Abstract
A non-invasive and portable bioimpedance method and a device for detecting superior to inferior closure of the pharynx during swallowing have been developed. The 2-channel device measures electric impedance across the neck at two levels of the pharynx via injected currents at 40 and 70 kHz. The device has been trialled on both healthy and dysphagic subjects. Results from these trials revealed a relationship (r = 0.59) between the temporal separation of the second peaks in the bioimpedance waveforms and descending pressure sequence in the pharynx as measured by pharyngeal manometry. However, these features were only clearly visible in the bioimpedance waveforms for 64% of swallows. Further research is underway to improve the bioimpedance measurement reliability and validate waveform feature correlation to swallowing to maximise the device's efficacy in dysphagia rehabilitation.
Keywords: bioelectric phenomena, electric impedance measurement, biomedical measurement, medical disorders
Keywords: electrical bioimpedance measurement, dysphagia visualisation, portable bioimpedance method, pharynx closure, swallowing, 2-channel device, neck, injected currents, dysphagic subjects, bioimpedance waveforms, descending pressure sequence, pharyngeal manometry, bioimpedance measurement reliability, waveform feature correlation, dysphagia rehabilitation, frequency 40 kHz, frequency 70 kHz
1. Introduction
Biofeedback is well established as a valuable tool in rehabilitation and performance enhancement [1–3]. Here, biofeedback for the specific condition of dysphagia is explored. Dysphagia is the disturbance of the intake or transport of food from the mouth to the stomach [4] and can result from structural abnormalities in the throat and from various neurological disorders. Biofeedback has been found to be a useful approach for treatment of several debilitating dysphagic conditions [5].
Recent research has identified a specific pathophysiologic feature of dysphagia characterised by pharyngeal mis-sequencing [6]. This condition consists of an absence or abnormality of the pressure sequencing in the pharynx during a swallowing event. Simultaneous and even inverted pressure generation throughout the pharynx has been documented in multiple subjects.
Researchers at the University of Canterbury Swallowing Rehabilitation Research Laboratory (UCSL) have found that providing real-time visual biofeedback of pressure patterns in the pharynx to patients with this mis-sequencing impairment can help them retrain their pharyngeal sequencing to obtain a more normal swallowing pattern [6]. This biofeedback is provided through dual-channel pharyngeal manometry, which provides spatiotemporal information on the pharyngeal pressure waves to the patient during swallowing. There are several drawbacks to this system, however, including its invasive and uncomfortable nature, the limited portability of the device and the requirement for a trained specialist to oversee the process. These drawbacks prompted a study into alternate measurement techniques and, in particular, electrical bioimpedance.
Previous research has been undertaken into the use of electrical bioimpedance for the investigation of fundamentals of the swallowing process. Kusuhara et al. [7] designed and built an impedance pharyngography device to assess the swallowing function based on electrical impedance changes between two electrodes on the neck during swallows. Their device was able to produce real-time data relating to specific steps in the swallowing sequence.
Bioimpedance was chosen as the technique to be investigated over other possible approaches such as dual-axis accelerometry, fibre-optic endoscopic evaluation and muscle mapping [8–10]. This was because of the non-invasive nature of bioimpedance measurement, related research that had promising results [7], and the simplicity of the information required for effective biofeedback of pharyngeal mis-sequencing [6]. Endoscopic visualisation offered problems similar to the currently used manometry technique. In addition, the high number of muscles responsible for swallowing was deemed to make muscle mapping and accelerometry [8, 11] less suitable for use in this particular application of biofeedback-based rehabilitation. Further analysis was therefore conducted into bioimpedance to outline its basic theory as well as its potential application to the detection of pharyngeal sequencing appropriate for biofeedback-based rehabilitation in pharyngeal mis-sequencing dysphagia.
