Abstract
Ultrasound imaging of the skin is becoming more and more popular. Skin ultrasound examinations are used both in order to assess healthy skin and to evaluate pathological lesions. They are mainly performed in dermatology as well as in broadly understood aesthetic medicine and cosmetology. At present, skin imaging is enabled by high-frequency equipment and high-quality conventional devices. The introduction of high-frequency electronic transducers which are supported by conventional scanners may be a turning point in skin ultrasound equipment. Irrespective of the ultrasound scanner, three layers may be distinguished in the image of the healthy skin: epidermal echo, dermis and subcutaneous tissue. High-frequency equipment allows for detailed imaging of the epidermal echo, dermis and upper part of the subcutaneous tissue. It is also possible to visualize the skin appendages (hair with follicles and nails) as well as slight vessels that run in the dermis and upper subcutaneous tissue. Contrary to high-frequency equipment, conventional scanners do not allow for a detailed assessment of the epidermal and dermal echoes. Instead, they enable the visualization of the entire subcutaneous tissue. The following parameters are used for the assessment of skin ultrasound images: thickness of individual skin layers, caliber of blood vessels, echogenicity of the dermis or its individual layers, echogenicity of the subcutaneous tissue as well as the presence or absence of flow in slight venous vessels. Currently, the studies on the usage of sonoelastography for skin assessment are in progress. Considering the dynamic development of skin imaging equipment and its diagnostic possibilities, one might suspect that high-frequency examinations will become more common and will be fundamental for the evaluation of both healthy and pathologically altered skin. This paper is an introduction to a series of articles on the clinical application of high-frequency ultrasound. The next articles will be published in the subsequent issues.
Keywords: dermatology, aesthetic medicine, skin, sonography, skin ultrasound, high-frequency ultrasound
Abstract
Ultrasonograficzne obrazowanie skóry staje się coraz bardziej popularne. Badania ultrasonograficzne skóry znajdują zastosowanie zarówno w ocenie skóry zdrowej, jak i zmienionej chorobowo i są wykorzystywane przede wszystkim na gruncie dermatologii oraz szeroko rozumianej medycyny estetycznej i kosmetologii. Obecnie obrazowanie skóry możliwe jest przy wykorzystaniu aparatów wysokich częstotliwości oraz wysokiej klasy aparatów klasycznych. Przełomem w aparaturze do ultrasonograficznego badania skóry może być wprowadzenie do użycia wysokoczęstotliwościowych głowic elektronicznych, które współpracują z klasycznymi aparatami. Na obrazie skóry zdrowej bez względu na typ zastosowanego ultrasonografu wyróżniamy trzy warstwy: echo naskórka, skórę właściwą i tkankę podskórną. Aparaty wysokich częstotliwości umożliwiają szczegółowe obrazowanie echa naskórka, skóry właściwej i górnej części tkanki podskórnej. Możliwe jest również obrazowanie przydatków skóry (włosy wraz z mieszkami włosowymi, paznokcie) oraz drobnych naczyń krwionośnych biegnących w skórze właściwej i górnej części tkanki podskórnej. W ultrasonografach klasycznych, w porównaniu z aparatami wysokich częstotliwości, nie ma możliwości szczegółowej oceny echa naskórka i skóry właściwej. W zamian istnieje możliwość zobrazowania całej tkanki podskórnej. Do oceny ultrasonograficznych obrazów skóry wykorzystuje się następujące parametry: pomiary grubości poszczególnych warstw skóry, pomiar średnicy naczyń krwionośnych, pomiar echogeniczności skóry właściwej lub jej poszczególnych warstw, pomiar echogeniczności tkanki podskórnej, brak lub obecność przepływu w drobnych naczyniach żylnych. Aktualnie trwają prace nad wykorzystaniem do oceny skóry sonoelastografii. Biorąc pod uwagę dynamiczny rozwój aparatów do obrazowania skóry i ich możliwości diagnostyczne, można przypuszczać, że badania wysokich częstotliwości upowszechnią się i będą podstawą w ocenie skóry zarówno zdrowej, jak i zmienionej chorobowo. Praca stanowi wstęp do cyklu artykułów o klinicznych zastosowaniach ultrasonografii wysokich częstotliwości, które będą omawiane na łamach kolejnych numerów.
