Abstract
Clinical application of anatomical and physiological knowledge of respiratory system improves patient's safety during anaesthesia. It also optimises patient's ventilatory condition and airway patency. Such knowledge has influence on airway management, lung isolation during anaesthesia, management of cases with respiratory disorders, respiratory endoluminal procedures and optimising ventilator strategies in the perioperative period. Understanding of ventilation, perfusion and their relation with each other is important for understanding respiratory physiology. Ventilation to perfusion ratio alters with anaesthesia, body position and with one-lung anaesthesia. Hypoxic pulmonary vasoconstriction, an important safety mechanism, is inhibited by majority of the anaesthetic drugs. Ventilation perfusion mismatch leads to reduced arterial oxygen concentration mainly because of early closure of airway, thus leading to decreased ventilation and atelectasis during anaesthesia. Various anaesthetic drugs alter neuronal control of the breathing and bronchomotor tone.
Keywords: Anatomy, bronchomotor tone, functional residual capacity, physiology, respiratory system, tracheobronchial tree, ventilation-perfusion
INTRODUCTION
Accurate knowledge of anatomy and physiology of the respiratory tract is important not only in the field of pulmonology but also in anaesthesiology and critical care. About 70–80% of the morbidity and mortality occurring in the perioperative period is associated with some form of respiratory dysfunction.[1] General anaesthesia and paralysis are associated with alterations in the respiratory function.[2,3] Dynamic anatomical changes and physiological alteration happening during anaesthesia make it imperative for an anaesthesiologist to have sound knowledge of the respiratory system and apply it for safe and smooth conduct of anaesthesia. Such knowledge has influence on clinical practice of airway management, lung isolation during anaesthesia, management of cases with respiratory disorders, respiratory endoluminal procedures and surgeries, optimising ventilator strategies in perioperative period and designing airway devices.
ANATOMY OF RESPIRATORY SYSTEM
The respiratory system, functionally, can be separated in two zones; conducting zones (nose to bronchioles) form a path for conduction of the inhaled gases and respiratory zone (alveolar duct to alveoli) where the gas exchange takes place. Anatomically, respiratory tract is divided into upper (organ outside thorax - nose, pharynx and larynx) and lower respiratory tract (organ within thorax - trachea, bronchi, bronchioles, alveolar duct and alveoli).
The discussion is mainly concentrated on the lower respiratory tract and the related physiology.
Nose and nasal cavity are divided into two halves by the nasal septum. The lateral wall of the nose consists of three turbinates or conchae (superior, middle and inferior). The passage inferior to inferior turbinate is preferred passage for nasotracheal intubation.[4] The pharynx is a tube-like passage that connects the posterior nasal and oral cavities to the larynx and oesophagus. It is divided into nasopharynx, oropharynx and laryngopharynx. Increase in soft tissue within bony enclosure of pharynx or decrease in bony enclosure size would result in anatomical imbalance and cause limitation of space available for airway [Figure 1].[5]
Figure 1.
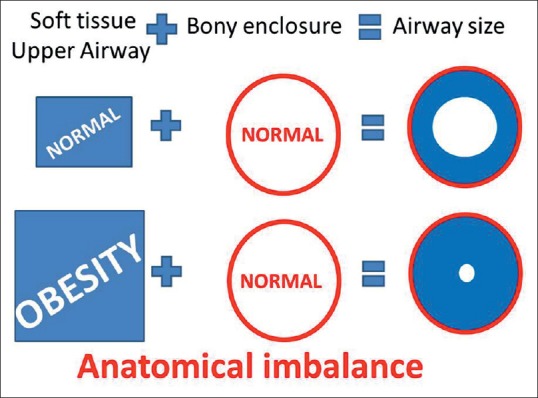
Excessive soft tissue (obesity) in fix bony enclosure leads to compromised pharyngeal passage
There are three narrowest portions of pharynx; passage posterior to the soft palate (retro palatal space), passage posterior to the tongue (retroglossal space) and passage posterior to epiglottis (retroepiglotic space). There is significant reduction of these spaces with sedation and anaesthesia[6] which would lead to upper airway obstruction.
ANATOMICAL FACTORS WHICH COMPROMISES PHARYNGEAL PATENCY
Inefficient contraction of pharyngeal dilator muscles [Figure 2]
Figure 2.