The underlying theory of operation for swallowing bioimpedance is that a change in impedance in the throat corresponds to a swallowing event. As a swallowing event occurs, the pharynx experiences a change in geometry because of the pressure created from contraction of the pharyngeal muscles. This change in geometry is associated with the air-filled pharyngeal lumen closing in a superior to inferior descending pattern, as shown in Fig. 1, resulting in a decrease in impedance between the electrodes. Results from a study performed by Hughes et al. [12] suggest that the exclusion of air from the larynx and pharynx is the major factor influencing the change in conductivity when a solution of low conductivity material is swallowed. The impedance change because of the geometry change in the pharynx was outlined as the most likely feature of bioimpedance to correspond to sequencing of the pharynx.
Figure 1.
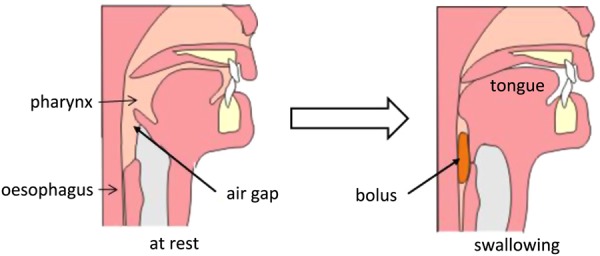
Visual representation of two instances in the swallowing sequence, where the air gap across the pharynx closes during a swallowing event [13]
The aim of this study was to extend the measurement of bioimpedance across the throat to two levels so as to derive two points of spatiotemporal reference of the pharynx, similar to that of two manometric channels, to allow determination of pharyngeal sequencing. This simple identification of basic pharyngeal sequencing has the potential to be used as a bio-feedback technique. Although measuring different aspects of the same physiologic mechanism as pharyngeal manometry, an association between the two signals was expected.
2. Design of the measurement system
The block diagram of one channel of the bioimpedance measurement device can be seen in Fig. 2, where two channels (each using four electrodes) are used in the device in order to emulate the manometry dual-channel system. The two channels inject currents of 40 and 70 kHz, respectively. These frequencies were chosen such that they were not integer multiples of each other to avoid harmonic interference and were chosen to be close to those used by Kusuhara et al. [7] in their investigation into bioimpedance characteristics of the throat. Kusuhara et al. chose 50 kHz in order to reduce the effect of surface conductance on the four-electrode system (observed at lower frequencies), while maintaining a lower level of base tissue conductance (which increases as frequency increases). The maximum current for each channel was chosen to be 0.5 mA (rms), so as to avoid discomfort experienced at currents of higher than 1 mA [5]. Potential sensory and motor implications of the stimulation current were not systematically explored in this project because of the low amplitude, high frequency and zero DC offset of the current used. In addition, other research has suggested that a minimum DC current of approximately 7 mA is required to stimulate movement in the pharyngeal area with the use of external electrodes [14].
Figure 2.
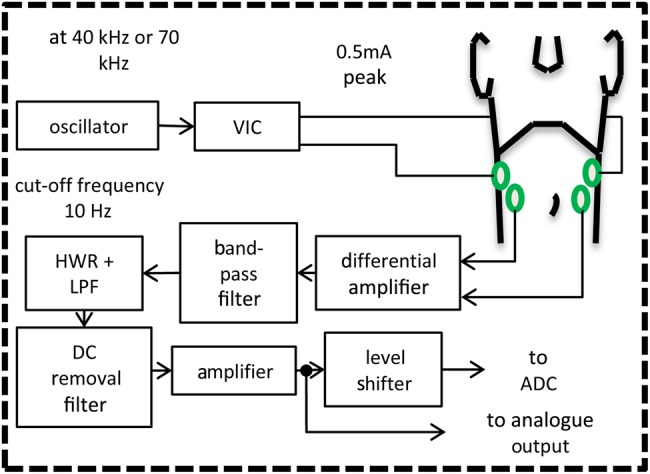
Block diagram of the modules in each channel of impedance measurement
VIC is the voltage-to-current converter, HWR is the half-wave rectifier, LPF is the low-pass filter and ADC stands for the analogue-to-digital converter
Each channel applies a constant-amplitude current across the throat to measure impedance. The oscillator module generates a constant-amplitude sinusoidal voltage waveform at the stated frequency. Following this, a voltage-to-current converter (VIC) creates the constant-amplitude AC-current waveform with the same frequency and phase as the oscillator. This waveform is produced across the neck, where a four electrode set-up is used to avoid surface/contact impedance change issues [15]. As a result of this constant amplitude electric current, impedance change in the neck is detected as a change in voltage, which is measured and amplified through a differential amplifier in combination with the voltage sensing electrodes. This signal is then band-pass filtered, centred on the channel's frequency to extract the desired signal, where each channel's input waveform experiences amplitude modulation by the changing impedance. This signal is then demodulated by the use of a half-wave rectifier and a low-pass filter with a −3 dB cut-off frequency of 10 Hz, as unpublished data from UCSL found that the maximum frequency of interest in manometry is ∼8 Hz. The initial at-rest value of the impedance is removed by the DC-removal filter to enable only the change in impedance to be measured, as the at-rest value of the impedance was deemed not required for the quantification of pharyngeal sequencing. This changing impedance signal is then amplified and can either be accessed via an analogue or a digital output (after being level-shifted and converted by the ADC). Custom software was written and used on a PC to communicate with the device digitally and display the output in real time to the user.
