Abstract
Gamma (γ)-band oscillations play a key role in perception, associative learning, and conscious awareness and have been shown to be disrupted by cannabinoids in animal studies. The goal of this study was to determine whether cannabinoids disrupt γ-oscillations in humans and whether these effects relate to their psychosis-relevant behavioral effects. The acute, dose-related effects of Δ-9-tetrahydrocannabinol (Δ9-THC) on the auditory steady-state response (ASSR) were studied in humans (n=20) who completed 3 test days during which they received intravenous Δ9-THC (placebo, 0.015, and 0.03 mg/kg) in a double-blind, randomized, crossover, and counterbalanced design. Electroencephalography (EEG) was recorded while subjects listened to auditory click trains presented at 20, 30, and 40 Hz. Psychosis-relevant effects were measured with the Positive and Negative Syndrome scale (PANSS). Δ9-THC (0.03 mg/kg) reduced intertrial coherence (ITC) in the 40 Hz condition compared with 0.015 mg/kg and placebo. No significant effects were detected for 30 and 20 Hz stimulation. Furthermore, there was a negative correlation between 40 Hz ITC and PANSS subscales and total scores under the influence of Δ9-THC. Δ9-THC (0.03 mg/kg) reduced evoked power during 40 Hz stimulation at a trend level. Recent users of cannabis showed blunted Δ9-THC effects on ITC and evoked power. We show for the first time in humans that cannabinoids disrupt γ-band neural oscillations. Furthermore, there is a relationship between disruption of γ-band neural oscillations and psychosis-relevant phenomena induced by cannabinoids. These findings add to a growing literature suggesting some overlap between the acute effects of cannabinoids and the behavioral and psychophysiological alterations observed in psychotic disorders.
INTRODUCTION
With the legalization of ‘medical’ marijuana (cannabis) (Kleber and DuPont, 2012; Procon.org, 2014) and recreational cannabis use in some states of the United States (Wilkinson and D'Souza, 2014), the high rates (ONDCP, 2008; SAMHSA, 2011) and earlier onset of cannabis use (Johnston et al, 2012), the increasing potency of cannabis (Mehmedic et al, 2010), the recreational use of highly potent synthetic cannabinoids (eg, Spice and K-2) (Johnson et al, 2011; Vardakou et al, 2010), and the high rates of emergency department visits related to cannabis (SAMHSA, 2012), there is a need to understand the basic mechanisms underlying the behavioral effects of cannabinoids such as Δ-9-tetrahydrocanabinol (Δ9-THC), the primary psychoactive constituent in cannabis.
Δ9-THC, via activation of brain cannabinoid 1 receptors (CB1Rs), induces a range of acute alterations in perceptual, emotional, and cognitive functions that are relevant to psychotic states and psychotic disorders such as schizophrenia (reviewed in Radhakrishnan et al, 2014). Neural oscillations in the gamma (γ)-band (30–80 Hz) are thought to play a key role in the operation of these functions by participating in sensory registration and integration, associative learning, and conscious awareness among other processes (Uhlhaas et al, 2008). Therefore, it is expected that alterations in these processes will be associated with abnormalities in γ-band oscillations. Consistent with this view, a number of studies in schizophrenia patients have confirmed the existence of an association between functional and γ-band abnormalities as measured by electroencephalography (EEG) (see Uhlhaas et al, 2008 for review). This raises the intriguing possibility that some of the acute psychosis-relevant functional abnormalities induced by Δ9-THC may be associated with γ-band alterations (Skosnik et al, 2006).
Consistent with this possibility, both in vitro and in vivo studies in animals have shown that CB1R agonists modulate γ-oscillations in the cerebral cortex and hippocampus (Hajos et al, 2000, 2008; Morgan et al, 2008; Robbe et al, 2006). For example, systemic administration of the CB1R agonist CP-55940 has been shown to decrease the amplitude of γ-band oscillations in mice as measured via neocortical electrocorticograms (Sales-Carbonell et al, 2013). Similar findings have been observed via local field potential (LFP) recordings in rats (Hajos et al, 2008).
However, although γ-band abnormalities have been reported in schizophrenia, cannabinoids have been shown to acutely induce psychosis-relevant phenomena in healthy humans, and cannabinoids have been shown to disrupt γ-band oscillations in animals, we are unaware of any studies in humans examining the acute effects of CB1R agonists on either γ-band oscillations or the relationship between γ-band oscillations and the acute psychosis-relevant phenomena induced by CB1R agonists.
In humans, macroscopic synchronized neural oscillations can be evaluated noninvasively with the EEG by measuring the brain’s auditory steady-state response (ASSR) to sensory stimulation, that is, the entrainment of EEG activity to regular auditory stimuli (eg, auditory click trains) of varying frequencies. Neural circuits act as oscillators that tune their activity to the frequency and phase of the presented stimuli, providing an indicator of the brain’s ability to engage in transient states of synchronized oscillatory activity at the frequency used for stimulation. Furthermore, a number of studies have shown that the ASSR is sensitive to the abnormalities present in schizophrenia. For example, first-episode and chronic schizophrenia patients show attenuated γ-band (~40 Hz) responses in the ASSR paradigm (Krishnan et al, 2009; Kwon et al, 1999; Light et al, 2006; Spencer et al, 2008a) that is associated with some of the characteristic abnormalities of the disorder (eg, positive symptoms and working memory deficits) (Light et al, 2006; Spencer et al, 2008b). In view of this, we selected the ASSR paradigm to study the relationship between acute Δ9-THC-induced alterations in γ-band oscillations and psychosis-relevant effects.
This study was part of a larger project that aimed to assess the dose-related effects of Δ9-THC on several electrophysiological indices of information processing relevant to psychosis (eg, P300; D'Souza et al, 2012) and to determine the relationship between the electrophysiological and behavioral effects of Δ9-THC. In this study we examined the acute, dose-related effects of intravenous (i.v.) Δ9-THC on the ASSR in a number of frequency bands, and the relationship between these effects and the psychosis-relevant effects induced by Δ9-THC. We hypothesized that Δ9-THC would specifically reduce the γ-band (40 Hz) ASSR, and that γ-band ASSRs measures would be inversely correlated with the psychosis-relevant effects of Δ9-THC.
MATERIALS AND METHODS
This randomized, double-blind, placebo-controlled, counterbalanced, crossover study was conducted at the Neurobiological Studies Unit (VA Connecticut Healthcare System (VACHS), West Haven, CT). Subjects were recruited by advertisements and by word of mouth, and were paid for their participation. The study was approved by the institutional review boards of the VACHS and Yale University School of Medicine and was carried out in accordance with the Helsinki Declaration of 1975. Subjects were informed about the potential for adverse effects of Δ9-THC including psychosis, anxiety, panic, and abuse liability.