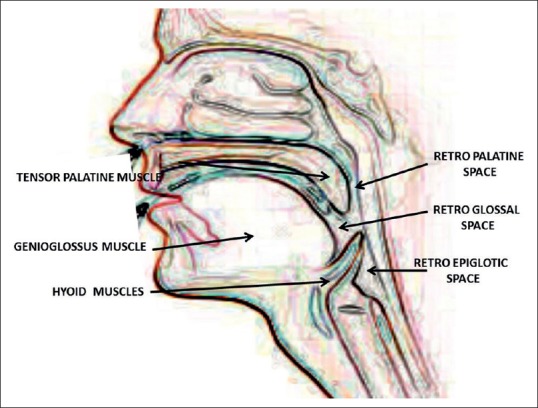
Upper airway showing pharyngeal dilator muscles and pharyngeal airway space
(1) The tensor palatine retracts the soft palate away from the posterior pharyngeal wall, thereby maintaining retro palatal patency. (2) The genioglossus moves the tongue anteriorly to open the retroglossal space. (3) Hyoid muscles (geniohyoid, sternohyoid and thyrohyoid) make the hyoid move anteriorly and stabilise the retroepiglotic laryngopharynx. Excessive fat deposition around these muscles would result in inefficient contraction of pharyngeal dilator muscles. This would lead to pharyngeal airway obstruction during sedation and anaesthesia.[7]
Anatomical imbalance of oropharyngeal soft tissue
Enlarged tongue (in the case of acromegaly or obesity) in normal bony enclosure of oropharynx or a smaller bony enclosure (receding mandible) of oropharynx would be unable to accommodate the tongue into oropharynx and thus shift the tongue into hypopharynx (laryngopharynx). Hypo pharyngeal tongue decreases laryngopharyngeal airway patency. This is one reason for obstructive sleep apnoea and difficult mask ventilation during anaesthesia.[8]
Tracheal tug
There is constant traction on trachea, pharynx and larynx during inspiration because of negative intrathoracic pressure which elongates pharyngeal airway during inspiration that would result in decreased pharyngeal luminal space in obese patients. This is also one of the reasons for difficult mask ventilation and obstructive sleep apnoea.[9]
Larynx
It serves as a sphincter, transmitting air from oropharynx and nasopharynx to trachea.
TRACHEOBRONCHIAL TREE
It is a complex system that transports gases from the trachea down to the acini, the gas exchange units of the lung. It is partitioned into 23 generations of dichotomous branching, extending from trachea (generation 0) to the last order of terminal bronchioles (generation 23). At each generation, each airway is being divided into two smaller daughter airways[10] [Figure 3].
Figure 3.
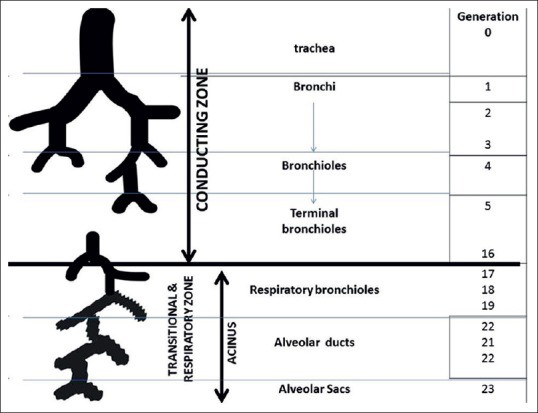
Tracheobronchial tree showing 23 generations
From the trachea to the terminal bronchioles (generation 15–16), the airways are purely conducting pipes. Since no gas exchanges take place in this region, the volume in these pipes is called as the dead space volume (average 150 ml). The terminal bronchioles (generation 16) divide into respiratory bronchioles or transitional bronchioles (generations 17–19) as they have occasional alveoli at the walls. These respiratory bronchioles further divide into alveolar ducts (generations 20–22) which are completely lined with alveoli. This region is known as acinus (generations 16–23). The acinus is comprised of respiratory airways and forms functional tissues (gas exchange units) of lung. The alveolar ducts are small tubes supported by a rich matrix of elastic and collagen fibres. The distal ends of alveolar ducts open into the alveolar sac which is made up by alveoli.
TRACHEA AND RIGHT/LEFT MAIN BRONCHUS
The trachea is a hollow conduit for gases and bronchial secretions. It extends from the level of C6 (cricoid cartilage) to the carina, approximately located at the level of T4–T5.[11] In adults, its length is approximately 11–13 cm, with 2–4 cm being extra-thoracic.[12] The trachea has 16 to 22 horseshoe bands (c-shaped) of cartilages. The posterior tracheal wall lacks cartilage and is supported by the trachealis muscle. Depending on the level of inspiration, the posterior wall of the trachea becomes flat, convex or slightly concave.[13,14] The posterior wall of the trachea either flattens or bows slightly forward during expiration. In normal subjects, there is up to 35% reduction in antero-posteior tracheal lumen in forced expiration, whereas the transverse diameter decreases only by 13%.[15] The trachea is generally midline in position, often displaced slightly to the right and posteriorly as it approaches carina. The angle of the tracheal bifurcation is called as the carinal/subcarinal angle, which is measured commonly as 73° (35–90°).[16,17,18] The carinal angle is wider in individuals with an enlarged left atrium, in females and obese patients.
The trachea divides at carina into the right and left main bronchus. The distance of the carina from the teeth varies markedly with change in neck position from flexion to extension (tracheal length variation is ± 2 cm), body position and position of diaphragm.[19] This explains the change in position of endotracheal tube during change in position of patient or flexion – extension of neck. The right main stem bronchus has a more direct downward course, is shorter than the left and begins to ramify earlier than the left main bronchus.[11] This leads to higher chances of right endobronchial intubation. The right main stem bronchus divides into (secondary bronchi) right upper lobe bronchus and bronchus intermedius which further divides into right middle and lower lobe bronchus. The left bronchus passes inferolaterally at a greater angle from the vertical axis than the right bronchus. The left main stem bronchus divides into (secondary bronchi) the left upper and lower lobe bronchi.
