Abstract
In the wake of the ongoing 2014/2015 Ebola virus outbreak, significant questions regarding the appropriate handling of Ebola virus-contaminated liquid waste remain, including the persistence of Ebola virus in wastewater. To address these uncertainties, we evaluated the persistence of Ebola virus spiked in sterilized domestic sewage. The viral titer decreased approximately 99% within the first test day from an initial viral titer of 106 TCID50 mL–1; however, it could not be determined if this initial rapid decrease was due to aggregation or inactivation of the viral particles. The subsequent viral titer decrease was less rapid, and infectious Ebola virus particles persisted for all 8 days of the test. The inactivation constant (k) was determined to be −1.08 (2.1 days for a 90% viral titer decrease). Due to experimental conditions, we believe these results to be an upper bound for Ebola virus persistence in wastewater. Wastewater composition is inherently heterogeneous; subsequently, we caution that interpretation of these results should be made within a holistic assessment, including the effects of wastewater composition, dilution, and potential exposure routes within wastewater infrastructure. While it remains unknown if Ebola virus may be transmitted via wastewater, these data demonstrate a potential exposure route to infectious Ebola virus via wastewater and emphasize the value of a precautionary approach to wastewater handling in an epidemic response.
Introduction
In March 2014, an unprecedented outbreak of Ebola virus disease (EVD) began in Western Africa that as of July 2015 is ongoing and has claimed more than 11000 lives.1 The current outbreak is caused by viruses belonging to the species of the Zaire ebolavirus, a member of the Filoviridae family.2,3 Filoviridae are enveloped, filamentous viruses with lengths that may reach >1000 nm.4,5 The current outbreak has a reported case fatality rate of 51%.6 Ebola virus can be excreted in bodily fluids, including vomit, stool, blood, saliva, semen, and breast milk.7−9 Ebola virus loads of up to 108 genome copies mL–1 have been reported in blood, 107 genome copies mL–1 in stool, and 105.5 genome copies mL–1 in urine;10 however, the conversion between genome copies and infectious units is unknown. The median infectious dose is believed to be <10 infectious viral particles.11 Once infected, individuals may produce up to 9 L of liquid waste per day,12 primarily watery diarrhea.13 Ebola virus is considered a potential bioterrorism agent.17,18
In response to the EVD epidemic, both the World Health Organization (WHO) and the U.S. Centers for Disease Control and Prevention advised direct disposal of Ebola-contaminated liquid waste into sewage systems (wastewater collection and treatment systems) and latrines without disinfection.14 Initial recommendations were made on the basis of an expected limited persistence of Ebola virus in the environment, as Ebola virus is an enveloped virus, and a lack of strong evidence for a waterborne transmission route. As stated by a WHO guidance document, “Ebola virus is likely to inactivate significantly faster in the environment than enteric viruses with known waterborne transmission (e.g., norovirus, hepatitis A virus)”.14 However, as has been noted in a recent review, the persistence of enveloped viruses in the water environment varies by >2 orders of magnitude.15 Recommendations for Ebola virus-contaminated wastewater disposal were met with debate (e.g., refs (16−18)) because of uncertainty about Ebola virus persistence within wastewater matrices and the lack of a risk-based analysis for waste handling. Wastewater handling recommendations have since been revised to recognize uncertainty in this area and to recommend disinfection of latrines and holding of wastewater prior to handling to allow Ebola virus inactivation.19−21 Additionally, some facilities have opted to provide additional disinfection prior to disposal of liquid waste into sewer systems.12 Recent research found both ethanol and hypochlorite to be effective disinfectants for Ebola virus dried on surfaces;22 however, the disinfection kinetics of Ebola virus within liquid matrices remains unknown. Various wastewater disinfection approaches have been recently suggested for pathogen control in an outbreak setting.23
Currently, no data on Ebola virus persistence in wastewater exist, hindering risk estimation and examination of potential environmental exposure routes. The necessity of evaluating Ebola virus persistence in wastewater matrices has previously been highlighted, as wastewater in Ebola virus outbreak settings may be temporarily held in open containers or disposed of in open sewers.24 Historically, the transmission of Ebola virus via environmental routes (droplets, aerosols, or fomites) has been thought to be unlikely due to epidemiological evidence and environmental sampling.24 The primary Ebola virus transmission route is via direct contact with bodily fluids.24 Transmission has previously occurred without known direct contact with infected individuals,25 providing supporting evidence that Ebola virus transmission may be possible via large droplets.24 The potential for transmission of Ebola virus via wastewater is currently unknown.