The technological advancement, which took place in the last thirty years, has contributed to the development of sonography. With the creation of various new scanners and transducers, the imaging of the largest human organ, i.e. the skin, has become possible(1). The first works on skin imaging began over 40 years ago. The pioneers, who as the first ones published a paper concerning the assessment of the skin by means of 15 MHz transducer, were Alexander and Miller(2). Alexander and Miller performed A-mode examinations thanks to which they managed to measure the thickness of the skin. Although high-frequency A-mode ultrasound is still used in ophthalmology, its application in skin imaging is limited since it allows for obtaining information concerning only one parameter, i.e. for measuring the thickness of a given structure. In the following years, more and more reports concerning skin imaging appeared. Nevertheless, the real breakthrough was brought about by the invention of high-frequency ultrasound transducers (above 20 MHz)(3–5). Since then, a dynamic development of skin examinations has been observed. The examinations connected with skin imaging focus on two aspects. The first of them is related to the diagnosis of healthy skin and to monitoring the changes occurring within it that result from various factors(6–8). In the case of the healthy skin, based on its thickness and echogenicity, the researchers attempt to describe the changes caused by natural ageing processes and photoageing connected with excessive exposition to ultraviolet radiation. They also try to determine sex-related differences(6, 7). As Waller and Maibach(6) indicate, there is no agreement among researchers concerning the changes of the skin's thickness occurring with age. Several papers demonstrated that the dermis is the thickest in young persons and subsequently, it becomes thinner with age. Other authors claim that it is not the age, but external factors, such as UV radiation, that play a crucial role in the change of the thickness of the dermis. The changes in the echogenicity of the skin are also interpreted in various ways. Nonetheless, most of the researchers confirm that in the ageing skin, echogenicity undergoes changes and a subepidermal anechoic band appears, so-called SLEB (subepidermal low-echogenic band). Such divergent results obtained by different researchers may be disturbing, but one should remember that their studies were conducted with the use of different scanners, there were few such trials and what is more, the examinations were performed on the skin in various localizations. In such a situation, large randomized studies would be desirable. What is more, attempts are also made to assess the activity of skin irritating factors by means of high-frequency ultrasound(8). Seidenari demonstrated that ultrasound allowed for monitoring the inflammation caused by the application of acids on the healthy skin. Apart from the assessment of the healthy skin, ultrasound is also used in dermatology. Above all, it is used for imaging of the pathologically altered skin and for monitoring the course of treatment(9–11). One of the first diseases assessed by sonography is scleroderma(9) – both ultrasound diagnosis and monitoring the course of treatment are possible. With the appearance of high-frequency equipment, in the field of dermatology, numerous studies were started whose aim is to visualize and differentiate between focal lesions(10). Currently, sonography allows for imaging of the majority of neoplastic lesions of the skin, both benign and malignant, measuring such changes and evaluating them in relation to adjacent tissues. Unfortunately, it is still not possible to differentiate between such lesions based on ultrasound presentation. The studies concerning the foregoing issues are being conducted continuously, the proof of which is a recently published article(11) whose author indicates characteristic features of basal-cell carcinoma based on ultrasound images.