BRONCHO-PULMONARY SEGMENT
Broncho-pulmonary segment may be defined as an area of distribution of any bronchus [Figure 4]. Each lobar bronchi divides into segmental bronchi (tertiary bronchi), which supply the broncho-pulmonary segment of each lobe. Technically, there are ten broncho-pulmonary segments in each lung, but in left lung, some of these segments fuse and there are as few as eight broncho-pulmonary segments. The bronchi continue to divide into smaller and smaller bronchi up to 23 generations of divisions from main bronchus. As bronchi become smaller, their structure changes:
Figure 4.
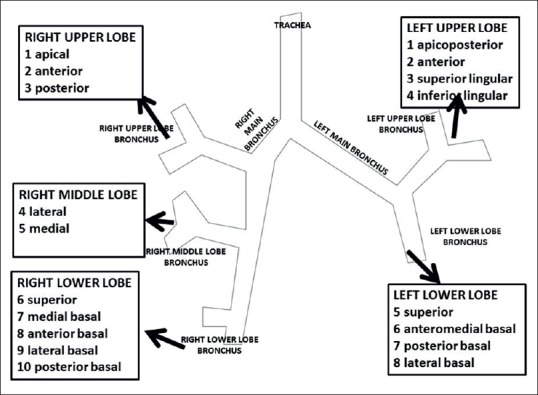
Tracheobronchial tree with broncho-pulmonary segments
Cartilaginous ring becomes irregular and then disappear. When bronchi lose all cartilaginous support, the airway is then referred as bronchioles
The epithelium changes from pseudostratified columnar to columnar to cuboidal in the terminal bronchioles
There are no cilia and mucous producing cells in bronchioles
The amount of smooth muscle in the tube wall increases as the airway becomes smaller.
DIMENSIONS OF TRACHEOBRONCHIAL TREE [TABLE 1]
Table 1.
Dimensions and features of tracheobronchial tree
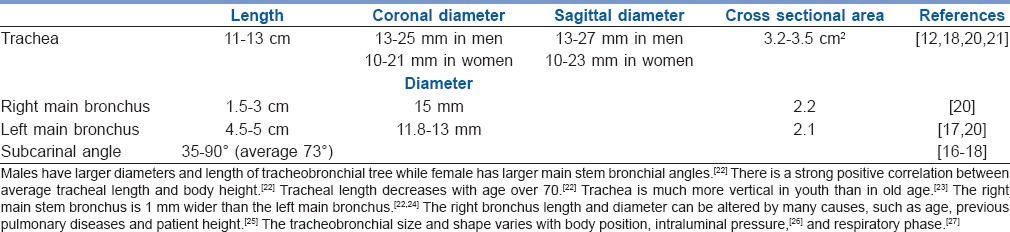
Ascertaining the parameters of tracheobronchial tree such as length, diameters and angulations helps optimizing procedures such as intubation, lung isolation techniques and jet ventilation during interventional endoscopic surgeries of trachea or bronchi.[20]
Tracheobronchial anatomical variations
Tracheobronchial tree exhibits a wide range of variations and its prevalence is 4%.[28] The most common main bronchus anomalies are the tracheal bronchus and the accessory cardiac bronchus. Knowledge of tracheobronchial variants is important for clinical aspect in pre-operative evaluation in view of intubation, lung isolation techniques and other endo-bronchial procedures.
Tracheal bronchus
This is a bronchus usually originating from the right side of the trachea above the carina and within 2–6 cm from it.[29] Right tracheal bronchus has a prevalence of 0.1–2% and left bronchus has a prevalence of 0.3–1%.[30,31,32,33,34] The tracheal bronchus may cause complications such as atelectasis or pneumothorax in the cases of obstruction to its entrance or tube entering into it during intubation.[35,36,37]
Accessory cardiac bronchus
It is a congenital, short and thin bronchus towards pericardium originating either from right bronchus or intermediate bronchus. Its prevalence is 0.08%.[31] It is associated with recurrent infections in few cases.[38]
PHYSIOLOGY OF RESPIRATORY SYSTEM
Movement of inspired gas into and exhaled gas out of lung is called as ventilation. Understanding of lung volumes, lung compliance, ventilation-perfusion and bronchomotor tone are essential for clinical application of respiratory physiology in anaesthesia and critical care.
Lung volumes [Figure 5]
Figure 5.
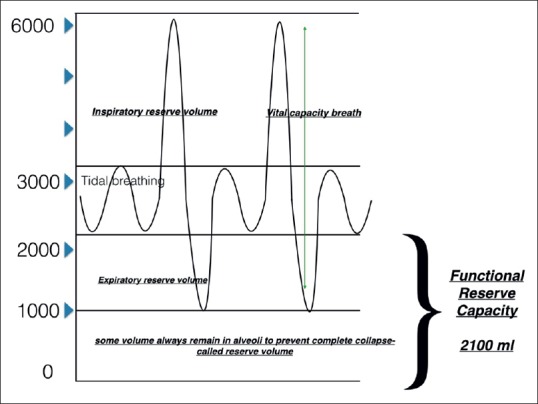
Lung volumes
Normal requirements of the body can be easily met by normal tidal ventilation which is approximately 4–8 ml/kg. Body has kept mechanism to provide extra ventilation in the form of inspiratory reserve volume and expiratory reserve volume whenever required (e.g., exercise). When an individual, after tidal expiration, takes full inspiratory breath followed by expiration to reserve volume, it is called as vital capacity breath and is 4–5 L in an average 70 kg individual. There is always some amount of air remaining in the alveoli which prevents it from collapsing. The volume remaining in the lungs after vital capacity breath is called as residual volume.