To address uncertainties regarding Ebola virus persistence in wastewater, we have conducted an initial evaluation of Ebola virus persistence within wastewater to address uncertainty and inform ongoing risk assessments. A current Ebola virus outbreak strain from Guinea (Makona-WPGC07) was spiked to two end concentrations (102 and 106 TCID50 mL–1) into a domestic wastewater (untreated sewage) sample. The Ebola virus-containing wastewater was sampled for 8 days, and the viability of Ebola virus was determined in these samples. Study results are presented, and study limitations and implications are discussed, as well as recommendations for an ongoing research agenda.
Methods
Untreated wastewater was collected from an anonymous regional wastewater treatment facility in western Pennsylvania that receives wastewater from seven communities (combined population of approximately 60000). The total raw wastewater flow to the treatment facility is <10 MGD (million gallons per day). Approximately 8% of the raw wastewater originates from industrial sources. Following collection, the wastewater was frozen at −80 °C to minimize compositional changes prior to analysis. Wastewater characteristics (Table 1) were determined at an EPA-certified analysis facility (Microbac Laboratories, Marietta, OH). The region from which the sample was collected uses a combined sewer system that experiences significant infiltration, and the determined composition is typical for the region.
Table 1. Composition of the Wastewater Evaluateda.
| constituent | tested wastewater |
|---|---|
| pH | 8.6 |
| chemical oxygen demand (mg/L) | 125 ± 8 |
| ammonia (mg/L) | 21.5 ± 1.3 |
| phosphorus (mg/L) | 4.3 ± 0.7 |
| total organic carbon (mg/L) | 39 ± 5 |
| total suspended solids (mg/L) | 124 ± 9 |
The error gives the 95% confidence interval. Values measured prior to γ-irradiation disinfection.
Ebola virus cultivation experiments were conducted at Rocky Mountain Laboratories under BSL4 conditions. Wastewater samples were shipped to Rocky Mountain Laboratories overnight on ice. Upon receipt, samples were sterilized with 5 Mrad of γ-irradiation. Sterilization was performed to limit cell culture death due to wastewater microbial activity leading to a false positive. Stock virus (Ebola virus Guinea Makona-WPGC07, 107.3 TCID50 mL–1)26 was handled as described previously.27 Ebola virus was diluted in wastewater to achieve two separate virus titers (106 and 102 TCID50 mL–1), and both experiments were completed in triplicate. The Ebola virus concentration in sewage has not been previously measured or estimated; thus, two separate concentrations were utilized to cover possible concentration scenarios. TCID50 is an end point dilution series that is used to determine at what dilution 50% of the infected wells produce cell death. The original infectious titer can be calculated utilizing the Spearman–Karber method.28 An approximation of focus-forming units (FFUs) can be made from a Poisson distribution utilizing the formula TCID50 × 0.69, assuming each FFU is formed from a single virus. Spiked wastewater was then distributed into three labeled vials for each concentration, and samples were taken daily for 8 days. Tests were conducted at 20 °C and 40% relative humidity. At each time point, including the time zero measurement, 50 μL of wastewater from the bulk wastewater vial was added into 450 μL of Dulbecco’s modified Eagle’s medium (DMEM, Sigma) supplemented with heat-inactivated fetal bovine serum (FBS, Gibco) to a final concentration of 2%, Pen/Strep (Gibco) to a final concentration of 50 units/mL penicillin and 50 μg/mL streptomycin, and l-glutamine (Gibco) to a final concentration of 2 mM in an appropriately labeled 2 mL screw top vial and frozen at −80 °C. Negative controls were 50 μL of nonspiked wastewater in 450 μL of DMEM. To perform the titrations, a 96-well 1.1 mL well dilution plate (Axygen, Corning, NY) was prepared. The thawed sample (400 μL) was placed in the top row of the plate and a 10-fold dilution conducted by passing 40 μL of sample into 360 μL of DMEM. Next, 100 μL from each well of the dilution plate was transferred to a 96-well cell culture plate seeded with Vero cells. The cells were incubated with virus dilutions for 1 h; then the medium was removed from the two highest concentrations and rinsed two times with PBS, and 200 μL of fresh culture medium was added. Fresh culture medium (100 μL) was also added to the remaining wells in the plate. The plates were incubated at 37 °C for 7 days, inspected for the cytopathic effect (CPE), and scored. Statistical analyses and graphing were completed with Microsoft Excel 2011. The natural logarithm of C/Co TCID50 was plotted and fit with a linear trendline for estimation of the inactivation constant (k). A literature review was then performed to compare observed inactivation to other environmental matrices.