Skin ultrasound examinations are becoming more and more popular which is proven by the growing number of academic publications as well as by the number of scanners for skin imaging available on the market. Furthermore, ultrasound scanners for skin examinations more and more frequently constitute an integral element of the equipment used in aesthetic medicine for lifting or silhouette modeling. For instance, Ulthera™ (Ulthera, Inc., Arizona, USA) and Doublo Hironic (Hironic Co., Ltd., Korea) are applied for non-surgical facelift procedures where the obtained skin image constitutes the basis for the selection of surgical parameters and monitoring the course of the procedure. Another example of equipment in the field of aesthetic medicine that uses ultrasound examinations is Storz Medical, a device for silhouette modeling. In this case, sonography is used to assess the skin prior to the commencement of the therapy and to monitor its course.
Apparatus
Skin ultrasound examinations may be performed by means of high-frequency scanners and modern, high-class conventional machines.
High-frequency apparatuses are equipped with singleelement mechanical transducers with the frequency of 20–100 MHz(10, 12). At present, there are a few machines available on the market that are dedicated to skin examinations. DermaScan by Cortex Technology (Denmark) is one of the best known scanners with the transducers with the frequency ranging from 10 to 50 MHz. This apparatus also supports the option of saving three dimensional (3D) images. Another popular ultrasound machine for skin examinations is Episcan (fig. 1) by Longport International (Great Britain, USA) which is available with the transducers of 20–50 MHz. Since 1986, DUB® scanners by a German company taberna pro medicum GmbH are also on the market. In the beginning, such machines were equipped with the transducers of 20 MHz. Currently, the producers offer a wide range of transducers, reaching even 75 MHz. This year, a high-frequency ultrasound scanner DermaView by Dramiński company with the transducer of 48 MHz (fig. 2) made its debut on the Polish market. What is more, the Institute of Fundamental Technological Research of the Polish Academy of Sciences led by Professor Andrzej Nowicki has been working on their high-frequency apparatus for over 20 years. This team has created µScan machine which is continuously upgraded and perfected (fig. 3). Currently, µScan is used with the transducer of 35 MHz. Unfortunately, such equipment is not yet available for sale. All the abovementioned scanners are equipped with specialist software enabling the performance of basic measurements as well as saving and archiving obtained images. Some of the high-frequency transducers allow for color imaging (in green, red or blue depending on the settings of an apparatus).
Fig. 1.
High-frequency ultrasound scanner Episcan (Longport Int., USA) with a mechanical transducer of 50 MHz
Fig. 2.
High-frequency ultrasound scanner DermaView (Dramiński, Poland) with a mechanical transducer of 48 MHz
Fig. 3.
High-frequency ultrasound scanner μScan with a mechanical transducer of 35 MHz created in the Institute of Fundamental Technological Research of the Polish Academy of Sciences: A. a model from a few years ago; B. current appearance
Nevertheless, to perform skin ultrasound examinations, conventional scanners with broadband linear-array transducers may also be used. Thanks to outstanding technological progress and the introduction of a range of options that improve imaging, such as harmonic imaging, skin examination is rendered possible even with the use of broadband linear-array transducers with the frequency of 12–18 MHz. Moreover, linear transducers with the frequency of 20 MHz are more and more often available on the market. A new option, which might prove useful in skin imaging, is elastography.
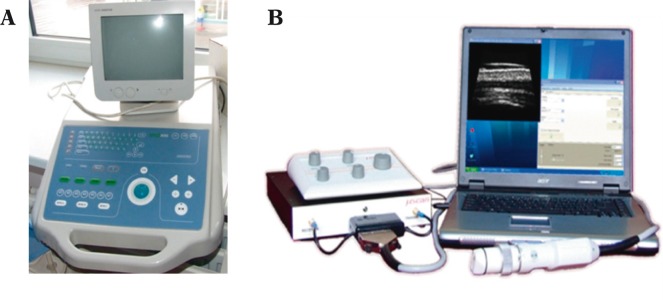
Last year, a Canadian company, Ultrasonix, created and introduced to the market an electronic, multi-element linear transducer with the frequency of 40 MHz (fig. 4) which is supported by conventional ultrasound machines. This is an innovation and, probably, a breakthrough in high-frequency ultrasound. This transducer also allows for the performance of vascular examinations with power Doppler, pulse Doppler or color Doppler options, which is highly useful in the assessment of vessels running in the dermis and subcutaneous tissue.