Residual volume with expiratory reserve volume is called as functional residual capacity (FRC). FRC is basically the amount of air in the lungs after a normal expiration. Gases remaining in the lungs at the end of expiration not only prevent alveolar collapse but also it continues to oxygenate the pulmonary blood flowing though the capillaries during this time period.[39] Reported FRC values vary with various reports but on average it is between 2.8 and 3.1 L[40] in standing position. FRC varies with change of position, anaesthesia and body weight. FRC is the reserve which prolongs non-hypoxic apnoea time.
The portion of the minute ventilation which reaches alveoli and takes part in the gas exchange is called as alveolar ventilation. Normal value of alveolar ventilation is approximately 5 L/min which is similar to the volume of blood flowing through the lung (cardiac output 5 L/min). This makes alveolar ventilation to perfusion ratio approximately one.[39]
RESPIRATORY MECHANICS
Lungs are like inflatable balloon which distend actively by positive pressure inside and/or negative pressure created in pleural space. In normal respiration, negative pleural pressure (Ppl) is sufficient to distend the lungs during inspiratory phase. Understanding of distending pressure is very important to understand the respiratory mechanics. Distending pressure can be known as transpulmonary pressure (Ptp), which is expressed by the following equation:
Ptp = Paw−Ppl, (Ptp = transpulmonary pressure, Paw = alveolar pressure, Ppl = Pleural pressure).
Compliance and ventilation of lung
Compliance is expressed as the distension of lung for a given level of Ptp. It is usually 0.2–0.3 L/cm H2O.[41] Compliance (ability of lung to distend) depends upon the volume of the lung. Compliance is lowest at extremes of FRC. It implies that expanded lung and completely deflated lung has lower capacity to distend to a given pressure [Figure 6]. In the upright lung, intra-Ppl varies from the top to the base of the lungs. Intra-Ppl becomes 0.2 cm H2O positive for every centimetre distance from apex to base of lung. Average height of lung is about 35 cm. In quite breathing, the intra-Ppl at apex is about − 8 cm of H2O while at base it is − 1.5 cm of H2O. This means that the alveoli at the apex are exposed to a greater distending pressure (PA−Ppl = 0 − (−8) =8 cm H2O) compared to those at the base (PA−Ppl = 0 − (−1.5) =1.5 cm H2O). As already distended, apical region becomes less compliant than other area of lung. This explains the preferential distribution of ventilation to the alveoli at the base of the lungs in upright posture. Distribution of ventilation changes with the position of individual because of the change of Ppl with the gravity.
Figure 6.
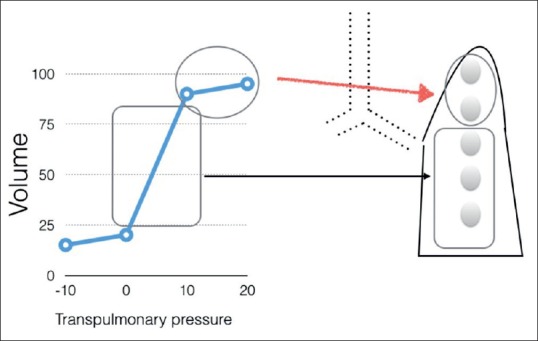
Transpulmonary pressure
Airway closure during expiration is normal phenomenon, with reopening of airways during the succeeding inspiration.[42] The volume remaining above the residual volume where expiration below FRC closes some airways is termed as closing volume and this volume added to the residual volume is termed as the closing capacity. In upright position, closing capacity approaches near FRC in older individual (65–70 years) which would result in airway closure even at normal tidal expiration. Change in body position from upright to supine, lateral or prone reduces FRC. Reduction in FRC promotes airway closure in dependent lung regions. Early airway closure thus decreases ventilation in the dependent regions. Since lung blood flow passes preferentially to dependent regions, matching between ventilation and perfusion is impeded.[43]
Perfusion of lung
Pulmonary circulation differs from systemic circulation. The pulmonary vessels are thin-walled and have less musculature to assist fast diffusion of gases. They are subjected to less pressure compared to systemic circulation. Because of less pressure and structural differences of pulmonary vasculature to assist diffusion, they are subjected to Paw inside the thorax and gravity.[44]
On the basis of the influence of gravity, perfusion of lung is divided into three zones.[45] The distribution of blood flow in these zones depends upon three factors: Alveolar pressure (PA), pulmonary arterial pressure (Pa) and pulmonary venous pressure (Pv).
Apical region where PA can be higher than Pa and Pv is considered as zone I. Since PA > Pa > Pv in zone I, no arterial blood flow occurs and this zone is considered as physiological dead space. Though such zone I do not exist in healthy subject under normal perfusion pressure, in condition of haemorrhage or positive pressure, ventilation zone I may become reality and adds to dead space ventilation.