Results and Discussion
Ebola Virus Persistence in Wastewater
Ebola virus was spiked into wastewater at two concentrations and assayed for 8 days to determine persistence in a wastewater matrix. The time zero time point was measured immediately following addition of Ebola virus to the wastewater. No viable Ebola virus was recovered from samples spiked with 102 Ebola virus TCID50 mL–1 after the initial time zero sampling. The limit of detection was 0.75 log10 TCID50 mL–1. Virus viabilities from the initial 106 Ebola virus TCID50 mL–1 concentration are shown in Figure 1 and detailed in Table S1. Viable Ebola virus persisted for all 8 days of the test. Ebola virus titer was rapidly reduced (approximately 99%) within the first day of the test, consistent with an inability to identify infectious Ebola virus from the initial sample with 102 Ebola virus TCID50 mL–1 on day 1.
Figure 1.
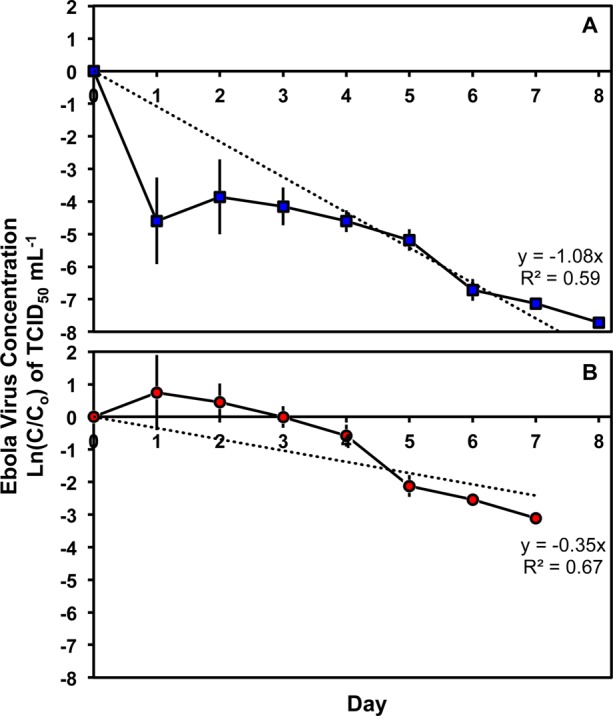
Persistence of an initial Ebola virus concentration of 106 TCID50 mL–1 in domestic wastewater (untreated sewage) (A) including the time zero time point and (B) excluding the time zero time point to mitigate potential aggregation effects. Linear trendlines are shown. Fit inactivation constants (k) were determined to be −1.08 when including time zero and −0.35 when excluding time zero. Error bars are ±1 standard deviation.