Fig. 4.
Conventional ultrasound scanner Sonix (Ultrasonix, Canada) with an electronic, multi-element linear transducer with the frequency of 40 MHz
Ultrasound image of the skin
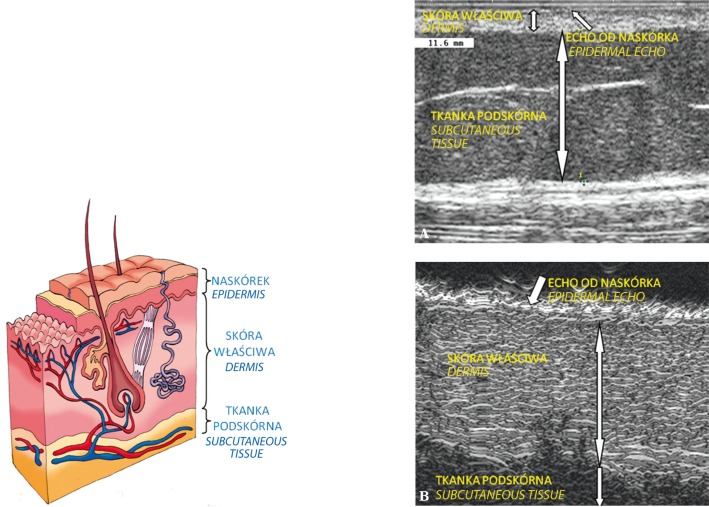
In the ultrasound image of the healthy skin, three basic layers may be distinguished: epidermal echo, dermis and subcutaneous tissue(12, 13), which correspond to the anatomical structure of the skin(14) (fig. 5). Depending on the ultrasound scanner and the frequency of the transducer, images of various resolutions may be obtained. The higher the resolution, the lower the depth of ultrasound beam penetration into the skin. This allows for the visualization of the greater number of details. Therefore, for a thorough assessment of the skin, high-frequency equipment is irreplaceable (fig. 5).
Fig. 5.
Ultrasound image of the skin with visible three layers: epidermal echo, dermis and subcutaneous tissue: A. image obtained by means of a classical scanner Philips HD11 XE with a linear-array transducer; B. scan obtained by means of a high-frequency ultrasound machine Episcan with a mechanical transducer of 50 MHz
The first layer visible from the head of the transducer is a hyperechoic line that corresponds to the epidermis. In 1992, Altmeyer(13) observed that this line is not the epidermis itself, but it is created by the reflections between the ultrasound gel and the surface of the skin as well as the reflections from the epidermis and air bubbles located between the callused epidermal cells. He proposed to call this line an epidermal echo. Currently, when it is possible to visualize the epidermis by means of transducers with the frequency of 50 MHz and more, this idea appears to be correct and the term ‘epidermal echo’ is still in use.