Subjects
After obtaining written informed consent, subjects (n=30; 18–35 years) underwent a Structured Clinical Interview for DSM-IV (SCID; First et al, 2002) and were carefully screened for any DSM Axis I lifetime psychiatric or substance use disorder (excluding tobacco and cannabis use) and family history of major Axis I disorder. Subjects were screened at a separate session within ∼4 weeks of the first test day. Cannabis-naive individuals were excluded to minimize any risk of promoting future cannabis use/abuse. Subjects with DSM-IV cannabis dependence based on the SCID were excluded because cannabis dependence has been associated with a bunted response to THC (tolerance). Subjects were categorized into those who had not used cannabis in the past 30 days (recent users) and those who had not (nonusers) for exploratory analyses to determine the effects of cannabis exposure on study outcomes. The history provided by subjects was confirmed by a telephone interview conducted with a spouse or family member identified by the subject. A general physical and neurological examination, electrocardiogram, and laboratory tests (serum electrolytes, liver function tests, complete blood count with differential, urine toxicology, and urine pregnancy in women) were also conducted. After screening, subjects were instructed to refrain from alcohol, caffeinated beverages, illicit drugs (other than cannabis), or prescription drugs not approved by the research team for 2 weeks before the study and throughout study participation. Cigarette smokers were permitted to participate only if their pattern of cigarette consumption would allow them to abstain for each test day (0800–1500 h) and their consumption did not exceed 10 cigarettes/day. Recent users of cannabis were instructed to abstain from smoking for at least 24 h before test day. Test days were rescheduled if subjects reported using cannabis within 24 h of the test day. Subjects who were not categorized as recent users of cannabis were reminded not to use cannabis for 2 weeks before testing and throughout study participation. For this group, abstinence was confirmed by urine drug testing on the morning of each test day.
Subjects completed 3 test days during which they received Δ9-THC (placebo (vehicle (ethanol)), 0.015 mg/kg, or 0.03 mg/kg) over 10 min by i.v. route in a randomized, counterbalanced order under double-blind conditions. Both staff and subjects received identical information without reference to any hypothesized group differences.
Drugs
The preparation, formulation, and storage of the Δ9-THC solutions are reported elsewhere (D'Souza et al, 2004). For the control placebo condition, an equivalent volume of ethanol (vehicle) was used that was previously shown to be undetectable in multiple postinjection blood samples (D'Souza et al, 2004). The i.v. route of administration was chosen to standardize the delivery of Δ9-THC as discussed previously (D'Souza et al, 2004).
General EEG Acquisition and Processing
Multichannel EEG was recorded from the scalp using a 22-lead electrode cap (Physiometrix, Billerica, MA) based on the International 10–20 System (see Supplementary Text 5). Electrode impedances were maintained <5 kohms. Recordings were made using a linked ear reference. The data were recorded using Neuroscan Synamps amplifiers (Neuroscan SynAmps, Compumedics Neuroscan, Charlotte, NC). Codes indicating stimulus onset and type were incorporated into the data stream for offline averaging and analysis using Neuroscan Acquire software for data acquisition and software for stimulus presentation (Presentation, Neurobehavioral Systems, Berkeley, CA). EEG was continuously monitored on a screen outside the recording chamber to detect drowsiness.
ASSR Paradigm
For assessment of ASSRs, subjects sat in an acoustically shielded booth in front of a computer monitor with eyes open, while passively listening to click trains presented through Etymotic insert ER-1 earphones (Etymotic Research, Elk Grove Village, IL). Stimuli consisted of standard, unattended (nontarget) auditory click trains from a three-stimulus oddball task as reported previously (D'Souza et al, 2012). The auditory click trains were presented at three different frequencies (20, 30, and 40 Hz; 80 dB SPL). Each block contained 150 trials of a single frequency presented for 500 ms each (ISI 750 ms). Each trial lasted 1250 ms, and each block lasted 4 min. Across subjects, the order of blocks was counterbalanced and the order of conditions was randomized.
EEG Signal Analysis
A detailed account of EEG methods is provided in the Supplementary Text 1. Continuous EEG data were band-pass filtered (0.5–100 Hz), line noise was removed using a multi-tapering technique (Partha and Hemant, 2007), muscle artifacts were removed using a blind source separation algorithm (De Clercq et al, 2006), and eye movement and blink artifacts were removed with an adaptive filter algorithm (Puthusserypady and Ratnarajah, 2005). Data were segmented in 1200 ms epochs time-locked to stimulus onset, with a 300-ms prestimulus baseline. A ±95 μV voltage criterion was used to reject bad epochs. EEG data from three midline electrodes (Fz, Cz, and Pz) were used for ASSR analyses, given that the ASSR is typically maximal at the midline electrodes (Skosnik et al, 2012). All analyses were done in Matlab (MathWorks, Natick, MA) using either custom-made scripts (for inter-trial coherence (ITC) and evoked power) or the EEGLAB toolbox’ scripts and plugins (for signal preprocessing) (Delorme and Makeig, 2004; Gómez-Herrero et al, 2006).
ITC reflects the consistency across trials of the phases of the brain’s electrophysiological response to equivalent stimuli/events (Tallon-Baudry et al, 1996). ITC values range from 0 to 1, being maximal at a given time point (relative to the onset of the stimulation/event) when the phases of the EEG signals of all the trials are the same at the time point, and minimal when the phases at the time point are randomly distributed across the trials. For each auditory stimulation frequency (20, 30, and 40 Hz) and electrode (Fz, Cz, ad Pz), the signal epochs (trials) were band-pass filtered around the stimulation frequency (stimulation frequency ±5 Hz) and then Hilbert-transformed to obtain the analytic signal. Instantaneous ITC was obtained as the norm of the point-by-point average across trials of the normalized analytic signals. ITC values were averaged in the time window 50–550 ms after the onset of the auditory stimulation, and the average ITC of the baseline period (−300 to −50 ms) was subtracted from it.
Evoked power reflects both the magnitude of the brain’s voltage response to a stimulus/event and the consistency across trials of the time course of this time-locked response. For each auditory stimulation frequency and electrode, signal epochs (trials) were band-pass filtered (stimulation frequency ±5 Hz), averaged across trials in a point-by-point manner, and then Hilbert-transformed to obtain the analytic signal. Instantaneous evoked power was obtained by squaring the norm of the analytic signal. Evoked power was then averaged in the interval 50–550 ms after the onset of auditory stimulation, and the average power of the baseline period (−300 to −50 ms) was subtracted from it.
Behavioral Psychosis-Relevant Measures
Psychosis-relevant effects were captured with the Positive and Negative Syndrome Scale (PANSS) (Kay et al, 1989) positive, negative, general, and total scores that are known to be sensitive to the effects of Δ9-THC (Radhakrishnan et al, 2014).
General Procedure and Test Days
Test days were separated by 3 days to minimize carryover effects (see Supplementary Table 1). On the morning of each test day, subjects underwent drug and pregnancy testing. EEG was recorded during an ASSR task, administered before and when peak drug effects were expected to occur on each test day. In-study safety procedures and poststudy prospective safety assessments were performed; their results were reported in further detail elsewhere (Carbuto et al, 2011; D'Souza et al, 2004).
Statistical Analysis
Initially, data were examined descriptively using means, SDs, and graphs. For each drug condition (placebo, 0.015 mg/kg, and 0.03 mg/kg), EEG (evoked power and ITC) and behavioral (PANSS positive, negative, general, and total scores) measures were assessed for normality with the Kolmogorov–Smirnov test. Outliers were detected using a median absolute deviation (MAD)-based (Hampel, 1974) criterion that, compared with the common ‘standard deviations above the mean’ criterion, is highly robust against the presence of multiple outliers (Davies and Gather, 1993) (for further details, see Supplementary Text 2). Using this approach, no greater than 12% of the data for any outcome variable were excluded from the analysis.
