Diabetic foot ulcers have a biomechanical etiology related to triaxial plantar stresses (3DS) (1). Bergtholdt and Brand (2) suggested that the foot would heat up before breaking down, indicating that elevated 3DS in the diabetic foot would result in inflammation that could be monitored by thermography. The purpose of this study was to explore the hypothesized relationship between 3DS and plantar temperatures.
Twenty-eight individuals with diabetes, 14 with peripheral neuropathy (DN) and 14 without (DC), walked at self-selected speeds across a custom-built plate that quantified 3DS. After 10 min of acclimation, resting barefoot temperatures were recorded using a Fluke infrared thermal camera. Linear regressions were used to reveal associations between magnitudes of 3DS and resting temperatures. Associations between locations of peak 3DS and peak temperatures were also examined.
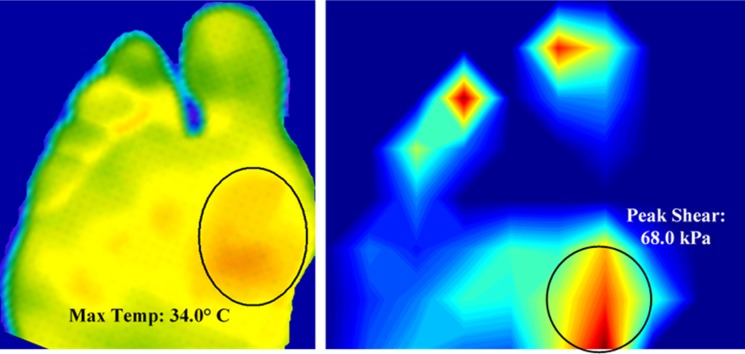
As assessed by linear regression, temperature was a statistically significant predictor of peak shear stress (PS) and shear-time integral magnitudes at the hallux. No significant association was found between peak pressure (PP) and temperature (P > 0.05). Linear regressions overall produced relatively lower R2 values (≤0.26). Peak temperature sites overlapped the site of PS in 71% of DC and 57% of DN participants (Fig. 1). PP location predicted the maximum temperature location in 86% of DC subjects and only 14% of DN subjects. Mean temperature for DN subjects (31.06°C ± 3.26) was significantly greater (P ≤ 0.001) than for DC subjects (28.82°C ± 3.85).
Figure 1.
Resting plantar temperature (left panel) and plantar PS (right panel) profiles of a representative DN subject. Note the match between the sites of peak temperature and PS at the first metatarsal head.
The results of this study, for the first time, revealed a moderate linear association between resting plantar temperature and PS magnitudes. Despite statistical significance, lower R2 values indicate that temperature is not an excellent predictor of PP and PS magnitudes. In comparison, PP and PS locations were predicted more accurately by temperature. We believe the relationship between 3DS and temperature might be better described by nonlinear techniques that account for the effects of fat pad damage, autonomic neuropathy, excessive or impaired sweating, and blood flow on plantar temperatures (3).
Yavuz et al. (4) demonstrated a plantar temperature increase of 5.3°C after 10 min of walking, which was strongly associated with frictional shear stresses. The thermal response of diabetic tissue to mechanical stresses may be categorized as acute and chronic. Acute response is observed right after load-bearing activity, mostly due to kinetic friction. Chronic thermal response results from prolonged exposure to repetitive stresses and is characterized by inflammation. The results of this and previous studies indicate that patients with diabetes experience both types of temperature increase.
Kokate et al. (5) demonstrated that temperature can determine whether tissue will break down when subjected to constant mechanical stress. The study reported moderate muscle damage at 35°C, while no damage was seen at 25°C under the same stress/strain conditions.
The damaging effects of 3DS in the diabetic foot may be due to not only strained cells and tissue but also an associated temperature increase. We believe that elevated plantar stresses warm up the diabetic foot, thereby reducing the tissue’s resistance to breakdown.
Exploring 3DS along with plantar temperatures may provide invaluable insight into ulceration etiology, which will lead to improved predictive tools and preventive measures.
Article Information
Acknowledgments. The authors thank Andrew Franklin, Rebecca McGaha, Joseph Stuto, Vinai Prakash, Garneisha Torrence, Jessica Rispoli, Sarah A. Richards, Kevin Garfield, Samuel T. Gray, Ashley E. Jensen, Nilin Rao, and Neha Delvadia of the Kent State University College of Podiatric Medicine.
Funding. This research was possible due to support from the National Institutes of Health (1R15DK082962).
None of the funding or supportive agencies were involved in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. M.Y. is the principal investigator and solely conceived and designed the study. M.Y. collected all data. R.W.B. and L.S.A. contributed to the analysis of data. A.G.G. contributed to the statistical analysis and interpretation of the data. A.G.G., A.G., M.F., L.L., B.L.D., and H.H. contributed to the review of the article and critically revised it for important intellectual content. M.Y. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. This study was presented in abstract form at the 7th World Congress of Biomechanics, Boston, MA, 6–11 June 2014, and at the 14th biennial Expert Scientific Meeting, Cambridge, MA, 2–6 July 2014.
References
- 1.Yavuz M. American Society of Biomechanics Clinical Biomechanics Award 2012: plantar shear stress distributions in diabetic patients with and without neuropathy. Clin Biomech (Bristol, Avon) 2014;29:223–229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bergtholdt HT, Brand PW. Thermography: an aid in the management of insensitive feet and stumps. Arch Phys Med Rehabil 1975;56:205–209 [PubMed] [Google Scholar]
- 3.Yavuz M, Ocak H, Hetherington VJ, Davis BL. Prediction of plantar shear stress distribution by artificial intelligence methods. J Biomech Eng 2009;131:091007. [DOI] [PubMed] [Google Scholar]
- 4.Yavuz M. Brem R, Davis BL, et al. . Temperature as a predictive tool for plantar triaxial loading. J Biomech 2014;47:3767–3770 [DOI] [PubMed] [Google Scholar]
- 5.Kokate JY, Leland KJ, Held AM, et al. . Temperature-modulated pressure ulcers: a porcine model. Arch Phys Med Rehabil 1995;76:666–673 [DOI] [PubMed] [Google Scholar]