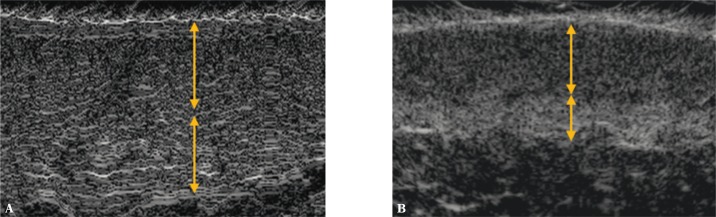
Beneath the epidermis, lies the dermis. It may be anatomically divided into the papillary dermis (uppermost part of the dermis lying beneath the epidermis) and reticular dermis (a layer located under the papillary dermis)(14). The papillary dermis constitutes circa 20% of the dermis(14) and contains blood vessels and irregularly arranged thin collages and elastin fibers(15). On the other hand, in the reticular dermis, which constitutes approximately 80% of the dermis(14), the collagen, elastin and reticular fibers are arranged regularly. In terms of echogenicity, the dermis is a heterogeneous layer with hyperechoic reflections of the collagen fibers and hypoechoic ones originating from the extracellular matrix that lies between the collagen fibers. Furthermore, by means of the ultrasound machines supporting the transducers of 30 MHz and more, two layers may be distinguished in the dermis that differ in terms of their echogenicity (fig. 6). The upper layer is usually thinner and presents decreased echogenicity in comparison to the lower one. This diversification of the dermal image results from the anatomical structure of the skin. As was shown above, the papillary dermis includes a lower number of the collagen fibers and they are much thinner. Therefore, they reflect ultrasounds in a weaker way. This results in lower echogenicity as compared to the echoes of the collagen fibers situated in the lower layer – they are thicker and thus, produce stronger echoes. Unfortunately, the division of the skin into the upper and lower layers as seen in the ultrasound image, may not be strictly understood as the division into the papillary and reticular dermis.
Fig. 6.
Ultrasound image of the dermis with its visible division into the upper and lower layers: A. image obtained by means of a highfrequency scanner Episcan with a mechanical transducer of 50 MHz; B. scan obtained by means of a high-frequency ultrasound machine DermaView with a mechanical transducer of 48 MHz
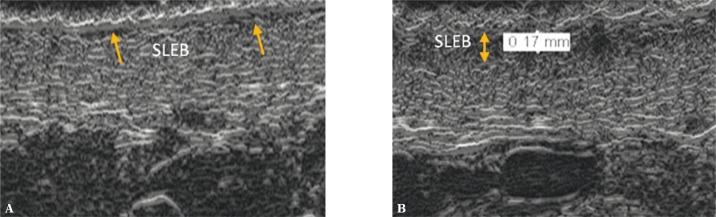
In some ultrasound images, a thin anechoic band may be observed between the epidermal echo and the dermis (fig. 7), so-called SLEB (subepidermal low-echogenic band) or SENEB (subepidermal non-echogenic band). SLEB appears in the aged skin or skin subjected to excessive exposition to ultraviolet radiation(16–19). Moreover, the increase in the thickness of SLEB is related to water retention in the papillary dermis(20).
Fig. 7.
Imaging of the anechoic band lying beneath the epidermis (SLEB) by means of a high-frequency ultrasound scanner Episcan with a mechanical transducer of 50 MHz: A. SLEB of slight thickness on the cheek; B. well visible SLEB on the dorsal side of the hand
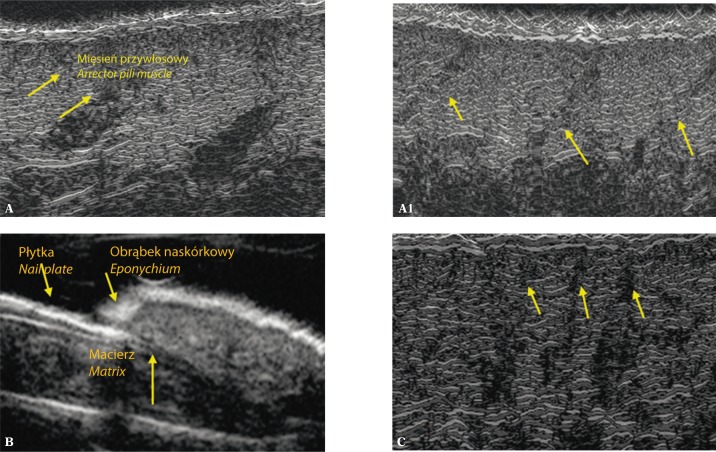
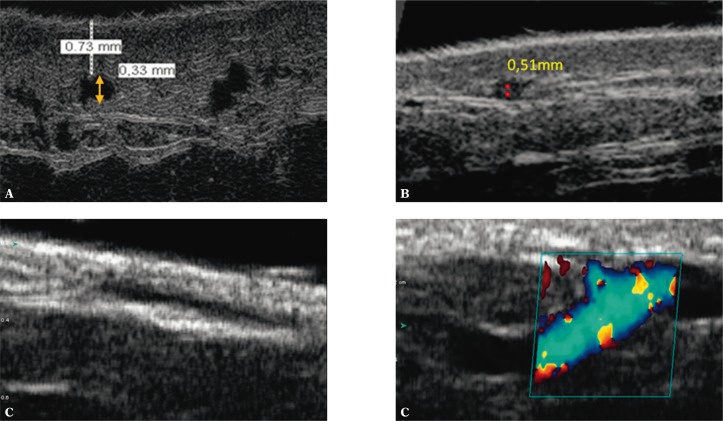
In the region of the dermis, one may also visualize skin appendages such as nails or hair follicles and openings of the sweat glands (fig. 8). Depending on the frequency of the transducer and abilities of the examiner, it is also possible to visualize the hair fiber located in the follicle and the arrector pili muscle. Moreover, it is possible to visualize slight blood vessels, including telangiectasias, whose diameters are lower than 1 mm (fig. 9).
Fig. 8.
Ultrasound imaging of the skin appendages: A. hair follicles with the arrector pili muscle; A1. numerous hair follicles on the chin of a male patient; B. nail; C. openings of the sweat glands