Given that the auditory steady-state stimulation response was maximal at the electrode Cz, only this electrode was used for statistical analyses. EEG measures were obtained both before drug administration (baseline) and around predicted occurrence of peak drug effects. However, as there were no significant differences in predrug measures of ASSR between the 3 test days (for further details, see Supplementary Text 3), predrug data were not included in the analysis to detect drug effects.
The effects of Δ9-THC on ITC and evoked power were assessed using generalized estimating equations (GEE) with unstructured working correlation matrices (Liang and Zeger, 1986; Zeger and Liang, 1986). The effect of drug condition on each EEG measure (two measures: evoked power and ITC) was modeled by fitting three separate GEEs to the data, one for each stimulation frequency. For each EEG measure, the p-values of the GEE models were adjusted for three comparisons (one for each stimulation frequency) with the Holm–Bonferroni (HB) sequential procedure. The post hoc pairwise comparisons (0.03 mg/kg vs placebo, 0.015 mg/kg vs placebo, and 0.03 mg/kg vs 0.015 mg/kg) were performed for the GEE models with a significant main effect of drug condition in order to localize the source of the effect. For each EEG measure, p-values of the pairwise comparisons were HB adjusted in accordance with the total number of comparisons performed for the EEG measure (maximum possible number of comparisons for each EEG measure=9: 3 frequencies × 3 drug condition pairs).
To characterize the relationship (correlation) between the effects of Δ9-THC on both EEG (ITC and evoked power) and PANSS scores, longitudinal regressions were conducted on the data of both Δ9-THC-active conditions. The behavioral measures were regressed on the EEG measure/s presenting a significant main effect of drug by fitting GEE models with unstructured working correlation matrices to the data of both Δ9-THC-active conditions (maximum number of regressions =8: 2 EEG measures × 4 behavioral measures). Furthermore, in order to approximate the regression coefficients to partial correlation coefficients, standardized regression coefficient (βs) were obtained by transforming the data into composite z-scores before fitting the GEE models. To preserve the relative differences in the values of each variable between the two Δ9-THC-active conditions, composite z-scores were calculated using the mean and SD of the data of both Δ9-THC-active conditions pooled together. The p-values of the coefficients were HB adjusted for the total number of regression performed (maximum number =8). Analyses were done using SPSS 21 (IBM Corporation, Armonk, NY) and custom-made scripts in Matlab (MathWorks, Natick, MA).
RESULTS
The demographic and cannabis use data are listed in Table 1. Of the 56 subjects who initially consented for the study, 10 failed the screening process and 8 chose not to initiate the study. Of the remaining 38 subjects, 30 completed all 3 test days (21% dropout rate), of which 5 had to be dropped because of technical difficulties during EEG acquisition. There were no obvious differences between dropouts and completers (see Supplementary Table 2). Of the remaining 25 subjects, 2 were dropped during the EEG preprocessing because of artifactual contamination (for details, see Supplementary Text 1), and 3 were categorized as outliers and dropped during the statistical inspection of the EEG measures. Thus, EEG data from 20 subjects who completed all test days were used for statistical analyses. The inspection of the behavioral measures of these 20 subjects revealed one outlier for the PANSS general and total scores during the 0.015 mg/kg condition. This data point was excluded from the regression analyses (for details about the rejections of outliers, see Supplementary Text 2).
Table 1. Sample Demographics.
| General characteristics | ||
| No. of male (female) | 14 (6) | |
| Age (mean (SD)) | 25.700 (7.623) | |
| Handedness | 1 Left handed | |
| Years of education (mean (SD)) | 15.200 (2.142) | |
| Estimated IQ (mean (SD)) | 116.850 (3.883) | |
| Body mass index (mean (SD)) | 24.25 (2.99) | |
| Cannabis exposure | ||
| Age of first cannabis use | 16.150 (4.522) | |
| Days since last use (mean (SD) range) | 402.725 (854.634) 1–3650 | |
| Subgrouping (no. of subjects) | Recent users | 9 |
| Nonusers | 11 | |
| Frequency of cannabis use within past 30 days (no. of subjects) | 0 Days | 11 |
| 1–3 Days | 4 | |
| 4–8 Days | 1 | |
| 9–15 Days | 2 | |
| 16–29 Days | 2 | |
| Estimated lifetime exposure to cannabis (no. of subjects) | Only once | 0 |
| 2–5 Days | 1 | |
| 5–10 Days | 2 | |
| 11–20 Days | 4 | |
| 21–30 Days | 1 | |
| 31–50 Days | 1 | |
| 51–100 Days | 1 | |
| 101–200 Days | 1 | |
| 201–300 Days | 0 | |
| 301–500 Days | 4 | |
| 501–1000 Days | 2 | |
| >1000 Days | 3 | |
| Estimated cannabis exposure during heaviest use (no. of subjects) | <1 Per year | 1 |
| 1 Per year | 2 | |
| 1 Per 6 months | 4 | |
| 1 Per 3 months | 3 | |
| 1–3 Per month | 2 | |
| 1–2 Per week | 1 | |
| 3–6 Per week | 3 | |
| 7 Per week | 4 | |
| Other drug exposurea | ||
| Daily cigarette smokers (no. of subjects) | 1 | |
| Social cigarette smoker (no. of subjects) | 1 | |
| Average no. of alcoholic drinks per week (mean (SD)) | 6.01 (6.06) | |
| No exposure to other drugs (no. of subjects) | 6 | |
| Exposure to drugs other than cannabis (no. of subjects) | Psilocybin | 11 |
| LSD | 2 | |
| Salvinorin | 3 | |
| Nitrous oxide | 2 | |
| Cocaine | 5 | |
| Amphetamines | 3 | |
| MDMA | 2 | |
| Opioids | 2 | |
None of the subjects met criteria for abuse or dependence of tobacco, alcohol, and other drugs of abuse. Exposure to the drugs listed above was limited and remote.
Auditory Steady-State Response
Intertrial coherence
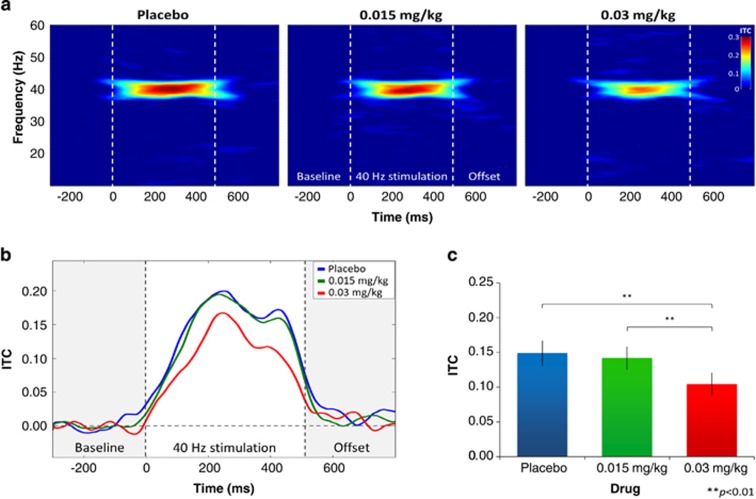
There was a HB-corrected significant main effect of dose on ITC with 40 Hz stimulation (Wald QUOTE (2)=12.677, pAdj=0.006). No significant main effect of dose was observed with the 20 and 30 Hz stimulation frequencies either before or after HB correction (psAdj>0.1). The post hoc analyses of the 40 Hz data revealed HB-corrected (3 comparisons) significantly lower ITC in the 0.03 mg/kg condition compared with the 0.015 mg/kg (pAdj=0.005) and the placebo (pAdj=0.002) conditions (Figure 1). No significant differences were found between the 0.015 mg/kg and the placebo conditions (pAdj>0.1). Means and SDs of the EEG measures are reported in Table 2.