3. Electrode arrangement
The positioning of the eight electrodes (four for each channel) on the neck was an important factor for measuring impedance level changes. Positioning for the electrodes was considered to be optimal when the output of the two channels resembled the waveforms produced in pharyngeal manometry (the best comparative standard in this case), had the best absolute amplitude change during a swallowing event, and included two similar, but temporally separated, waveforms with clearly defined peaks. The protocol to determine the desired positioning included testing a grid of electrode placements covering the majority of each side of the neck. Swallows with and without a water bolus of 10 ml were conducted, where all swallows were completed with the mouth closed and with as little tongue movement as possible. The final position chosen was around the point of the pharynx, where a wafer was constructed containing electrodes with a 20 mm horizontal separation between the current generation and voltage detection electrodes for each channel. In turn, each channel is separated by a 40 mm vertical gap as shown in Fig. 3. The current-generating electrode pair for each channel was placed in the forward position on the throat. The electrodes were a dry, easily attachable and reusable type (EMG triode electrodes, Thought Technology Ltd., Toronto), which had been removed from their foam housing.
Figure 3.
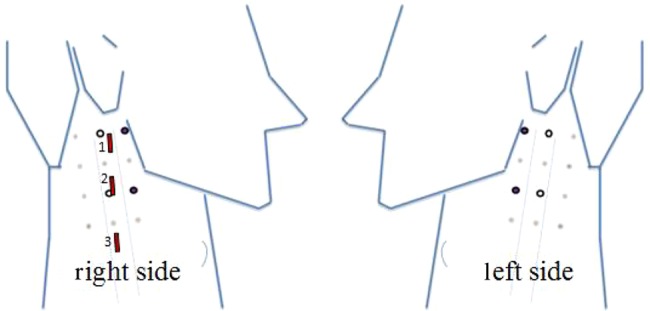
Chosen electrode positions:
Signal detection electrodes are circular electrodes with white centres (central) and current-generation circular electrodes have dark centres (closer to the jaw)
Relative nominal positioning of (internal) manomentry sensors are indicated by rectangular shapes 1, 2 and 3 on the right side image (corresponding to the sensor numbering allocated to the catheter used)
4. Manometric measurement
A 100-cm-long, round catheter, 2.1 mm in diameter (Model CTS3 + EMG, Gaeltec, Hackensack, NJ, USA) was used for manometric data collection. The catheter houses three solid-state, unidirectional, posteriorly oriented pressure sensors (2 × 5 mm), with 2 cm spacing between sensors 1 and 2, and 3 cm between sensors 2 and 3 (per standardised catheter recommendations from Salassa et al. [16]). Pressures were measured at the proximal-pharynx, distal-pharynx and upper oesophageal sphincter from sensors 1, 2 and 3, respectively (nominal positions of the sensors are shown in Fig. 3).