Fig. 9.
Ultrasound imaging of the vessels in the skin: A. Episcan apparatus with a transducer of 50 MHz; B. DermaView apparatus with a transducer of 48 MHz; C. Sonix apparatus with the linear transducer of 40 MHz and color Doppler option
The third layer seen in ultrasound images is the subcutaneous tissue. The entire subcutaneous tissue may be assessed in conventional ultrasound scans but high-frequency machines enable the assessment of merely its upper part which is seen as a hypoechoic layer with linear hyperechoic reflections. Due to the fact that the measurement of the thickness of the subcutaneous tissue is particularly significant for aesthetic medicine and cosmetology, there are ongoing works whose aim is to enable its visualization by a single machine. In this case, the solution introduced by Dramiński company, namely, the possibility to decrease the frequency of the transducer, is interesting since it increases the depth of the penetration which enables to visualize the subcutaneous tissue.
Examination technique and assessed parameters
Most of the skin ultrasound examinations do not require any particular preparations. Prior to the examination, the condition of the skin to be examined should be assessed visually or by palpation. The patient may assume any position depending on the examined region. The technique of the examination depends on the used ultrasound equipment. Usually, ultrasound gel is placed on the examined region and subsequently, the examination is performed by moving the transducer slowly along the tested region. The highfrequency DUB® apparatus is an exception. In this case, ultrasound gel is not used and the ultrasound transducer is tightly applied to the tested region and subsequently, filled with water. On the one hand, thanks to this solution, the reflections from the foil used in the transducers of other ultrasound machines may be avoided. On the other hand, it is inconvenient and renders the movement of the transducer impossible. If sonoelastography option is used during skin ultrasound examination, the technique depends on the type of elastography provided by the apparatus(21).
In ultrasound assessment of the skin, various parameters are taken into consideration such as: thickness of the epidermal echo, dermis and subcutaneous tissue, the surface area of particular layers, thickness of SLEB, calibers of the blood vessels as well as presence or absence of flow in the vessels. A particularly useful parameter is the assessment of the echogenicity of individual layers of the skin or their fragments. Echogenicity may be determined with the use of a number of pixels counted in a given area of interest. Depending on the purpose of the examination, echogenicity may also be analyzed based on the indicator which determines the ratio of pixels from a given range of brightness to the total number of pixels in a given area of interest. Such an indicator was introduced by Gniadecka and Quistorff(22) who in their study on determining the level of skin hydration by sonography calculated the ratio of the darkest pixels (ranging from 0–30 in the grey-scale of 256 shades) to the total number of pixels in a given area of interest. The indicator described by Gniadecka was used in the research conducted by one of the authors of this paper(23).