Figure 1.
The 40 Hz intertrial coherence (ITC) per drug condition at electrode Cz. (a) Hilbert transform-based time–frequency plots for ITC (for details, see Supplementary Text 1). From left to right, the plots show the group-averaged time–frequency plots of the placebo, 0.015 mg/kg, and 0.03 mg/kg conditions during 40 Hz stimulation at electrode Cz. (b) Time course of the group-averaged ITC per drug condition at electrode Cz. The blue line represents the ITC of the placebo condition, whereas the green and red lines represent the ITC of the 0.015 and 0.03 mg/kg doses, respectively. (c) ITC (mean±SEM) by drug condition at electrode Cz during the time interval 50–550 ms after stimulation onset. **: Significant differences (pAdj<0.01) between drug conditions.
Table 2. Δ9-THC Effects on Intertrial Coherence (ITC) and Evoked Power.
| Measure | Placebo, M (SD) | 0.015 mg/kg, M (SD) | 0.03 mg/kg, M (SD) |
|---|---|---|---|
| Intertrial coherence | |||
| 40 Hz | 0.149 (0.082) | 0.142 (0.073) | 0.104 (0.073) |
| 30 Hz | 0.027 (0.042) | 0.042 (0.044) | 0.043 (0.043) |
| 20 Hz | 0.038 (0.040) | 0.030 (0.040) | 0.039 (0.041) |
| Evoked power (μV2) | |||
| 40 Hz | 0.288 (0.209) | 0.269 (0.167) | 0.196 (0.167) |
| 30 Hz | 0.075 (0.122) | 0.114 (0.137) | 0.107 (0.100) |
| 20 Hz | 0.252 (0.393) | 0.134 (0.178) | 0.184 (0.194) |
Evoked power
No significant main effect of dose on evoked power was observed with any stimulation frequency after HB correcting for multiple comparisons (pAdj>0.1). Before corrections a trend to significance was observed with 40 Hz stimulation (Wald QUOTE (2)=5.023, p=0.081), whereas no effects were detected with 20 and 30 Hz stimulation. Inspection of the means (Table 2) showed that in the 40 Hz condition, evoked power had a dose-related reduction as observed in ITC.
Behavioral and Subjective Effects
As reported elsewhere (D'Souza et al, 2012), Δ9-THC significantly increased PANSS positive, negative, general, and total scores (all ps<0.001). All doses were significantly different from each other at 10 min drug postinfusion for all these measures (all ps<0.01).
Relationship Between Electrophysiological Measures and Psychosis-Related Measures
There was a significant main effect of dose only for the 40 Hz stimulation ITC. Thus, only the 40 Hz ITC was used in the regressions of psychosis-relevant symptoms (PANSS scores) on EEG measures. Results were HB adjusted for four comparisons (ITC for 1 frequency × 4 psychosis-relevant measures).
Intertrial coherence
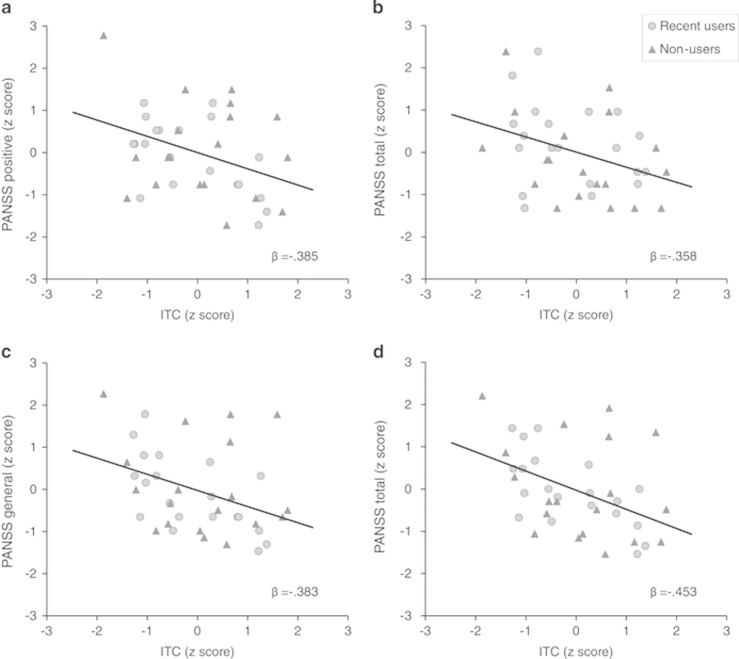
For the active Δ9-THC conditions, significant HB-adjusted inverse relationships were found between ITC and the (1) PANSS positive (β=−0.385, Wald χ2(1)=4.847, pAdj=0.028), (2) negative (β=−0.358, Wald χ2(1)=7.247, pAdj=0.021), (3) general (β=−0.383, Wald χ2(1)=5.618, pAdj=0.036), and (4) total (β=−0.453, Wald χ2(1)=11.800, pAdj=0.002) scores (Figure 2).
Figure 2.
Relationship between 40 Hz intertrial coherence (ITC) and psychosis-relevant measures under the effects of Δ9-THC. The scatter plots show the z-normalized values of the 40 Hz ITC (x axes) versus the PANSS (a) positive, (b) negative, (c) general, and (d) total scores (y axes) under the effects of Δ9-THC. The relationship between the variables is represented by the regression lines and the standardized regression coefficients (β). Data from recent users (past 30 days) and nonusers of cannabis are depicted as circles and triangles, respectively.
Exploratory Analyses on the Effects of Recent Cannabis Exposure
Exploratory analyses were conducted to determine the association between cannabis use in 30 days before study participation and the effects of acute Δ9-THC on ITC and evoked power. The sample was divided into those who reported using cannabis in the past 30 days (‘recent users’, n=9) and those who did not (‘nonusers’, n=11) as per (D'Souza et al, 2012). The effects of cannabis exposure (recent user vs nonuser) and the interaction between dose and cannabis exposure on each EEG measure (evoked power and ITC) were examined by fitting a GEE model with an unstructured working correlation matrix to the data. The post hoc analyses were performed whenever significant main effects or interaction effects were observed.
These exploratory analyses revealed that recent users of cannabis had lower ITC than nonusers at a trend level (group effect: p=0.07). As reported earlier, the dose effect was significant, but the group × dose interaction was not significant (Wald χ2(2)=2.328, p=0.312). Furthermore, recent users of cannabis had significantly lower evoked power than nonusers (Wald χ2(1)=5.188, p=0.023). As reported earlier the dose effect showed a trend toward significance but the group × dose interaction was not significant (Wald χ2(2)=2.372, p=0.306).
Plasma THC and THC-COOH Levels
For both active doses of Δ9-THC, there were significant (pAdj<0.001) increases in plasma levels of Δ9-THC and its metabolite THC-COOH (see Supplementary Figure 1 and Supplementary Text 4 for more information).
Safety
As reported elsewhere (D'Souza et al, 2012), there were five nonserious adverse events and no serious adverse events that occurred on test days.
