed] [Google Scholar]
- 29.De Benedetti F, Ruperto N, Brunner H et al. Tapering and withdrawal of tocilizumab in patients with systemic juvenile idiopathic arthritis in inactive disease: results from an alternative dosing regimen in the TENDER study. Arthritis Rheum 2014;66(Suppl 11):S8–9. 10.1002/art.38417 [DOI] [Google Scholar]
- 30.Horneff G, De Bock F, Foeldvari I et al. Safety and efficacy of combination of etanercept and methotrexate compared to treatment with etanercept only in patients with juvenile idiopathic arthritis (JIA): preliminary data from the German JIA Registry. Ann Rheum Dis 2009;68:519–25. 10.1136/ard.2007.087593 [DOI] [PubMed] [Google Scholar]
- 31.Lovell DJ, Reiff A, Ilowite NT et al. Safety and efficacy of up to eight years of continuous etanercept therapy in patients with juvenile rheumatoid arthritis. Arthritis Rheum 2008;58:1496–504. 10.1002/art.23427 [DOI] [PubMed] [Google Scholar]
- 32.Consolaro A, Ruperto N, Bazso A et al. Development and validation of a composite disease activity score for juvenile idiopathic arthritis. Arthritis Rheum 2009;61:658–66. 10.1002/art.24516 [DOI] [PubMed] [Google Scholar]