Conclusion
Skin ultrasound examinations are becoming more and more popular. They are performed in order to evaluate healthy and pathologically altered skin as well as to monitor the changes taking place in the skin. Such a popularization is conditioned by the technological progress which allows for the production of perfected ultrasound scanners that are cheaper and easy to use. The advantages of sonography itself are also significant, i.e. its non-invasive character, possibility to repeat examinations and mobility. Unfortunately, at present, the lack of uniform examination standards and assessment parameters is noticeable. This frequently renders it impossible for different researchers to compare their results. For the sake of the development of skin ultrasound examinations, it is vital to continue studies in this regard, to conduct large randomized trials as well as to standardize the methodology and propose examination standards.
This paper is an introduction to a series of articles devoted to the clinical application of skin sonography. Its use in aesthetic medicine and phlebology will be discussed in the subsequent issues.
Conflict of interest
Authors do not report any financial or personal links with other persons or organizations, which might affect negatively the content of this publication and/or claim authorship rights to this publication.
References
- 1.Szymańska E, Maj M, Majsterek M, Litniewski J, Nowicki A, Rudnicka L. Zastosowanie ultrasonografii wysokiej częstotliwości w diagnostyce dermatologicznej – obraz ultrasonograficzny wybranych zmian skórnych. Pol Merkuriusz Lek. 2011;31:37–40. [PubMed] [Google Scholar]
- 2.Alexander H, Miller DL. Determining skin thickness with pulsed ultra sound. J Invest Dermatol. 1979;72:17–19. doi: 10.1111/1523-1747.ep12530104. [DOI] [PubMed] [Google Scholar]
- 3.Tikjøb G, Kassis V, Søndergaard J. Ultrasonic B-scanning of the human skin. An introduction of a new ultrasonic skin-scanner. Acta Derm Venereol. 1984;64:67–70. [PubMed] [Google Scholar]
- 4.Dines KA, Sheets PW, Brink JA, Hanke CW, Condra KA, Clendenon JL, et al. High frequency ultrasonic imaging of skin: experimental results. Ultrason Imaging. 1984;6:408–434. doi: 10.1177/016173468400600403. [DOI] [PubMed] [Google Scholar]
- 5.Yano T, Fukukita H, Ueno S, Fukumoto A. 40 MHz ultrasound diagnostic system for dermatologic examination. IEEE Ultrasonics Symposium Proceeding. 1987:875–878. [Google Scholar]
- 6.Waller JM, Maibach HI. Age and skin structure and function, a quantitative approach (I): blood flow, pH, thickness, and ultrasound echogenicity. Skin Res Technol. 2005;11:221–235. doi: 10.1111/j.0909-725X.2005.00151.x. [DOI] [PubMed] [Google Scholar]
- 7.Seidenari S, Pagnoni A, Di Nardo A, Giannetti A. Echographic evaluation with image analysis of normal skin: variations according to age and sex. Skin Pharmacol. 1994;7:201–209. doi: 10.1159/000211295. [DOI] [PubMed] [Google Scholar]
- 8.Seidenari S. Echographic evaluation with image analysis of irritant reactions induced by nonanoic acid and hydrochloric acid. Contact Dermatitis. 1994;31:146–150. doi: 10.1111/j.1600-0536.1994.tb01953.x. [DOI] [PubMed] [Google Scholar]