5. Experimental procedure
Testing was performed with swallows of both water bolus (wet) and saliva (dry) for each subject; the amount of water used was 10 ml for each bolus. Both normal and effortful swallowing techniques were used to determine the optimal testing conditions. The testing included using the device in a stand-alone manner as well as in combination with pharyngeal manometry for comparison. Three healthy subjects (2 male, 1 female; aged 20–24 years) and one subject with pharyngeal mis-sequencing following a brainstem stroke (male, age 51) were trialled.
6. Results
The output waveforms from the bioimpedance device were analysed to determine if any features could be related to the sequencing of pressure in the pharynx as measured by pharyngeal manometry. It was observed that a swallow would often produce three distinct features in the output waveforms of the bioimpedance device: two peaks and one trough (Fig. 4a). These features were not always visible but were the most repeatable of the observed features. The features were only seen in 64% of swallow measurements in healthy subjects when bioimpedance alone was being measured and this dropped further still to 24% of swallows when bioimpedance was measured concomitantly with manometry. The swallowing technique that best produced these waveforms was an effortful, wet swallow.
Figure 4.

Typical measured waveforms of healthy subject and dysphagic subject using the bioimpedance device in combination with pharyngeal manometry
Solid waveform for each figure is from the top position of measurement and the dashed is the bottom
Negative vertical impedance scale has been used in order to somewhat correspond to pressure increase in manometry measurements
a Bioimpedance waveforms for healthy subject
b Bioimpedance waveforms for dysphagic subject
c Pharyngeal manometry waveforms for healthy subject
d Pharyngeal manometry waveforms for dysphagic subject
To investigate the extent to which the bioimpedance features are related to pharyngeal sequencing, we used the bioimpedance device concomitantly with pharyngeal manometry (Fig. 4c). For comparison purposes, a typical dysphagic swallow bioimpedance waveform is shown in Fig. 4b and its equivalent manometry waveform in Fig. 4d. Linear regression analyses were undertaken between temporal separations of features in the impedance waveforms from both electrode positions (top and bottom) and the temporal separation between the peaks in manometric waveforms (Table 1). The measured waveform feature temporal resolution was better than ±10 ms. This regression identified reasonable correlations between impedance and manometric feature separations for bioimpedance troughs and second peaks, but not first peaks.
Table 1.
Correlations between temporal separation of features in bioimpedance waveforms and the peaks in manometry waveforms for a healthy subject and a dysphagic patient
| Subject | Swallows | Correlation (r) | ||
|---|---|---|---|---|
| First peaks | Troughs | Second peaks | ||
| healthy | 33 | 0.01 | 0.60 | 0.59 |
| dysphagic | 22 | 0.13 | 0.31 | 0.49 |
7. Discussion
We have demonstrated that continuous measures of bioimpedance at two levels across the throat can provide high-resolution temporal information corresponding to pharyngeal swallowing, which otherwise can only be obtained via invasive manometry. Notwithstanding, there is considerable room for the bioimpedance waveform measurements to be improved in terms of consistency. For example, the distinct features only occurred in 24% of trials when used concomitantly with manometry. Thus, a focus of our future work is aimed at identifying the source of this unreliability and variability.
Although a potential relationship has been found between the temporal separations of the features of the waveforms, it was expected that these features (specifically, the peaks) would line up with the features of manometry, but this was not the case. This may be because of the electrode positions relative to the pharyngeal anatomy being at different positions to the manometry pressure sensors. Another possible reason is that, in contrast to manometric pressure, bioimpedance is not a point measurement, with impedance changes reflecting transient structural changes over a much wider volume of the throat.
8. Conclusion
Two-channel electrical impedance measurement through the throat was investigated as an alternate method for the quantification of pharyngeal pressure generation. A custom-built multichannel measuring device was able to measure the spatiotemporal aspects of swallowing when trialled on several subjects. These measures are correlated with changes in peak separation seen in pharyngeal manometry. However, the device requires further refinement and validation before it can be reliably introduced into clinical and rehabilitative practice.