In middle zone or zone II, difference of Pa to PA decides the perfusion (Pa > PA > Pv) while in lower zone or zone III, difference of Pa to Pv (Pa > Pv > PA) decides the perfusion. Few studies also include 4th zone of less blood supply because of the compression of vessels due to the weight of lungs.[46]
The zones described earlier are purely physiological and not anatomical. The borders between zones changes with many physiological and pathophysiological alterations or conditions. Paw changes are minimal during the course of a quiet breath but they are much greater during speech, exercise and other conditions. The patients on positive pressure ventilation with positive end expiratory pressure (PEEP) may have substantial zone I due to high PAs. Pa alters with severe haemorrhage or during general anaesthesia resulting in zone I conditions. Pulmonary artery pressure is high during exercise, eliminating any existing zone I into zone II and moving the boundary between zones III and II upward
Ventilation to perfusion matching
The alveolar partial pressure of oxygen and carbon dioxide are determined by the ratio of ventilation (V) to perfusion (Q). As discussed earlier, ventilation and perfusion both increase from top to bottom in lungs, but perfusion increases more in comparison to ventilation.
Proportionately, ratio of ventilation to perfusion is more in upper lung and less towards the base of lungs [Figure 7]. This gradient occurs in vertical axis of the lung fields irrespective of body positions. (i.e., if patient is in upright posture, apex has more ventilation while base has more perfusion. If patient is in lateral posture, nondependent lung gets more ventilation while dependent lung gets more perfusion).
Figure 7.
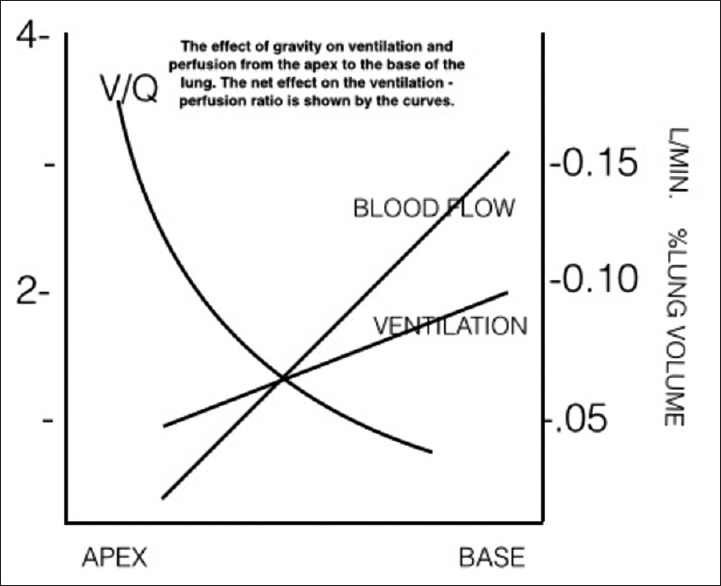
Ventilation perfusion ratio from apex to the base of lung
HYPOXIC PULMONARY VASOCONSTRICTION
Hypoxic pulmonary vasoconstriction (HPV) is compensatory blood flow away from hypoxic lung regions to better oxygenated regions. HPV occurs in response to low alveolar oxygen tension. This mechanism improves the V/Q mismatch. All inhalation agents except newer agents, sevoflurane and desflurane, inhibit the HPV.[39]
PHYSIOLOGICAL VARIATION WITH POSITION AND ANAESTHESIA
Supine position
General anaesthesia promotes basal atelectasis irrespective of the modes of ventilation (spontaneous or controlled) or drugs (intravenous or inhalation) used. Nearly, 15–20% of the lung is atelectatic during general anaesthesia. Atelectasis decreases towards the apex, which usually remains aerated.[42] The area of atelectasis becomes the area of shunt where no gas exchange occurs in spite of perfusion. Early airway closure in tidal breathing with supine position, promotes ventilation perfusion mismatch (V/Q < 1) and impairment of gas exchange. The combination of atelectasis and airway closure explains about 75% of the overall impairment in oxygenation in anaesthetised subject.[47]
Lateral position and one-lung ventilation
Anaesthesia in lateral position causes ventilation perfusion mismatch where upper or nondependent lung receives more ventilation and lower or dependent lung receives higher (60–65%) perfusion. Dependent lung also exhibits signs of early airway closure and formation of atelectasis. With addition of PEEP, almost 80% of blood flow is directed to lower dependent lung.[47] During one-lung ventilation, HPV can divert blood flow away from the non-ventilated lung. One should avoid drugs causing inhibition of HPV.
Prone position
Prone position decreases ventilation perfusion mismatch and improves the oxygenation. Various reasons (e.g., uniform vertical distribution of perfusion, better ventilation distribution because of smaller vertical pleural gradient, increased FRC, more uniform gas distribution and less lung compression by heart) have been proposed by different authors for improvement in ventilation with prone position. There are no reports of atelectasis in prone position, probably because weight of heart transferred on the sternum instead of lungs as opposed to supine position.[42]
NEUROLOGICAL CONTROL OF BREATHING
The respiratory centres are located in pons and medulla. They contain different types of inspiratory and expiratory neurons that fire during the three phases of the respiratory cycle, namely inspiratory phase of sudden discharge of signals to inspiratory muscles and the dilator muscles of the pharynx, followed by gradual decline of signals in post-inspiratory phase. Inspiration is followed by no signals in expiratory phase except in forced expiration or high minute ventilation.[48] Inhalational agents influence rate, rhythm and intensity of discharge from the respiratory centres which receive inputs from the chemoreceptors, cortex, hypothalamus, pharyngeal mechanoreceptors, vagus nerve and other afferents. Peripheral chemoreceptors respond quickly to hypoxia, hypercapnia and hydrogen ion concentration. The central chemoreceptors are slow responders relative to peripheral chemoreceptors.