- 9.Szymanska E, Nowicki A, Mlosek K, Litniewski J, Lewandowski M, Secomski W, et al. Skin imaging with high frequency ultrasound – preliminary results. Eur J Ultrasound. 2000;12:9–16. doi: 10.1016/s0929-8266(00)00097-5. [DOI] [PubMed] [Google Scholar]
- 10.Schmid-Wendtner MH, Dill-Müller D. Ultrasound technology in dermatology. Semin Cutan Med Surg. 2008;27:44–51. doi: 10.1016/j.sder.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 11.Wortsman X. Sonography of facial cutaneous basal cell carcinoma: a first-line imaging technique. J Ultrasound Med. 2013;32:567–572. doi: 10.7863/jum.2013.32.4.567. [DOI] [PubMed] [Google Scholar]
- 12.Nowicki A. Wstęp do ultrasonografii. Podstawy fizyczne i instrumentacja. Warszawa: MediPage; 2004. [Google Scholar]
- 13.Altmeyer P, El-Gammal S, Hoffmann K, editors. Ultrasound in Dermatology. Heidelberg: Springer-Verlag; 1992. [Google Scholar]
- 14.Martini MC. Anatomia i fizjologia skóry. In: Martini MC, editor. Kosmetologia i farmakologia skóry. Warszawa: Wydawnictwo Lekarskie PZWL; 2007. pp. 37–59. [Google Scholar]
- 15.Nowicka D. Funkcje i budowa skóry oraz jej przydatków. In: Nowicka D, editor. Dermatologia. Podręcznik dla studentów kosmetologii. Wrocław: Górnicki Wydawnictwo Medyczne; 2010. pp. 1–8. [Google Scholar]
- 16.de Rigal J, Escoffier C, Querleux B, Faivre B, Agache P, Lévêque JL. Assessment of aging of the human skin by in vivo ultrasonic imaging. J Invest Dermatol. 1989;93:621–625. doi: 10.1111/1523-1747.ep12319741. [DOI] [PubMed] [Google Scholar]
- 17.Serup J. High-frequency ultrasound examination of aged skin: intrinsic, actinic, and gravitational aging, including new concepts of stasis dermatitis and leg ulcer. In: Lévêque JL, Agache PG, editors. Aging Skin: Properties and Functional Changes. New York: Marcel Dekker; 1993. pp. 69–85. [Google Scholar]
- 18.Lévêque JL. Non invasive measurements on photodamaged skin. In: Gilchrest BA, editor. Photodamage. New York: Blackwell Science, Inc.; [Google Scholar]
- 19.Gniadecka M, Jemec GBE. Quantitative evaluation of chronological ageing and photoageing in vivo: studies on skin echogenicity and thickness. Br J Dermatol. 1998;139:815–821. doi: 10.1046/j.1365-2133.1998.02506.x. [DOI] [PubMed] [Google Scholar]
- 20.Richard S, Querleux B, Bittoun J, Jolivet O, Idy-Peretti I, de Lacharriere O, et al. Characterization of the skin in vivo by high resolution magnetic resonance imaging: water behavior and age-related effects. J Invest Dermatol. 1993;100:705–709. doi: 10.1111/1523-1747.ep12472356. [DOI] [PubMed] [Google Scholar]
- 21.Mlosek RK. Badanie usg skóry. In: Jakubowski W, editor. Standardy badań ultrasonograficznych Polskiego Towarzystwa Ultrasonograficznego. Wyd. 4. Warszawa – Zamość: Praktyczna Ultrasonografia, Roztoczańska Szkoła Ultrasonografii; 2011. [Google Scholar]
- 22.Gniadecka M, Quistorff B. Assessment of dermal water by high-frequency ultrasound: comparative studies with nuclear magnetic resonance. Br J Dermatol. 1996;135:218–224. [PubMed] [Google Scholar]
- 23.Mlosek RK. Obrazowanie skóry i tkanki podskórnej za pomocą ultrasonografii klasycznej oraz ultrasonografii wysokich częstotliwości i jego przydatność w kosmetologii i medycynie estetycznej. Warszawa: Warszawski Uniwersytet Medyczny; 2012. [Google Scholar]