DISCUSSION
To our knowledge, this is the first report of exogenous cannabinoids (i.v. Δ9-THC) disrupting evoked γ-band neural oscillations in humans. For the 40 Hz ASSR, there was a dose-dependent reduction of ITC, with the higher dose (0.03 mg/kg) showing reduced ITC compared with both the lower dose (0.015 mg/kg) and placebo. No significant effects of Δ9-THC were detected on the 20 or 30 Hz ASSRs, suggesting that cannabinoids selectively affected time-locked γ-band activity. Although not statistically significant, Δ9-THC also reduced evoked power.
These findings are similar to a large body of evidence from ASSR studies showing reduced ITC during γ-band stimulation (maximal effect at 40 Hz) and preserved response to 20 Hz stimulation in first-episode and chronic schizophrenia patients compared with healthy controls (Krishnan et al, 2009; Kwon et al, 1999; Light et al, 2006; Roach et al, 2012; Spencer et al, 2008a, 2008b).
Intertrial Coherence
ITC is a measure of the consistency in the phases of the brain’s oscillatory responses to a stimulus/event across different trials. Thus, as reflected by reductions in ITC, it seems that both schizophrenia and relevant phenomena acutely induced by Δ9-THC are associated with an increase in the intraindividual variability of the brain’s response to identical stimuli/events. This intraindividual variability may reflect greater randomness in the neural processes underlying the ASSR. As observed in schizophrenia, Δ9-THC-induced increased intraindividual variability was more pronounced at 40 than 20 Hz oscillations.
Relationship to Psychotomimetic Effects
Consistent with other studies, Δ9-THC induced psychotomimetic effects in a dose-dependent manner (D'Souza et al, 2004; Morrison et al, 2009). Thus, at doses that induce psychotomimetic effects, Δ9-THC concurrently disrupted evoked γ-band neural oscillations. Of note, there were robust (β=−0.35 to −0.45) inverse relationships between ITC and several subscales of the PANSS that assess symptoms relevant to schizophrenia.
The γ-band neural oscillations are essential for processes such as sensory registration, integration and binding of perceptual features, associative learning, and conscious awareness (for a review, see Cannon et al, 2014; Gandal et al, 2012; Uhlhaas et al, 2008; Uhlhaas and Singer, 2013). If disrupted, this could contribute to the Δ9-THC-induced psychotomimetic effects (Skosnik et al, 2006) captured by the PANSS. These observations are consistent with other reports of inverse relationships between clinical variables and measures of γ-band oscillations in schizophrenia. For example, in a study by Haig et al (2000), it was demonstrated that the magnitude of γ deficits in schizophrenia patients correlated with PANSS scores (one of the primary dependent measures in the current study) (Haig et al, 2000).
Neural Mechanisms Underlying Δ9-THC Effects on γ-Band Oscillations
Given the extensive crosstalk between the CB1R system and the GABAergic and glutamatergic systems, below herewith we speculate on how the latter two might be mechanistically involved in mediating the effects of Δ9-THC on γ-band oscillations.
The potential role of GABA
A large body of research has shown that GABAergic interneurons are the generators of neural oscillations in the γ-range (Buzsaki and Wang, 2012; Foldy et al, 2004; Gonzalez-Burgos and Lewis, 2008; Sohal, 2012; Uhlhaas and Singer, 2010; Wang, 2010). Furthermore, the sizeable branching of outputs from GABAergic interneurons are ideally suited to synchronize large numbers of pyramidal cells (Cobb et al, 1995). However, there are diverse types of GABAergic interneurons based upon their electrophysiological characteristics, their expression of calcium-binding proteins, and/or whether or not they are ‘fast’ or ‘non-fast’ spiking neurons. The fast-spiking parvalbumin (PV)-expressing interneurons appear to be the primary generator of neural oscillations in the brain (Curley and Lewis, 2012; Sohal, 2012; Sohal et al, 2009). PV cells typically target the pyramidal cell axon initial segment and cell body, thus positioning their terminals in an optimal location to synchronize numerous pyramidal cells. The non-fast spiking CCK-positive interneurons are in a prime location to ‘fine-tune’ the network oscillations generated by PV cells (Freund, 2003). Germane to the current study, CCK-positive interneurons cells appear to be the only cortical and hippocampal interneuron type to express CB1Rs (Ali and Todorova, 2010; Bacci et al, 2004; Bodor et al, 2005; Eggan and Lewis, 2007; Eggan et al, 2010; Foldy et al, 2006; Hill et al, 2007; Katona et al, 2000). CCK-positive interneurons also target pyramidal cell bodies, putting them in an ideal location to modulate PV to pyramidal cell oscillations (Keimpema et al, 2012). Furthermore, CCK cells themselves have collaterals that provide input onto PV cells (Karson et al, 2009). Thus, whereas PV interneurons are involved in the generation of γ-rhythms (like a ‘metronome’), CCK interneurons enhance the signal-to-noise ratio of γ—activity through a CB1R-mediated mechanism (Bartos and Elgueta, 2012; Csicsvari et al, 2003; Tukker et al, 2007).
Under physiological conditions, the release of neurotransmitters such as GABA or glutamate results in the on-demand synthesis of endocannabinoids that travel retrogradely to activate presynaptic CB1R. The activation of these presynaptic CB1Rs results in the inhibition of further neurotransmitter release. In the case of CCK interneurons this would lead to the disinhibition of PCs. Only PCs that are strongly recruited by a stimulus/task (signal) can mount an adequate endocannabinoid release to overcome CCK-BC-mediated inhibition (Bartos and Elgueta, 2012; Wilson and Nicoll, 2002). Conversely, PCs that are weakly recruited by a stimulus/task (noise) will not be able to overcome the CCK-BC-mediated inhibition, and thus their random activity will remain inhibited (ie, their contribution is ‘filtered’ out).
In contrast to endocannabinoids that are synthesized on demand, released locally, and quickly removed after release, the administration of exogenous cannabinoids such as Δ9-THC produces long-lasting and less localized effects. This nonphysiological activation of CB1Rs on CCK-positive interneurons by Δ9-THC will therefore interfere with the fine-tuning of network oscillations. Although admittedly speculative, interference with the fine-tuning of network oscillations would be expected to disrupt sensory, perceptual, and cognitive functions, leading to psychosis-like phenomena. Confirming this postulate, the current study found that 40 Hz ITC during high-dose THC inversely correlated with PANSS scores. Hence, although this finding of an association between disruptions in neural oscillations and psychosis does not prove a causal relationship, these data suggest a potential relationship between THC-induced disruption in γ-oscillations and measures of psychosis.
The potential role of glutamate
In addition to the suppression of GABA release from CCK-positive interneurons, cannabinoids can disrupt stimulus-locked γ-band responses by suppressing glutamate release from PCs through the activation of CB1Rs located on their synaptic terminals (Holderith et al, 2011; Katona et al, 2006; Kawamura et al, 2006). In vitro evidence shows that the CB1R-mediated reduction of glutamate release onto PCs and fast-spiking PV-BCs decreases γ-band local field potentials (spectral power) by reducing the firing rate and by increasing the temporal variability (randomness) of spiking (with respect to the phase of local field potentials) of both types of postsynaptic neurons (Holderith et al, 2011).