BRONCHOMOTOR TONE
Bronchomotor tone is the state of contraction or relaxation of the smooth muscle in the bronchial walls that regulates the calibre of the airways. Number of factors influences the change of bronchomotor tone, e.g. depth of anaesthesia, drugs and various procedures on airway, respiratory diseases (bronchial asthma) and inhalational agents. Using computed tomography, Brown et al. had showed that halothane causes greater broncho-dilatation than isoflurane at low concentrations.[49] Sevoflurane (1 minimum alveolar concentration) reduced respiratory system resistance (determined using an isovolume technique) by 15% in patients undergoing elective surgery. In contrast, desflurane did not significantly alter resistance.[50]
SUMMARY
Clinical application of the anatomical knowledge of respiratory system definitely improves safety of conduct of anaesthesia and also optimises patient ventilatory condition and airway patency. Such knowledge has influence on the clinical practice of airway management, lung isolation during anaesthesia, management of cases with respiratory disorders, respiratory endoluminal procedures and surgeries, optimising ventilator strategies in perioperative period, applying jet ventilation during emergency and endoluminal surgeries and designing airway devices.
An anaesthesiologist should understand that FRC is the most important parameter. Its relation with closing capacity is an important determinant of ventilation of patient. Ventilation and perfusion both are affected by the gravity. Overall ventilation to perfusion ratio is 1 but it alters with anaesthesia, body positions and with one-lung anaesthesia. HPV, an important safety mechanism, is inhibited by majority of anaesthetic drugs. Ventilation perfusion mismatch leading to reduced arterial oxygen concentration is mainly because of early closure of airway leading to decreased ventilation and atelectasis occurring with the anaesthesia. Various anaesthetic drugs alter neuronal control of the breathing and bronchomotor tone.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Drain CB. Physiology of respiratory system related to anesthesia. CRNA. 1996;7:163–80. [PubMed] [Google Scholar]
- 2.Brismar B, Hedenstierna G, Lundquist H, Strandberg A, Svensson L, Tokics L. Pulmonary densities during anesthesia with muscular relaxation – A proposal of atelectasis. Anesthesiology. 1985;62:422–8. doi: 10.1097/00000542-198504000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Hedenstierna G. Gas exchange during anaesthesia. Acta Anaesthesiol Scand Suppl. 1990;94:27–31. doi: 10.1111/j.1399-6576.1990.tb03218.x. [DOI] [PubMed] [Google Scholar]
- 4.Ahmed-Nusrath A, Tong JL, Smith JE. Pathways through the nose for nasal intubation: A comparison of three endotracheal tubes. Br J Anaesth. 2008;100:269–74. doi: 10.1093/bja/aem350. [DOI] [PubMed] [Google Scholar]
- 5.Watanabe T, Isono S, Tanaka A, Tanzawa H, Nishino T. Contribution of body habitus and craniofacial characteristics to segmental closing pressures of the passive pharynx in patients with sleep-disordered breathing. Am J Respir Crit Care Med. 2002;165:260–5. doi: 10.1164/ajrccm.165.2.2009032. [DOI] [PubMed] [Google Scholar]
- 6.Shorten GD, Opie NJ, Graziotti P, Morris I, Khangure M. Assessment of upper airway anatomy in awake, sedated and anaesthetised patients using magnetic resonance imaging. Anaesth Intensive Care. 1994;22:165–9. doi: 10.1177/0310057X9402200208. [DOI] [PubMed] [Google Scholar]
- 7.Benumof JL. Obstructive sleep apnea in the adult obese patient: Implications for airway management. Anesthesiol Clin North America. 2002;20:789–811. doi: 10.1016/s0889-8537(02)00020-2. [DOI] [PubMed] [Google Scholar]
- 8.Chou HC, Wu TL. Large hypopharyngeal tongue: A shared anatomic abnormality for difficult mask ventilation, difficult intubation, and obstructive sleep apnea? Anesthesiology. 2001;94:936–7. doi: 10.1097/00000542-200105000-00043. [DOI] [PubMed] [Google Scholar]
- 9.Isono S. Obesity and obstructive sleep apnoea: Mechanisms for increased collapsibility of the passive pharyngeal airway. Respirology. 2012;17:32–42. doi: 10.1111/j.1440-1843.2011.02093.x. [DOI] [PubMed] [Google Scholar]
- 10.Weibel ER. Morphometry of the Human Lung. Berlin, Heidelberg: Springer; 1963. Geometry and dimensions of airways of conductive and transitory zones; pp. 110–35. [Google Scholar]