There was a rapid decrease (approximately 99%) in Ebola virus titer within the first day of the test. In addition to inactivation, viral particle aggregation or adsorption to wastewater particles may play a role in the apparent rapid viral decrease and enhanced viral persistence. In this case, aggregation would have two primary effects. First, aggregated particles would not be detected as multiple infectious units, resulting in an apparent rapid decrease. Second, it has been previously recognized that aggregation increases viral persistence and resistance to inactivation stressors.29,30 Organic matter in wastewater has previously been suggested to enhance viral aggregation.31 Similarly, viral association with particles has been recognized to provide protection from inactivation,32 including association of viral particles with wastewater solids.33 Mechanistically, particle association is believed to protect viral particles from inactivation by shielding them from environmental stressors and is dependent on the organism and particle type.32
Utilizing the current assay, it cannot be determined if the initial rapid decrease in viral titer was due to viral inactivation or aggregation. Aggregation would result in an apparent viral titer decrease as each viral aggregate would function as an infectious unit in the cell culture assay. To address this uncertainty, we plotted two inactivation curves, both including (Figure 1A) and excluding the measured time zero point (Figure 1B). A linear trendline, as has been previously suggested for viral34 and Ebola virus27 persistence, showed a lower fit (R2 = 0.59 including the time zero time point, and R2 = 0.67 excluding the time zero time point) than that previously observed for Ebola virus in deionized water (R2 > 0.91), but a fit better than that previously observed for Ebola virus in human blood (R2 < 0.29). The inactivation constant (k) was determined to be −1.08 when including the time zero time point and −0.35 when excluding the time zero time point. On the basis of the model fit, the T90 (time for 90% inactivation) would be 2.1 days including the time zero time point and 6.6 days excluding the time zero time point. The observed Ebola virus inactivation in wastewater was slower than that observed for deionized water, which required 1.8 days for 90% inactivation at 21 °C.27 The observed Ebola virus inactivation in wastewater was more rapid than that reported for human blood, which required 20 days for a 90% inactivation,27 and results are consistent with recent studies that identified viable Ebola virus to persist in infected macaque blood for >8 days.35 In general, Ebola virus was found to be less persistent in wastewater than model enteric viruses. While the T90 for Ebola virus in wastewater was found to be <1 day, the T90 for hepatitis A is greater than 17 days36 and the T90 for enteric adenovirus is 33 days;37 however, the T90 for poliovirus is 5 days,38 which is between the observed T90 values including or excluding the time zero time point. The results demonstrate a more rapid initial viral titer decrease but overall enhanced persistence of Ebola virus in wastewater compared to the proposed enveloped surrogate bacteriophage Phi6.39
Limitations
This study has two primary limitations that may alter the persistence of Ebola virus compared to what may be observed in the field. First, the tested wastewater was more dilute than would be expected in typical latrine waste.40,41 In general, interaction with constituents within the wastewater (e.g., ammonia) would be expected to contribute to more rapid inactivation of viruses;42 however, the true effect of these constituents on Ebola virus persistence is unknown. Second, the wastewater was frozen to minimize compositional changes and disinfected (γ-irradiation) prior to utilization to limit microbial activity resulting in false positive viral cell culture. Microbial activity within wastewater matrices would be expected to contribute to more rapid inactivation of infectious viral particles;36,42 however, the true effect of microbial activity on Ebola virus persistence is unknown. Microbial activity reduces viral persistence through both the production of metabolites detrimental to viral persistence and direct usage of the viral particles as a nutrient source.42 Additionally, the influence of other environmental characteristics (e.g., temperature, pH, and mixing) on Ebola virus persistence is unknown and may contribute to altered environmental behavior. As such, we believe these results to be an upper bound for Ebola virus persistence in wastewater matrices. Subsequently, we caution extrapolation of these results without a holistic assessment of all factors, including wastewater composition, dilution, and potential exposure routes.
Implications
The results of this study suggest a potential exposure route to infectious Ebola virus via wastewater; however, any assessment of potential exposure routes must consider the effects of wastewater composition, dilution of contaminated wastewater, and inactivation of Ebola virus during treatment and holding. Additionally, the possibility for Ebola virus transmission via wastewater and subsequent infection remains unknown. The WHO updated guidelines in January 2015 to recommend holding of latrine waste for 1 week prior to further handling or transport.20 The objective of this holding period is to allow Ebola virus die-off. On the basis of these results, it would be reasonable to approximate a three-log (i.e., 99.9%) removal of Ebola virus due to this holding period. The resulting risk would ultimately depend upon the initial Ebola virus concentration in wastewater, potential for exposure, and susceptibility to infection via wastewater exposure. The wastewater travel times for wastewater via a sewer system to a centralized sewage treatment works would typically be <1 day, depending on system dynamics.34 Further assessment is necessary to determine Ebola inactivation and dilution within this period and potential human exposure routes, including workers within the sewer system and Ebola virus persistence within wastewater sludges. The greatest exposure risk would be expected for persons in contact with contaminated wastewater prior to significant dilution, treatment, or holding.
These results demonstrate a persistence of Ebola virus in wastewater greater than what has previously been suggested and the potential of a wastewater exposure route to infectious Ebola virus. While Ebola virus was found to be generally less persistent than enteric viruses in wastewater, the identified survival period suggests value in a nuanced evaluation of wastewater exposure risks during an epidemic response. Specifically, these findings highlight the value of a precautionary approach to wastewater handling within an outbreak scenario, in response to both Ebola virus and other emerging viruses.
