Sir
As per the estimates of the World Health Organization (WHO) worldwide more than half of all the medicines are prescribed, dispensed or sold inappropriately and about one-third of the world's population lack access to essential medicines1,2. Irrational use of medicines has several severe consequences including adverse drug reactions, drug resistance, protracted illness and even death. Inappropriate use and over-use of medicines waste resources, resulting in increased out-of-pocket expenditure by patients1,2.
The Government of Karnataka in 2005 published essential medicines list (EML) and standard treatment guidelines (STG) for use in the primary health care facilities in the State3,4. Since the implementation of these guidelines there was no formal assessment of the prescription practices and availability of essential medicines in the State. Hence, a study was conducted to describe the medicine prescription practices of the medical officers, and medicine dispensing practices of the pharmacists in primary health centres (PHCs) of Shimoga district, Karnataka, following the WHO guidelines for investigation of drug use in health facilities5.
Twenty of the 65 PHCs in Shimoga district were randomly selected. From each PHC, 30 consecutive patients were contacted on each Monday during the study period (December 2011-April 2012). The prescriptions of these patients were reviewed to abstract the details of medicines prescribed using the standardized data collection form to calculate five prescription indicators, i.e. (i) average number of medicines per prescription, (ii) percentage of medicines prescribed by generic name, (iii) percentage of prescriptions with antibiotic, (iv) percentage of medicines prescribed as per the essential medicines list, and (v) percentage of prescriptions with injections.
For calculating the patient care indicators, ten consecutive patients exiting from dispensing room on each Monday during the study period were observed from each PHC to calculate the dispensing time, and were interviewed to know their knowledge about the dosage of medicines prescribed. From the prescriptions of these patients, the information about the number of medicines prescribed, number of medicines actually dispensed, and number of medicines adequately labelled with respect to their strength, dosage and frequency was abstracted.
To calculate the facility based indicators [availability of essential medicine list (EML) and STG, percentage availability of key indicator medicines], we physically verified the availability of 20 key essential medicines in the PHC and interviewed the medical officers and pharmacists to assess their awareness about EML and STG.
Averages and proportions were calculated for the medicine use indicators. To assess the degree of rational prescribing, the Index of Rational Drug Prescribing (IRDP) was calculated6. This index system has been validated for use in medical and health research6,7,8. The index of individual prescribing indicator was calculated by dividing the optimal level recommended for that indicator with the observed level in the survey. IRDP was calculated by adding up all the five indices described above. The study was approved by the institutional ethics committee of National Institute of Epidemiology (NIE), Chennai.
For describing the prescription indicators, information was abstracted from 600 prescriptions from the 20 sampled primary health centres. A total of 2059 medicines were prescribed in these prescriptions (average: 3.43, SD=1.53, range: 1-9). Most of the medicines prescribed were from EML (94%) and were prescribed by generic name (84%). About a quarter of the prescriptions were poly-pharmacy prescriptions (defined as prescriptions with 5 or more drugs). Antibiotics and injections were prescribed in 49 and 61 per cent of the prescriptions respectively (Table I).
Table I.
Indicators of rational drug use, Shimoga, Karnataka, India, 2012.
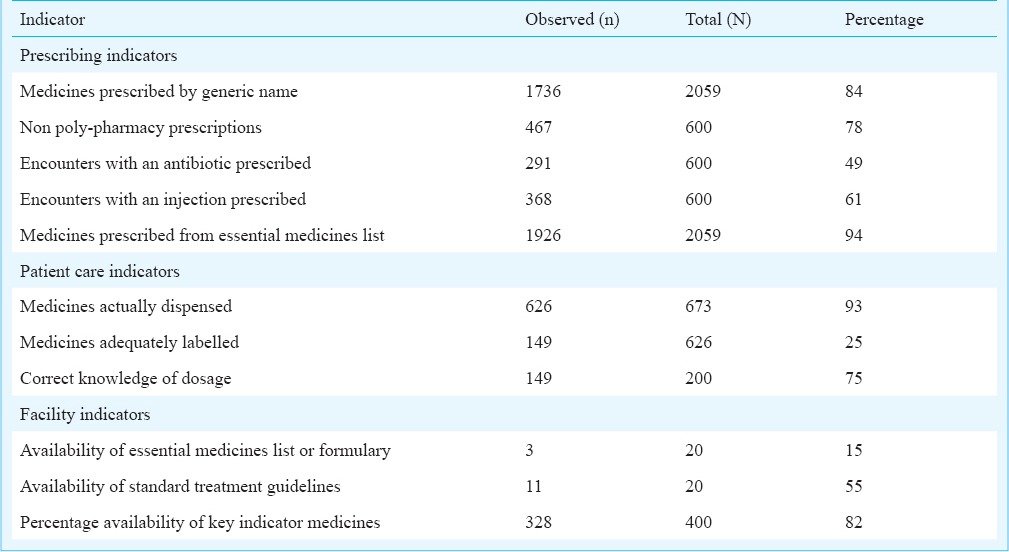
The 200 prescriptions surveyed for patient care indicators contained 673 medicines, of which 93 per cent medicines were dispensed in the PHC. Only 25 per cent of the medicines dispensed were adequately labelled with a mention of strength, dosage and duration. All prescriptions had a pictogram indicating the frequency of medicine use. Majority (75%, 149/200) of patients interviewed knew the correct dosage schedule for all the medicines prescribed. The average dispensing time was 86 ± 32.36 sec.
Overall, 82 per cent of the essential medicines were available in the PHCs. The EML and STG were available in three (15%) and 11 (55%) PHCs, respectively. Seventeen of the 20 (85%) medical officers and 15 of the 20 pharmacists (75%) interviewed were aware of essential medicines list. Twelve doctors (60%) were aware of standard treatment guidelines.