9 References
- 1.van Boxtel G.J.M., Gruzelier J.H.: ‘Neurofeedback: introduction to the special issue’, Biol. Psychol., 2014, 95, pp. 1–3 (doi: ) [DOI] [PubMed] [Google Scholar]
- 2.Basmajian J.V.: ‘Biofeedback-principles and practice for clinicians’ (Williams & Wilkins, Baltimore, MD, USA, 1979) [Google Scholar]
- 3.Edmonds W., Tenenbaum G.: ‘Case studies in applied psychophysiology: neurofeedback and biofeedback treatments for advances in human performance’ (Wiley, Chichester, UK, 2011) [Google Scholar]
- 4.Leopold N.A., Kagel M.C.: ‘Prepharyngeal dysphagia in Parkinson's disease’, Dysphagia, 1996, 11, (1), pp. 14–22, 1996 (doi: ) [DOI] [PubMed] [Google Scholar]
- 5.Langmore S.: ‘Endoscopic evaluation and treatment of swallowing disorders’ (Thieme, New York, NY, USA, 2001) [Google Scholar]
- 6.Huckabee M.: ‘The complexities of pharyngeal pathophysiology: Limitations in diagnosis lead to limitations in rehabilitation’, Int. J. Stroke, 2013, 8, (3), pp. 27–29 [Google Scholar]
- 7.Kusuhara T., Nakamura T., Shirakawa Y., Mori K., Naomoto Y., Yamamoto Y.: ‘Impedance pharyngography to assess swallowing function’, J. Int. Med. Res., 2004, 32, pp. 608–616 (doi: ) [DOI] [PubMed] [Google Scholar]
- 8.Lee J., Sejdić E., Steele C., Chau T.: ‘Effects of liquid stimuli on dual-axis swallowing accelerometry signals in a healthy population’, Biomed. Eng. Online, 2010, 9, (7), p. 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Langmore S.E., Schatz K., Olsen N.: ‘Fiberoptic endoscopic examination of swallowing safety: a new procedure’, Dysphagia, 1988, 2, (4), pp. 216–219 (doi: ) [DOI] [PubMed] [Google Scholar]
- 10.van Elswijk G., Kleine B.U., Overeem S., Eshuis B., Hekkert K.D., Stegeman D.F.: ‘Muscle imaging: Mapping responses to transcranial magnetic stimulation with high-density surface electromyography’, Cortex, 2008, 44, (5), pp. 609–616 (doi: ) [DOI] [PubMed] [Google Scholar]
- 11.Doeltgen S.H., Hofmayer A., Gumbley F., et al. : ‘Clinical measurement of pharyngeal surface electromyography: exploratory research’, Neurorehabil. Neural Repair, 2007, 21, (3), pp. 250–262 (doi: ) [DOI] [PubMed] [Google Scholar]
- 12.Hughes T.A.T., Liu P., Griffiths H., Lawries B.W., Wiles C.M.: ‘An analysis of studies comparing electrical impedance tomography with x-ray videofluoroscopy in the assessment of swallowing’, Physiol. Meas., 1994, 15, pp. 199–209 (doi: ) [DOI] [PubMed] [Google Scholar]
- 13.WikiBooks: ‘Medical Physiology Gastrointestinal Physiology Motility’, April 2013. Available at: http://www.en.wikibooks.org/wiki/MedicalPhysiology/GastrointestinalPhysiology/Motility
- 14.Ludlow C., Humbert I., Saxon K., Poletto C., Sonies B., Crujido L.: ‘Effects of surface electrical stimulation both at rest and during swallowing in chronic pharyngeal dysphagia’, Dysphagia, 2007, 22, (1), pp. 1–10 (doi: ) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baker L.: ‘Applications of the impedance technique to the respiratory system’, IEEE Eng. Med. Biol. Mag., 1989, 8, (1), pp. 50–52 (doi: ) [DOI] [PubMed] [Google Scholar]
- 16.Salassa J.R., DeVault K.R., McConnel F.M.: ‘Proposed catheter standards for pharyngeal manouorography (videomanometry)’, Dysphagia, 1998, 13, (2), pp. 105–110 (doi: ) [DOI] [PubMed] [Google Scholar]