Acknowledgments
This study was supported by the Division of Intramural Research, National Institute of Allergy and Infectious Diseases, National Institutes of Health, and National Science Foundation Grants 1508415 (K.B. and L.W.C.) and 1507285 (C.N.H.). We acknowledge the anonymous wastewater sampling site for assistance.
Supporting Information Available
The Supporting Information is available free of charge on the ACS Publications website at DOI: 10.1021/acs.estlett.5b00193.
Recorded TCID50 values and standard deviations of Ebola virus spiked into sterilized domestic wastewater (Table S1) (PDF)
The authors declare no competing financial interest.
Supplementary Material
References
- CDC 2014 Ebola Outbreak in West Africa (http://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/index.html) (accessed July 9, 2015).
- Pourrut X.; Kumulungui B.; Wittmann T.; Moussavou G.; Délicat A.; Yaba P.; Nkoghe D.; Gonzalez J.-P.; Leroy E. M. The natural history of Ebola virus in Africa. Microbes Infect. 2005, 7 (7–8), 1005–1014. 10.1016/j.micinf.2005.04.006. [DOI] [PubMed] [Google Scholar]
- Team W. E. R. Ebola Virus Disease in West Africa — The First 9 Months of the Epidemic and Forward Projections. N. Engl. J. Med. 2014, 371 (16), 1481–1495. 10.1056/NEJMoa1411100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldmann H.; Geisbert T. W. Ebola haemorrhagic fever. Lancet 2011, 377 (9768), 849–862. 10.1016/S0140-6736(10)60667-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beer B.; Kurth R.; Bukreyev A. Characteristics of Filoviridae: Marburg and Ebola Viruses. Naturwissenschaften 1999, 86 (1), 8–17. 10.1007/s001140050562. [DOI] [PubMed] [Google Scholar]
- Kucharski A. J.; Edmunds W. J. Case fatality rate for Ebola virus disease in west Africa. Lancet 2014, 384 (9950), 1260. 10.1016/S0140-6736(14)61706-2. [DOI] [PubMed] [Google Scholar]
- Bausch D. G.; Towner J. S.; Dowell S. F.; Kaducu F.; Lukwiya M.; Sanchez A.; Nichol S. T.; Ksiazek T. G.; Rollin P. E. Assessment of the Risk of Ebola Virus Transmission from Bodily Fluids and Fomites. J. Infect. Dis. 2007, 196, S142–S147. 10.1086/520545. [DOI] [PubMed] [Google Scholar]
- Formenty P.; Leroy E. M.; Epelboin A.; Libama F.; Lenzi M.; Sudeck H.; Yaba P.; Allarangar Y.; Boumandouki P.; Nkounkou V. B.; Drosten C.; Grolla A.; Feldmann H.; Roth C. Detection of Ebola Virus in Oral Fluid Specimens during Outbreaks of Ebola Virus Hemorrhagic Fever in the Republic of Congo. Clin. Infect. Dis. 2006, 42 (11), 1521–1526. 10.1086/503836. [DOI] [PubMed] [Google Scholar]
- Rodriguez L. L.; De Roo A.; Guimard Y.; Trappier S. G.; Sanchez A.; Bressler D.; Williams A. J.; Rowe A. K.; Bertolli J.; Khan A. S.; Ksiazek T. G.; Peters C. J.; Nichol S. T. Persistence and Genetic Stability of Ebola Virus during the Outbreak in Kikwit, Democratic Republic of the Congo, 1995. J. Infect. Dis. 1999, 179 (Suppl. 1), S170–S176. 10.1086/514291. [DOI] [PubMed] [Google Scholar]
- Wolf T.; Kann G.; Becker S.; Stephan C.; Brodt H.-R.; de Leuw P.; Grünewald T.; Vogl T.; Kempf V. A. J.; Keppler O. T.; Zacharowski K. Severe Ebola virus disease with vascular leakage and multiorgan failure: treatment of a patient in intensive care. Lancet 2015, 385 (9976), 1428–1435. 10.1016/S0140-6736(14)62384-9. [DOI] [PubMed] [Google Scholar]
- Jelden K. C.; Gibbs S. G.; Smith P. W.; Schwedhelm M. M.; Iwen P. C.; Beam E. L.; Hayes A. K.; Marion N.; Kratochvil C. J.; Boulter K. C. Nebraska Biocontainment Unit patient discharge and environmental decontamination after Ebola care. Am. J. Infect. Control 2015, 43, 203–205. 10.1016/j.ajic.2014.12.005. [DOI] [PubMed] [Google Scholar]
- Lowe J. L.; Gibbs S. G.; Schwedhelm S.; Nguyen J.; Smith P. W. Nebraska Biocontainment Unit perspective on disposal of Ebola medical waste. Am. J. Infect. Control 2014, 42 (12), 1256–1257. 10.1016/j.ajic.2014.10.006. [DOI] [PubMed] [Google Scholar]
- Chertow D. S.; Kleine C.; Edwards J. K.; Scaini R.; Giuliani R.; Sprecher A. Ebola Virus Disease in West Africa — Clinical Manifestations and Management. N. Engl. J. Med. 2014, 371 (22), 2054–2057. 10.1056/NEJMp1413084. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Interim Infection Prevention and Control Guidance for Care of Patients with Suspected or Confirmed Filovirus Haemorrhagic Fever in Health-Care Settings, with Focus on Ebola; December 2014, 2014.