- 11.Minnich DJ, Mathisen DJ. Anatomy of the trachea, carina, and bronchi. Thorac Surg Clin. 2007;17:571–85. doi: 10.1016/j.thorsurg.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 12.Webb EM, Elicker BM, Webb WR. Using CT to diagnose nonneoplastic tracheal abnormalities: Appearance of the tracheal wall. AJR Am J Roentgenol. 2000;174:1315–21. doi: 10.2214/ajr.174.5.1741315. [DOI] [PubMed] [Google Scholar]
- 13.Ugalde P, Miro S, Fréchette E, Deslauriers J. Correlative anatomy for thoracic inlet; glottis and subglottis; trachea, carina, and main bronchi; lobes, fissures, and segments; hilum and pulmonary vascular system; bronchial arteries and lymphatics. Thorac Surg Clin. 2007;17:639–59. doi: 10.1016/j.thorsurg.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 14.Ederle JR, Heussel CP, Hast J, Fischer B, Van Beek EJ, Ley S, et al. Evaluation of changes in central airway dimensions, lung area and mean lung density at paired inspiratory/expiratory high-resolution computed tomography. Eur Radiol. 2003;13:2454–61. doi: 10.1007/s00330-003-1909-5. [DOI] [PubMed] [Google Scholar]
- 15.Boiselle PM, Reynolds KF, Ernst A. Multiplanar and three-dimensional imaging of the central airways with multidetector CT. AJR Am J Roentgenol. 2002;179:301–8. doi: 10.2214/ajr.179.2.1790301. [DOI] [PubMed] [Google Scholar]
- 16.Karabulut N. CT assessment of tracheal carinal angle and its determinants. Br J Radiol. 2005;78:787–90. doi: 10.1259/bjr/75107416. [DOI] [PubMed] [Google Scholar]
- 17.Chunder R, Guha R. A morphometric study of human subcarinal angle in different age groups in both sexes and its clinical implications. Indian J Basic Appl Med Res. 2015;4:424–30. [PubMed] [Google Scholar]
- 18.Haskin PH, Goodman LR. Normal tracheal bifurcation angle: A reassessment. AJR Am J Roentgenol. 1982;139:879–82. doi: 10.2214/ajr.139.5.879. [DOI] [PubMed] [Google Scholar]
- 19.Cherng CH, Wong CS, Hsu CH, Ho ST. Airway length in adults: Estimation of the optimal endotracheal tube length for orotracheal intubation. J Clin Anesth. 2002;14:271–4. doi: 10.1016/s0952-8180(02)00355-0. [DOI] [PubMed] [Google Scholar]
- 20.Breatnach E, Abbott GC, Fraser RG. Dimensions of the normal human trachea. AJR Am J Roentgenol. 1984;142:903–6. doi: 10.2214/ajr.142.5.903. [DOI] [PubMed] [Google Scholar]
- 21.Brock RC. The anatomy of the bronchial tree. AMA Arch Otolaryngol. 1958;68:454–9. doi: 10.1001/archotol.1958.00730020472008. [DOI] [PubMed] [Google Scholar]
- 22.Mi W, Zhang C, Wang H, Cao J, Li C, Yang L, et al. Measurement and analysis of the tracheobronchial tree in Chinese population using computed tomography. PLoS One. 2015;10:e0123177. doi: 10.1371/journal.pone.0123177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grillo HC. Diseases, Diagnosis, Results of Treatment. London: BC Decker Inc; 2004. Surgery of the Trachea and Bronchi; pp. 43–51. [Google Scholar]
- 24.Seymour AH. The relationship between the diameters of the adult cricoid ring and main tracheobronchial tree: A cadaver study to investigate the basis for double-lumen tube selection. J Cardiothorac Vasc Anesth. 2003;17:299–301. doi: 10.1016/s1053-0770(03)00057-0. [DOI] [PubMed] [Google Scholar]
- 25.Otoch JP, Minamoto H, Perini M, Carneiro FO, de Almeida Artifon EL. Is there a correlation between right bronchus length and diameter with age? J Thorac Dis. 2013;5:306–9. doi: 10.3978/j.issn.2072-1439.2013.03.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Griscom NT, Wohl ME. Tracheal size and shape: Effects of change in intraluminal pressure. Radiology. 1983;149:27–30. doi: 10.1148/radiology.149.1.6611936. [DOI] [PubMed] [Google Scholar]
- 27.Wittenborg MH, Gyepes MT, Crocker D. Tracheal dynamics in infants with respiratory distress, stridor, and collapsing trachea. Radiology. 1967;88:653–62. doi: 10.1148/88.4.653. [DOI] [PubMed] [Google Scholar]
- 28.Abakay A, Tanrikulu AC, Sen HS, Abakay O, Aydin A, Carkanat AI, et al. Clinical and demographic characteristics of tracheobronchial variations. Lung India. 2011;28:180–3. doi: 10.4103/0970-2113.83973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ghaye B, Szapiro D, Fanchamps JM. Congenital bronchial abnormalities revisited. Radiographics. 2001;21:105–19. doi: 10.1148/radiographics.21.1.g01ja06105. [DOI] [PubMed] [Google Scholar]