Impact of Cannabis Exposure
The limited power to examine the influence of cannabis exposure in this study notwithstanding, the results of the current study suggest that individuals with a recent (past 30 days) history of cannabis exposure had blunted responses to the disruptive effects of Δ9-THC on ITC and evoked power. These findings are consistent with the observation that relatively limited exposure to cannabis is associated with a blunted response to the effects of Δ9-THC across behavioral, subjective, cognitive (memory), neuroendocrine (cortisol), and neurochemical (brain-derived neurotrophic factor (BDNF)) outcomes (D'Souza et al, 2008a, b, 2009; Ranganathan et al, 2009). This is likely related to the known tolerance and CB1R downregulation that occurs after repeated cannabis exposure (Gonzalez et al, 2005; Hirvonen et al, 2012; Jones et al, 1981). Interestingly, recent cannabis use did not influence the disruptive effects of Δ9-THC on P300a/b amplitude and P300b latency (D'Souza et al, 2012) suggesting that measures of ITC and evoked power might be more sensitive to Δ9-THC effects.
Strengths, Limitations, and Conclusions
This study has several strengths and some limitations. The i.v. route of administration and the weight-adjusted dose addressing the inter- and intraindividual variability associated with oral or smoked Δ9-THC is a strength. Furthermore, the use of multiple doses allowed for establishing a dose–response relationship. The exclusion of heavy cannabis users who are likely tolerant to Δ9-THC effects (D'Souza et al, 2008b) also maximized the chance to capture acute Δ9-THC effects on neural oscillations. Finally, the use of novel preprocessing techniques (described in the Supplementary Text 1) to clean the muscular artifacts that frequently contaminate EEG data allowed more data to be retained, resulting in increased signal-to-noise ratio of evoked measures (Van Drongelen, 2006) and reduced the likelihood of spurious findings (Goncharova et al, 2003). There are some limitations regarding the use of EEG that should be taken into account. Despite the fact that muscular and ocular artifactual activity was minimized by preprocessing, it is not possible to rule out the possibility that some drug-induced effects may have been either obscured or erroneously boosted by residual artifactual activity. Furthermore, because of dropouts and the process of removing artifacts, not all the data that could have been used were available for analysis. This should be considered when interpreting the lack of statistically significant effects on some outcomes including power. The study may have had limited power to detect Δ9-THC effects on evoked power. Therefore, in order to characterize the acute effect of cannabinoid agonists on the ASSR in humans, future studies with a larger sample, the inclusion of a sufficient sample of subjects with a wide range of cannabis exposure, and the inclusion of cognitive measures that are influenced by γ-band oscillations are warranted.
In summary, we show for the first time in humans that exogenous cannabinoids acutely disrupt evoked γ-band neural oscillations that are essential for processes such as sensory registration, integration and binding of perceptual features, associative learning, and conscious awareness. Furthermore, we show a relationship between the disruption of neural oscillations and the presence of abnormalities in these cognitive processes similar to the ones observed in psychosis.
FUNDING AND DISCLOSURE
Jose Cortes-Briones, Patrick Skosnik, John Cahill, Ashley Williams, Brian Roach, Mohini Ranganathan, and R Andrew Sewell (deceased) declare no conflict of interest. Deepak Cyril D’Souza has in the past 3 years or currently receives research grant support administered through Yale University School of Medicine from AbbVie and Pfizer, and is a consultant for Bristol-Myers Squibb and Johnson and Johnson. Dr Mathalon is a consultant for Bristol-Myers Squibb, and Amgen.
Acknowledgments
We acknowledge support from the (1) Department of Veterans Affairs, (2) National Institute of Mental Health, (3) National Institute of Drug Abuse, (4) National Institute of Alcoholism and Alcohol Abuse (NIAAA) and (5) the Yale Center for Clinical Investigation (YCCI). This research project was funded in part by grants from NIDA (R21 DA020750 to DCD) and a NARSAD Young Investigator Award to PDS. We also thank Angelina Genovese, Michelle San Pedro, Elizabeth O’Donnell, Brenda Breault, Sonah Yoo, Rachel Galvan, and Willie Ford of the Neurobiological Studies Unit at the VA Connecticut Healthcare System, West Haven Campus, for their central contributions to the success of this project. Finally, this paper is dedicated to the memory of our dear friend and colleague, the late Dr R Andrew Sewell.
Footnotes
Supplementary Information accompanies the paper on the Neuropsychopharmacology website (http://www.nature.com/npp)
Supplementary Material
References
- Ali AB, Todorova M (2010). Asynchronous release of GABA via tonic cannabinoid receptor activation at identified interneuron synapses in rat CA1. Eur J Neurosci 31: 1196–1207. [DOI] [PubMed] [Google Scholar]
- Bacci A, Huguenard JR, Prince DA (2004). Long-lasting self-inhibition of neocortical interneurons mediated by endocannabinoids. Nature 431: 312–316. [DOI] [PubMed] [Google Scholar]
- Bartos M, Elgueta C (2012). Functional characteristics of parvalbumin‐and cholecystokinin‐expressing basket cells. J Physiol 590: 669–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodor AL, Katona I, Nyiri G, Mackie K, Ledent C, Hajos N et al (2005). Endocannabinoid signaling in rat somatosensory cortex: laminar differences and involvement of specific interneuron types. J Neurosci 25: 6845–6856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buzsaki G, Wang XJ (2012). Mechanisms of gamma oscillations. Annu Rev Neurosci 35: 203–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cannon J, McCarthy MM, Lee S, Lee J, Borgers C, Whittington MA et al (2014). Neurosystems: brain rhythms and cognitive processing. Eur J Neurosci 39: 705–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carbuto M, Sewell RA, Williams A, Forselius-Bielen K, Braley G, Elander J et al (2011). The safety of studies with intravenous Delta(9)-tetrahydrocannabinol in humans, with case histories. Psychopharmacology (Berl) 219: 885–896. [DOI] [PubMed] [Google Scholar]
- Cobb SR, Buhl EH, Halasy K, Paulsen O, Somogyi P (1995). Synchronization of neuronal activity in hippocampus by individual GABAergic interneurons. Nature 378: 75–78. [DOI] [PubMed] [Google Scholar]
- Csicsvari J, Jamieson B, Wise KD, Buzsáki G (2003). Mechanisms of gamma oscillations in the hippocampus of the behaving rat. Neuron 37: 311–322. [DOI] [PubMed] [Google Scholar]
- Curley AA, Lewis DA (2012). Cortical basket cell dysfunction in schizophrenia. J Physiol 590: 715–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Souza DC, Braley G, Blaise R, Vendetti M, Oliver S, Pittman B et al (2008. a). Effects of haloperidol on the behavioral, subjective, cognitive, motor, and neuroendocrine effects of Delta-9-tetrahydrocannabinol in humans. Psychopharmacology (Berl) 198: 587–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Souza DC, Fridberg DJ, Skosnik PD, Williams A, Roach B, Singh N et al (2012). Dose-related modulation of event-related potentials to novel and target stimuli by intravenous Δ9-THC in humans. Neuropsychopharmacology 37: 1632–1646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Souza DC, Perry E, MacDougall L, Ammerman Y, Cooper T, Wu YT et al (2004). The psychotomimetic effects of intravenous delta-9-tetrahydrocannabinol in healthy individuals: implications for psychosis. Neuropsychopharmacology 29: 1558–1572. [DOI] [PubMed] [Google Scholar]