- Wigginton K. R.; Ye Y.; Ellenberg R. M. Emerging Investigators Series: The source and fate of pandemic viruses in the urban water cycle. Environmental Science: Water Research & Technology 2015, 10.1039/C5EW00125K. [DOI] [Google Scholar]
- Bibby K.; Casson L. W.; Stachler E.; Haas C. N. Ebola Virus Persistence in the Environment: State of the Knowledge and Research Needs. Environ. Sci. Technol. Lett. 2015, 2 (1), 2–6. 10.1021/ez5003715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lantagne D. S.; Hunter P. R. Comment on “Ebola Virus Persistence in the Environment: State of the Knowledge and Research Needs. Environ. Sci. Technol. Lett. 2015, 2 (2), 48–49. 10.1021/ez500410t. [DOI] [Google Scholar]
- Akyon B.; Stachler E.; Wei N.; Bibby K. Microbial Mats as a Biological Treatment Approach for Saline Wastewaters: The Case of Produced Water from Hydraulic Fracturing. Environ. Sci. Technol. 2015, 49 (10), 6172–6180. 10.1021/es505142t. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Ebola Virus Disease (EVD): Key questions and answers concerning water, sanitation and hygiene (accessed July 8, 2015).
- World Health Organization. Manual for the care and management of patients in Ebola Care Units/Community Care Centres Interim emergency guidance; 2015. [Google Scholar]
- CDC Interim Guidance for Managers and Workers Handling Untreated Sewage from Individuals with Ebola in the United States (http://www.cdc.gov/vhf/ebola/prevention/handling-sewage.html) (accessed July 8, 2015).
- Cook B. W.; Cutts T. A.; Nikiforuk A. M.; Poliquin P. G.; Court D.; Strong J. E.; Theriault S. Evaluating Environmental Persistence and Disinfection of the Ebola Virus Makona Variant. Viruses 2015, 7 (4), 1975–1986. 10.3390/v7041975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sozzi E.; Fabre K.; Fesselet J.-F.; Ebdon J. E.; Taylor H. Minimizing the Risk of Disease Transmission in Emergency Settings: Novel In Situ Physico-Chemical Disinfection of Pathogen-Laden Hospital Wastewaters. PLoS Neglected Trop. Dis. 2015, 9 (6), e0003776. 10.1371/journal.pntd.0003776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Judson S.; Prescott J.; Munster V. Understanding ebola virus transmission. Viruses 2015, 7 (2), 511–521. 10.3390/v7020511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roels T. H.; Bloom A. S.; Buffington J.; Muhungu G. L.; Mac Kenzie W. R.; Khan A. S.; Ndambi R.; Noah D. L.; Rolka H. R.; Peters C. J.; Ksiazek T. G. Ebola Hemorrhagic Fever, Kikwit, Democratic Republic of the Congo, 1995: Risk Factors for Patients without a Reported Exposure. J. Infect. Dis. 1999, 179 (Suppl. 1), S92–S97. 10.1086/514286. [DOI] [PubMed] [Google Scholar]
- Hoenen T.; Groseth A.; Feldmann F.; Marzi A.; Ebihara H.; Kobinger G.; Günther S.; Feldmann H. Complete Genome Sequences of Three Ebola Virus Isolates from the 2014 Outbreak in West Africa. Genome Announcements 2014, 2 (6), e01331-14. 10.1128/genomeA.01331-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer R.; Judson S.; Miazgowicz K.; Bushmaker T.; Prescott J.; Munster V. J. Ebola Virus Stability on Surfaces and in Fluids in Simulated Outbreak Environments. Emerging Infect. Dis. 2015, 21 (7), 1243. 10.3201/eid2107.150253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hierholzer J.; Killington R.. Virus isolation and quantitation. In Virology methods manual; Mahy B., Kangro H., Eds.; Academic Press: London, 1996; pp 25–46. [Google Scholar]