The overall IRDP of the Shimoga district was 3.42 compared to the optimal level of 5. The indices of rational antibiotic prescribing and injection use were low at 0.68 and 0.19, respectively (Table II). The findings of our study indicated that majority of the health facilities in Shimoga district had the key essential medicines. However, the index of rational drug prescribing was below the optimal level with high proportion of prescriptions containing injections and antibiotics. The findings of our study were comparable with the findings of studies conducted in 35 low-income countries which reported 45 per cent (range: 22-77%) of prescriptions had antibiotics2. It is a well established fact that overuse of antibiotics leads to bacterial drug resistance, which is an important public health problem in many developing countries9,10.
Table II.
Index of rational drug prescribing (IRDP) in primary health centres of Shimoga, Karnataka, India, 2012.

Overuse of injection was the most prominent manifestation of irrational prescribing in Shimoga with more than 60 per cent prescriptions containing at least one injection as compared to the optimal level of 10 per cent. High proportion of prescriptions with at least one injection was reported from several studies in India11,12.
Our study had certain limitations. First, the prescribers were aware about the study, which could have biased the prescribing indicators in a socially desirable direction. Second, determining the quality of diagnosis and evaluating the appropriateness of choice of medicine was beyond the scope of our study. Third, the study was conducted in only one district of Karnataka and hence it would not be possible to generalize the findings in other districts.
In conclusion, prescription and dispensing practices of health care providers in Shimoga district were found to be below the optimal level, especially with respect to prescribing injection and antibiotics. It is, therefore, necessary to train the health care providers in the district about the rational use of injections and antibiotics. Interventions such as interactional group discussion on safety of injection to doctors working in the primary health centres have shown to reduce injection prescribing13. It is also necessary to ensure that the EML and STG for antibiotic use are made available in every primary health centre. Shimoga is one of the better performing districts in the State with respect to health indicators14. The prescribing indicators observed in the district are, therefore, likely to reflect the best case scenario in the State and are likely to be better compared with other districts.
Footnotes
Conflicts of Interest: None.
References
- 1.World Health Organization (WHO). Promoting rational use of medicines: core components. WHO policy perspectives on medicines. 2002. [accessed on September 17, 2013]. Available from: http://apps.who.int/medicinedocs/pdf/h3011e/h3011e.pdf .
- 2.Holloway K, van Dijk L. 3rd ed. Geneva: WHO; 2011. [accessed on September 17, 2013]. The world medicines situation 2011-Rational use of medicines. Available from: http://apps.who.int/medicinedocs/documents/s18064en/s18064en.pdf . [Google Scholar]
- 3.1st ed. Bangalore: Karnataka State Drugs Logistic and Warehousing Society, Government of Karnataka; 2005. Essential drugs list. [Google Scholar]
- 4.Bangalore: Department of Health and Family Welfare, Government of Karnataka; 2005. Manual of standard treatment guidelines. [Google Scholar]
- 5.Geneva: WHO; 1993. [accessed on September 17, 2013]. World Health Organization (WHO). How to investigate drug use in health facilities. Selected drug use indicators. Available from: http://apps.who.int/medicinedocs/en/d/Js2289e/ [Google Scholar]
- 6.Dong L, Yan H, Wang D. Drug prescribing indicators in village health clinics across 10 provinces of Western China. Fam Pract. 2011;28:63–7. doi: 10.1093/fampra/cmq077. [DOI] [PubMed] [Google Scholar]
- 7.El Mahalli AA. WHO/INRUD drug prescribing indicators at primary health care centres in Eastern province, Saudi Arabia. Eastern Mediterr Health J. 2012;18:1091–6. doi: 10.26719/2012.18.11.1091. [DOI] [PubMed] [Google Scholar]
- 8.Akl OA, El Mahalli AA, Elkahky AA, Salem AM. WHO/INRUD drug use indicators at primary healthcare centers in Alexandria, Egypt. J Taibah Uni Med Sci. 2014;9:54–64. [Google Scholar]
- 9.Magee JT, Pritchard EL, Fitzgerald KA, Dunstan FD, Howard AJ. Antibiotic prescribing and antibiotic resistance in community practice: retrospective study, 1996-8. BMJ. 1999;319:1239–40. doi: 10.1136/bmj.319.7219.1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kang CI, Song JH. Antimicrobial resistance in Asia: current epidemiology and clinical implications. Infect Chemother. 2013;45:22–31. doi: 10.3947/ic.2013.45.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.INCLEN Program Evaluation Network (IPEN) study group. Injection practices in India. WHO South-East Asia J Public Health. 2012;1:189–200. doi: 10.4103/2224-3151.206931. [DOI] [PubMed] [Google Scholar]
- 12.Rajasekaran M, Sivagnanam G, Thirumalaikolundusubramainan P, Namasivayam K, Ravindranath C. Injection practices in southern part of India. Public Health. 2003;117:208–13. doi: 10.1016/S0033-3506(03)00065-9. [DOI] [PubMed] [Google Scholar]
- 13.Bhunia R, Hutin Y, Ramkrishnan R, Ghosh PK, Dey S, Murhekar M. Reducing use of injections through interactional group discussions: a randomized controlled trial. Indian Pediatr. 2010;47:409–14. doi: 10.1007/s13312-010-0076-4. [DOI] [PubMed] [Google Scholar]
- 14.Bangalore: ISEC; 2012. Institute for Social and Economic Change (ISEC). District level NRHM funds flow and expenditure: sub-national evidence from the State of Karnataka, Working Paper 278. [Google Scholar]