- D'Souza DC, Pittman B, Perry E, Simen A (2009). Preliminary evidence of cannabinoid effects on brain-derived neurotrophic factor (BDNF) levels in humans. Psychopharmacology (Berl) 202: 569–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Souza DC, Ranganathan M, Braley G, Gueorguieva R, Zimolo Z, Cooper T et al (2008. b). Blunted psychotomimetic and amnestic effects of Delta-9-tetrahydrocannabinol in frequent users of cannabis. Neuropsychopharmacology 33: 2505–2516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies L, Gather U (1993). The identification of multiple outliers. J Am Stat Assoc 88: 782–792. [Google Scholar]
- De Clercq W, Vergult A, Vanrumste B, Van Paesschen W, Van Huffel S (2006). Canonical correlation analysis applied to remove muscle artifacts from the electroencephalogram. IEEE Trans Biomed Eng 53: 2583–2587. [DOI] [PubMed] [Google Scholar]
- Delorme A, Makeig S (2004). EEGLAB: an open source toolbox for analysis of single-trial EEG dynamics including independent component analysis. J Neurosci Methods 134: 9–21. [DOI] [PubMed] [Google Scholar]
- Eggan SM, Lewis DA (2007). Immunocytochemical distribution of the cannabinoid CB1 receptor in the primate neocortex: a regional and laminar analysis. Cereb Cortex 17: 175–191. [DOI] [PubMed] [Google Scholar]
- Eggan SM, Melchitzky DS, Sesack SR, Fish KN, Lewis DA (2010). Relationship of cannabinoid CB1 receptor and cholecystokinin immunoreactivity in monkey dorsolateral prefrontal cortex. Neuroscience 169: 1651–1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW (2002) Structured Clinical Interview for DSM-IV-TR Axis I Disorders- Non-Patient Edition. American Psychiatric Association: Washington, DC. [Google Scholar]
- Foldy C, Aradi I, Howard A, Soltesz I (2004). Diversity beyond variance: modulation of firing rates and network coherence by GABAergic subpopulations. Eur J Neurosci 19: 119–130. [DOI] [PubMed] [Google Scholar]
- Foldy C, Neu A, Jones MV, Soltesz I (2006). Presynaptic, activity-dependent modulation of cannabinoid type 1 receptor-mediated inhibition of GABA release. J Neurosci 26: 1465–1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freund TF (2003). Interneuron Diversity series: Rhythm and mood in perisomatic inhibition. Trends Neurosci 26: 489–495. [DOI] [PubMed] [Google Scholar]
- Gandal MJ, Edgar JC, Klook K, Siegel SJ (2012). Gamma synchrony: towards a translational biomarker for the treatment-resistant symptoms of schizophrenia. Neuropharmacology 62: 1504–1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gómez-Herrero G, De Clercq W, Anwar H, Kara O, Egiazarian K, Van Huffel S (eds) (2006). Automatic removal of ocular artifacts in the EEG without an EOG reference channel. Signal Processing Symposium, 2006. NORSIG 2006. Proceedings of the 7th Nordic. IEEE. [Google Scholar]
- Goncharova I, McFarland DJ, Vaughan TM, Wolpaw JR (2003). EMG contamination of EEG: spectral and topographical characteristics. Clin Neurophysiol 114: 1580–1593. [DOI] [PubMed] [Google Scholar]
- Gonzalez-Burgos G, Lewis DA (2008). GABA neurons and the mechanisms of network oscillations: implications for understanding cortical dysfunction in schizophrenia. Schizophr Bull 34: 944–961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez S, Cebeira M, Fernandez-Ruiz J (2005). Cannabinoid tolerance and dependence: a review of studies in laboratory animals. Pharmacol Biochem Behav 81: 300–318. [DOI] [PubMed] [Google Scholar]
- Haig AR, Gordon E, De Pascalis V, Meares RA, Bahramali H, Harris A (2000). Gamma activity in schizophrenia: evidence of impaired network binding? Clin Neurophysiol 111: 1461–1468. [DOI] [PubMed] [Google Scholar]
- Hajos M, Hoffmann WE, Kocsis B (2008). Activation of cannabinoid-1 receptors disrupts sensory gating and neuronal oscillation: relevance to schizophrenia. Biol Psychiatry 63: 1075–1083. [DOI] [PubMed] [Google Scholar]
- Hajos N, Katona I, Naiem SS, MacKie K, Ledent C, Mody I et al (2000). Cannabinoids inhibit hippocampal GABAergic transmission and network oscillations. Eur J Neurosci 12: 3239–3249. [DOI] [PubMed] [Google Scholar]
- Hampel FR (1974). The influence curve and its role in robust estimation. J Am Stat Assoc 69: 383–393. [Google Scholar]
- Hill EL, Gallopin T, Ferezou I, Cauli B, Rossier J, Schweitzer P et al (2007). Functional CB1 receptors are broadly expressed in neocortical GABAergic and glutamatergic neurons. J Neurophysiol 97: 2580–2589. [DOI] [PubMed] [Google Scholar]
- Hirvonen J, Goodwin RS, Li CT, Terry GE, Zoghbi SS, Morse C et al (2012). Reversible and regionally selective downregulation of brain cannabinoid CB1 receptors in chronic daily cannabis smokers. Mol Psychiatry 17: 642–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holderith N, Nemeth B, Papp OI, Veres JM, Nagy GA, Hajos N (2011). Cannabinoids attenuate hippocampal gamma oscillations by suppressing excitatory synaptic input onto CA3 pyramidal neurons and fast spiking basket cells. J Physiol 589: 4921–4934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson LA, Johnson RL, Alfonzo C (2011). Spice: a legal marijuana equivalent. Mil Med 176: 718–720. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O'Malley PM, Bachman HG, Schulenberg JE (2012) Monitoring the Future National Results on Adolescent Drug Use: Overview of Key Findings, 2011. Institute for Social Research, The University of Michigan: Ann Arbor. [Google Scholar]
- Jones RT, Benowitz NL, Herning RI (1981). Clinical relevance of cannabis tolerance and dependence. J Clin Pharmacol 21: 143S–152S. [DOI] [PubMed] [Google Scholar]
- Karson MA, Tang AH, Milner TA, Alger BE (2009). Synaptic cross talk between perisomatic-targeting interneuron classes expressing cholecystokinin and parvalbumin in hippocampus. J Neurosci 29: 4140–4154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katona I, Sperlagh B, Magloczky Z, Santha E, Kofalvi A, Czirjak S et al (2000). GABAergic interneurons are the targets of cannabinoid actions in the human hippocampus. Neuroscience 100: 797–804. [DOI] [PubMed] [Google Scholar]
- Katona I, Urban GM, Wallace M, Ledent C, Jung KM, Piomelli D et al (2006). Molecular composition of the endocannabinoid system at glutamatergic synapses. J Neurosci 26: 5628–5637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawamura Y, Fukaya M, Maejima T, Yoshida T, Miura E, Watanabe M et al (2006). The CB1 cannabinoid receptor is the major cannabinoid receptor at excitatory presynaptic sites in the hippocampus and cerebellum. J Neurosci 26: 2991–3001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kay SR, Opler LA, Lindenmayer JP (1989). The Positive and Negative Syndrome Scale (PANSS): rationale and standardisation. Br J Psychiatry Suppl 59–67. [PubMed]
