The sensitivity and specificity of plantar pressure in identifying diabetic foot ulcers (DFUs) are relatively low, leading investigators to label peak pressure (PP) as a “poor” predictor (1). Moreover, pressure-reducing therapeutic footwear is only “meagerly” effective in preventing recurrent ulceration (2). These findings indicate that DFUs have a more complicated pathology. The purpose of this study was to investigate the clinical significance of plantar shear as it relates to ulcer locations using a custom-built stress plate (3).
Eight volunteers, each with one recently healed forefoot plantar DFU, walked at self-selected speeds across the custom-built plate, quantifying both PP and peak shear (PS).
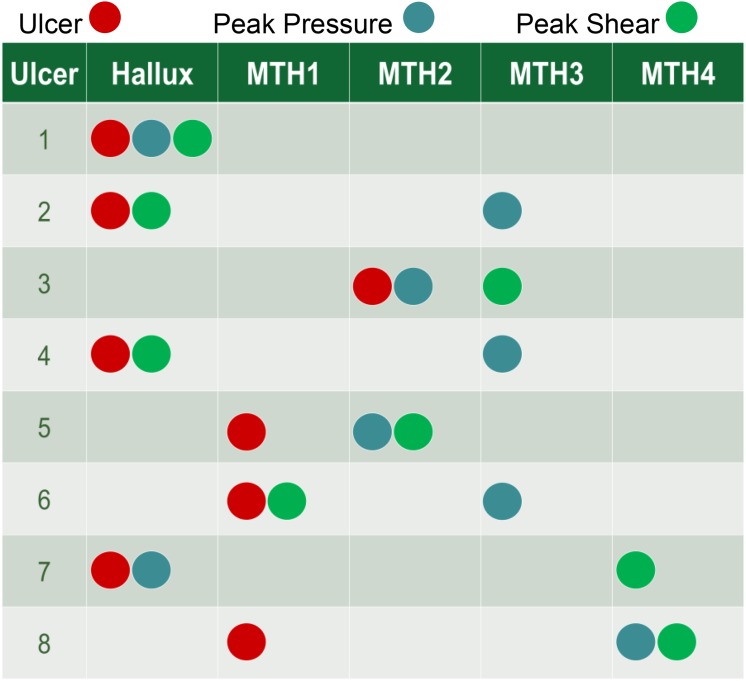
In five subjects (63%), PP and PS occurred at different plantar sites. Of eight ulcers, five did not develop at PP locations (Fig. 1). Two ulcers developed at PP-only locations, whereas three developed at PS-only sites. One ulcer location matched overlapping locations of PP and PS. Surprisingly, two ulcers occurred at neither PP nor PS locations.
Figure 1.
Relative locations of the healed ulcer, PP, and PS. MTH, metatarsal head.
Not only does pressure have low predictive value, but according to the only longitudinal study of its kind, only 38% of plantar ulcers develop at PP sites (4). Using the same custom-built device, we previously reported higher shear values in individuals with diabetes (3) and that PP and PS sites differ in 60% of diabetic neuropathic subjects. This study reports, for the first time in the literature, ulcers occurring at PS-only locations, not overlapping PP locations. Furthermore, more ulcers developed at PS locations as opposed to PP locations (50% vs. 38%).
Plantar shear may subject the tissue to fatigue failure by inducing forces in opposite directions during the same stance phase. Fatigue failure occurs due to low-magnitude cyclic loading—for example, breaking a paper clip by bending it back and forth. Moreover, early hyperkeratosis studies identified frictional shear as a major factor in callus formations, which are well-documented risk factors. Shear also contributes to both acute and chronic plantar temperature increases (5), which makes the tissue susceptible to breakdown.
We speculate that shear stresses lead to tissue damage and/or ulceration by:
causing fatigue failure
forming calluses
warming tissue and reducing its resistance to breakdown
Our results demonstrate that:
plantar shear has a clinically significant role in ulceration
utilizing both pressure and shear variables will be more effective in identifying/preventing ulceration
ulcers at different sites may have different pathologies
A better understanding of ulceration pathology will lead to more effective prevention methods, and, in this regard, pathological characteristics of combined pressure and shear should be further explored.
Many clinicians and researchers still oversimplify the pathology of ulceration, oftentimes referring to DFUs as “foot pressure ulcers.” DFUs and pressure ulcers (i.e., bedsores) are known to have different etiologies despite several similarities. In 2005, the National Pressure Ulcer Advisory Panel recognized shear as an underlying cause of pressure ulcers and started the “Shear Force Initiative” to foster research in this area. We hereby extend a call to the International Working Group on the Diabetic Foot and American Diabetes Association Interest Group on Foot Care to take similar action.
Article Information
Acknowledgments. The authors thank Andrew Franklin, Rebecca McGaha, Joseph Stuto, Vinai Prakash, Garneisha Torrence, Jessica Rispoli, Sarah A. Richards, Kevin Garfield, Samuel T. Gray, Ashley E. Jensen, Nilin Rao, and Neha Delvadia of the Kent State University College of Podiatric Medicine.
Funding. This research was possible due to support from the National Institutes of Health (1R15DK082962). None of the funding or supportive agencies were involved in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. M.Y. is the principal investigator and solely conceived and designed the study. M.Y. collected all data. H.M. and L.S.A. contributed to collection and analysis of data. A.G. and L.A.L. contributed to the review of the manuscript and critically revised it for important intellectual content. M.Y. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Parts of this study were presented in abstract form at the 7th World Congress of Biomechanics, Boston, MA, 6–11 July 2014, and at the 7th International Symposium on the Diabetic Foot, the Hague, the Netherlands, 20–23 May 2015. Portions of the data were presented at the 14th biennial Expert Scientific Meeting, Cambridge, MA, 2–6 July 2014.
References
- 1.Lavery LA, Armstrong DG, Wunderlich RP, Tredwell J, Boulton AJM. Predictive value of foot pressure assessment as part of a population-based diabetes disease management program. Diabetes Care 2003;26:1069–1073 [DOI] [PubMed] [Google Scholar]
- 2.Bus SA, Valk GD, van Deursen RW, et al. . The effectiveness of footwear and offloading interventions to prevent and heal foot ulcers and reduce plantar pressure in diabetes: a systematic review. Diabetes Metab Res Rev 2008;24(Suppl. 1):S162–S180 [DOI] [PubMed] [Google Scholar]
- 3.Yavuz M. American Society of Biomechanics Clinical Biomechanics Award 2012: plantar shear stress distributions in diabetic patients with and without neuropathy. Clin Biomech (Bristol, Avon) 2014;29:223–229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murray HJ, Young MJ, Hollis S, Boulton AJM. The association between callus formation, high pressures and neuropathy in diabetic foot ulceration. Diabet Med 1996;13:979–982 [DOI] [PubMed] [Google Scholar]
- 5.Yavuz M, Brem RW, Glaros AG, et al. . Association between plantar temperatures and triaxial stresses in individuals with diabetes. Diabetes Care 2015;38:e178–e179 [DOI] [PMC free article] [PubMed] [Google Scholar]