- 30.Horton KM, Horton MR, Fishman EK. Advanced visualization of airways with 64-MDCT: 3D mapping and virtual bronchoscopy. AJR Am J Roentgenol. 2007;189:1387–96. doi: 10.2214/AJR.07.2824. [DOI] [PubMed] [Google Scholar]
- 31.Saad C, Metha A. Accessory cardiac bronchus. J Bronchology. 2002;9:311–2. [Google Scholar]
- 32.Ghaye B, Szapiro D, Fanchamps JM, Dondelinger RF. Congenital bronchial abnormalities revisited. Radiographics. 2001;1:105–19. doi: 10.1148/radiographics.21.1.g01ja06105. [DOI] [PubMed] [Google Scholar]
- 33.Beder S, Küpeli E, Karnak D, Kayacan O. Tracheobronchial variations in Turkish population. Clin Anat. 2008;21:531–8. doi: 10.1002/ca.20667. [DOI] [PubMed] [Google Scholar]
- 34.Khurshid I, Anderson LC, Downie GH. Tracheal accessory lobe take-off and quadrifurcation of right upper lobe bronchus: A rare tracheobronchial anomaly. J Bronchology. 2003;10:58–60. [Google Scholar]
- 35.Conacher ID. Implications of a tracheal bronchus for adult anaesthetic practice. Br J Anaesth. 2000;85:317–20. doi: 10.1093/bja/85.2.317. [DOI] [PubMed] [Google Scholar]
- 36.Ikeno S, Mitsuhata H, Saito K, Hirabayashi Y, Akazawa S, Kasuda H, et al. Airway management for patients with a tracheal bronchus. Br J Anaesth. 1996;76:573–5. doi: 10.1093/bja/76.4.573. [DOI] [PubMed] [Google Scholar]
- 37.Aoun NY, Velez E, Kenney LA, Trayner EE. Tracheal bronchus. Respir Care. 2004;49:1056–8. [PubMed] [Google Scholar]
- 38.Ghaye B, Kos X, Dondelinger RF. Accessory cardiac bronchus: 3D CT demonstration in nine cases. Eur Radiol. 1999;9:45–8. doi: 10.1007/s003300050625. [DOI] [PubMed] [Google Scholar]
- 39.Kavanach B, Hedenstierna G. Respiratory physiology and pathophysiology. In: Miller RD, editor. Miller's Anesthesia. 8th ed. Philadelphia: Elsevier; 2015. pp. 444–72. [Google Scholar]
- 40.Roca J, Burgos F, Barberà JA, Sunyer J, Rodriguez-Roisin R, Castellsagué J, et al. Prediction equations for plethysmographic lung volumes. Respir Med. 1998;92:454–60. doi: 10.1016/s0954-6111(98)90291-8. [DOI] [PubMed] [Google Scholar]
- 41.Grassino AE, Roussos C, Macklem PT. The Lung: Scientific Foundations. 2nd ed. New York: New Raven; 1997. Static properties of the lung and chest wall; pp. 1187–202. [Google Scholar]
- 42.Hedenstierna G. Effects of body position on ventilation/perfusion matching. In: Gulio A, editor. Anaesthesia, Pain, Intensive Care and Emergency Medicine–A.P.I.C.E. Milan: Springer; 2005. pp. 3–15. [Google Scholar]
- 43.Hedenstierna G, Baehrendtz S, Klingstedt C, Santesson J, Söderborg B, Dahlborn M, et al. Ventilation and perfusion of each lung during differential ventilation with selective PEEP. Anesthesiology. 1984;61:369–76. doi: 10.1097/00000542-198410000-00003. [DOI] [PubMed] [Google Scholar]
- 44.Hughes M, West JB. Last word on point: Counterpoint: Gravity is/is not the major factor determining the distribution of blood flow in the human lung. J Appl Physiol. 2008;104:1539. doi: 10.1152/japplphysiol.90374.2008. [DOI] [PubMed] [Google Scholar]
- 45.West JB, Dollery CT, Naimark A. Distribution of blood flow in isolated lung; relation to vascular and alveolar pressures. J Appl Physiol. 1964;19:713–24. doi: 10.1152/jappl.1964.19.4.713. [DOI] [PubMed] [Google Scholar]
- 46.Hughes JM, Glazier JB, Maloney JE, West JB. Effect of lung volume on the distribution of pulmonary blood flow in man. Respir Physiol. 1968;4:58–72. doi: 10.1016/0034-5687(68)90007-8. [DOI] [PubMed] [Google Scholar]
- 47.Rothen HU, Sporre B, Engberg G, Wegenius G, Hedenstierna G. Airway closure, atelectasis and gas exchange during general anaesthesia. Br J Anaesth. 1998;81:681–6. doi: 10.1093/bja/81.5.681. [DOI] [PubMed] [Google Scholar]
- 48.Mills GH. Respiratory physiology and anaesthesia. Br J Anesth CEPD Rev. 2001;1:35–9. [Google Scholar]
- 49.Brown RH, Zerhouni EA, Hirshman CA. Comparison of low concentrations of halothane and isoflurane as bronchodilators. Anesthesiology. 1993;78:1097–101. doi: 10.1097/00000542-199306000-00012. [DOI] [PubMed] [Google Scholar]
- 50.Goff MJ, Arain SR, Ficke DJ, Uhrich TD, Ebert TJ. Absence of bronchodilation during desflurane anesthesia: A comparison to sevoflurane and thiopental. Anesthesiology. 2000;93:404–8. doi: 10.1097/00000542-200008000-00018. [DOI] [PubMed] [Google Scholar]