- Keimpema E, Straiker A, Mackie K, Harkany T, Hjerling-Leffler J (2012). Sticking out of the crowd: the molecular identity and development of cholecystokinin-containing basket cells. J Physiol 590: 703–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleber HD, DuPont RL (2012). Physicians and medical marijuana. Am J Psychiatry 169: 564–568. [DOI] [PubMed] [Google Scholar]
- Krishnan GP, Hetrick WP, Brenner CA, Shekhar A, Steffen AN, O'Donnell BF (2009). Steady state and induced auditory gamma deficits in schizophrenia. NeuroImage 47: 1711–1719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon JS, O'Donnell BF, Wallenstein GV, Greene RW, Hirayasu Y, Nestor PG et al (1999). Gamma frequency-range abnormalities to auditory stimulation in schizophrenia. Arch Gen Psychiatry 56: 1001–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang K-Y, Zeger SL (1986). Longitudinal data analysis using generalized linear models. Biometrika 73: 13–22. [Google Scholar]
- Light GA, Hsu JL, Hsieh MH, Meyer-Gomes K, Sprock J, Swerdlow NR et al (2006). Gamma band oscillations reveal neural network cortical coherence dysfunction in schizophrenia patients. Biol Psychiatry 60: 1231–1240. [DOI] [PubMed] [Google Scholar]
- Mehmedic Z, Chandra S, Slade D, Denham H, Foster S, Patel AS et al (2010). Potency trends of Delta9-THC and other cannabinoids in confiscated cannabis preparations from 1993 to 2008. J Forensic Sci 55: 1209–1217. [DOI] [PubMed] [Google Scholar]
- Morgan NH, Stanford IM, Woodhall GL (2008). Modulation of network oscillatory activity and GABAergic synaptic transmission by CB1 cannabinoid receptors in the rat medial entorhinal cortex. Neural Plast 2008: 808564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison PD, Zois V, McKeown DA, Lee TD, Holt DW, Powell JF et al (2009). The acute effects of synthetic intravenous Delta9-tetrahydrocannabinol on psychosis, mood and cognitive functioning. Psychol Med 39: 1607–1616. [DOI] [PubMed] [Google Scholar]
- ONDCP (2008). Marijuana: The Greatest Cause of Illegal Drug Abuse. The Marijuana Factbook. Executive Office of the President Washington: DC, 20503. [Google Scholar]
- Partha M, Hemant B (2007) Observed Brain Dynamics. Oxford University Press: New York. [Google Scholar]
- Procon.org (2014). Medical marijuana http://medicalmarijuana.procon.org/ Vol. 2014.
- Puthusserypady S, Ratnarajah T (2005). H∞ adaptive filters for eye blink artifact minimization from electroencephalogram. Signal Processing Lett IEEE 12: 816–819. [Google Scholar]
- Radhakrishnan R, Wilkinson ST, D’Souza DC (2014). Gone to pot–a review of the association between cannabis and psychosis. Front Psychiatry 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranganathan M, Braley G, Pittman B, Cooper T, Perry E, Krystal J et al (2009). The effects of cannabinoids on serum cortisol and prolactin in humans. Psychopharmacology (Berl) 203: 737–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roach B, Ford J, Hoffman R, Mathalon D (2012). Converging evidence for gamma synchrony deficits in schizophrenia. Suppl Clin Neurophysiol 62: 163–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robbe D, Montgomery SM, Thome A, Rueda-Orozco PE, McNaughton BL, Buzsaki G (2006). Cannabinoids reveal importance of spike timing coordination in hippocampal function. Nat Neurosci 9: 1526–1533. [DOI] [PubMed] [Google Scholar]
- Sales-Carbonell C, Rueda-Orozco PE, Soria-Gomez E, Buzsaki G, Marsicano G, Robbe D (2013). Striatal GABAergic and cortical glutamatergic neurons mediate contrasting effects of cannabinoids on cortical network synchrony. Proc Natl Acad Sci USA 110: 719–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA (2011) Results from the 2010 National Survey on Drug Use and Health: Summary of National Findings. Substance Abuse and Mental Health Services Administration: Rockville, MD. [Google Scholar]
- SAMHSA (2012) Drug Abuse Warning Network, 2010: National Estimates of Drug-Related Emergency Department Visits. Center for Behavioral Health Statistics and Quality (formerly the Office of Applied Studies), Substance Abuse and Mental Health Services Administration (SAMHSA): Rockville, MD. [Google Scholar]
- Skosnik P, Krishnan G, Aydt E, Kuhlenshmidt H, O’Donnell B (2006). Psychophysiological evidence of altered neural synchronization in cannabis use: relationship to schizotypy. Am J Psychiatry 163: 1798–1805. [DOI] [PubMed] [Google Scholar]
- Skosnik PD, D'Souza DC, Steinmetz AB, Edwards CR, Vollmer JM, Hetrick WP et al (2012). The effect of chronic cannabinoids on broadband EEG neural oscillations in humans. Neuropsychopharmacology 37: 2184–2193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohal VS (2012). Insights into cortical oscillations arising from optogenetic studies. Biol Psychiatry 71: 1039–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohal VS, Zhang F, Yizhar O, Deisseroth K (2009). Parvalbumin neurons and gamma rhythms enhance cortical circuit performance. Nature 459: 698–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer KM, Salisbury DF, Shenton ME, McCarley RW (2008. a). Gamma-band auditory steady-state responses are impaired in first episode psychosis. Biol Psychiatry 64: 369–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer KM, Salisbury DF, Shenton ME, McCarley RW (2008. b). γ-Band auditory steady-state responses are impaired in first episode psychosis. Biol Psychiatry 64: 369–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tallon-Baudry C, Bertrand O, Delpuech C, Pernier J (1996). Stimulus specificity of phase-locked and non-phase-locked 40 Hz visual responses in human. J Neurosci 16: 4240–4249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tukker JJ, Fuentealba P, Hartwich K, Somogyi P, Klausberger T (2007). Cell type-specific tuning of hippocampal interneuron firing during gamma oscillations in vivo. J Neurosci 27: 8184–8189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uhlhaas PJ, Haenschel C, Nikolić D, Singer W (2008). The role of oscillations and synchrony in cortical networks and their putative relevance for the pathophysiology of schizophrenia. Schizophr Bull 34: 927–943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uhlhaas PJ, Singer W (2010). Abnormal neural oscillations and synchrony in schizophrenia. Nat Rev Neurosci 11: 100–113. [DOI] [PubMed] [Google Scholar]
- Uhlhaas PJ, Singer W (2013). High-frequency oscillations and the neurobiology of schizophrenia. Dialogues Clin Neurosci 15: 301–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Drongelen W (2006) Signal Processing for Neuroscientists: An Introduction to the Analysis of Physiological Signals. Academic Press: Burlington, MA, USA. [Google Scholar]
- Vardakou I, Pistos C, Spiliopoulou C (2010). Spice drugs as a new trend: mode of action, identification and legislation. Toxicol Lett 197: 157–162. [DOI] [PubMed] [Google Scholar]
- Wang XJ (2010). Neurophysiological and computational principles of cortical rhythms in cognition. Physiol Rev 90: 1195–1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson ST, D’Souza D (2014). Problems with the medicalization of marijuana. JAMA 311: 2377–2378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson RI, Nicoll RA (2002). Endocannabinoid signaling in the brain. Science 296: 678–682. [DOI] [PubMed] [Google Scholar]
- Zeger SL, Liang K-Y (1986). Longitudinal data analysis for discrete and continuous outcomes. Biometrics 42: 121–130. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.