- Mattle M. J.; Crouzy B.; Brennecke M.; Wigginton K. R.; Perona P.; Kohn T. Impact of virus aggregation on inactivation by peracetic acid and implications for other disinfectants. Environ. Sci. Technol. 2011, 45 (18), 7710–7717. 10.1021/es201633s. [DOI] [PubMed] [Google Scholar]
- Berg G.; Chang S. L.; Harris E. K. Devitalization of microorganisms by iodine: I. Dynamics of the devitalization of enteroviruses by elemental iodine. Virology 1964, 22 (4), 469–481. 10.1016/0042-6822(64)90068-6. [DOI] [PubMed] [Google Scholar]
- Prado T.; Silva D. M.; Guilayn W. C.; Rose T. L.; Gaspar A. M. C.; Miagostovich M. P. Quantification and molecular characterization of enteric viruses detected in effluents from two hospital wastewater treatment plants. Water Res. 2011, 45 (3), 1287–1297. 10.1016/j.watres.2010.10.012. [DOI] [PubMed] [Google Scholar]
- Hoff J. C.; Akin E. W. Microbial resistance to disinfectants: mechanisms and significance. Environ. Health Perspect. 1986, 69, 7. 10.1289/ehp.86697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith E. M.; Gerba C. P.; Melnick J. L. Role of sediment in the persistence of enteroviruses in the estuarine environment. Appl. Environ. Microbiol. 1978, 35 (4), 685–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stallknecht D. E.; Shane S. M.; Kearney M. T.; Zwank P. J. Persistence of Avian Influenza Viruses in Water. Avian Dis. 1990, 34 (2), 406–411. 10.2307/1591428. [DOI] [PubMed] [Google Scholar]
- Prescott J.; Bushmaker T.; Fischer R.; Miazgowicz K.; Judson S.; Munster V. J. Postmortem stability of Ebola virus. Emerging Infect. Dis. 2015, 21 (5), 856. 10.3201/eid2105.150041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng M. Y.; Cliver D. O. Persistence of inoculated hepatitis A virus in mixed human and animal wastes. Appl. Environ. Microbiol. 1995, 61 (1), 87–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enriquez C. E.; Hurst C. J.; Gerba C. P. Survival of the enteric adenoviruses 40 and 41 in tap, sea, and waste water. Water Res. 1995, 29 (11), 2548–2553. 10.1016/0043-1354(95)00070-2. [DOI] [Google Scholar]
- Gundy P.; Gerba C.; Pepper I. Survival of Coronaviruses in Water and Wastewater. Food Environ. Virol. 2009, 1 (1), 10–14. 10.1007/s12560-008-9001-6. [DOI] [Google Scholar]
- Casanova L. M.; Weaver S. R. Inactivation of an Enveloped Surrogate Virus in Human Sewage. Environ. Sci. Technol. Lett. 2015, 2 (3), 76–78. 10.1021/acs.estlett.5b00029. [DOI] [Google Scholar]
- Foppen J. W. A. Impact of high-strength wastewater infiltration on groundwater quality and drinking water supply: the case of Sana’a, Yemen. J. Hydrol. 2002, 263 (1–4), 198–216. 10.1016/S0022-1694(02)00051-3. [DOI] [Google Scholar]
- Castro C. J.; Goodwill J. E.; Rogers B.; Henderson M.; Butler C. S. Deployment of the microbial fuel cell latrine in Ghana for decentralized sanitation. J. Water, Sanit. Hyg. Dev. 2014, 4 (4), 663–671. 10.2166/washdev.2014.020. [DOI] [Google Scholar]
- Sobsey M. D.; Meschke J. S. Virus survival in the environment with special attention to survival in sewage droplets and other environmental media of fecal or respiratory origin. Report for the World Health Organization, Geneva, Switzerland 2003, 70. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


