Abstract
Clinicians often use risk factor-based calculators to estimate an individual's risk of developing cardiovascular disease. Non-invasive cardiovascular imaging, particularly coronary artery calcium (CAC) scoring and coronary CT angiography (CTA), allows for direct visualization of coronary atherosclerosis. Among patients without prior coronary artery disease, studies examining CAC and coronary CTA have consistently shown that the presence, extent and severity of coronary atherosclerosis provide additional prognostic information for patients beyond risk factor-based scores alone. This review will highlight the basics of CAC scoring and coronary CTA and discuss their role in impacting patient prognosis and management.
Coronary artery disease (CAD) is the leading cause of morbidity and mortality in most industrialized nations throughout the world.1 Given the burden of coronary heart disease (CHD) to patients and society as a whole, much work has been carried out to determine patients' risk of adverse cardiovascular events. Such risk estimations are important as they often inform the need for preventive therapies such as lipid-lowering medications and aspirin. For instance, the Framingham risk score (FRS) uses age, gender, total cholesterol, high-density lipoprotein cholesterol, smoking status, systolic blood pressure and blood pressure treatment status to estimate 10-year risk of a myocardial infarction in patients without heart disease or diabetes.2 More recently, the 2013 American College of Cardiology/American Heart Association (ACC/AHA) guidelines on treatment of blood cholesterol identified four groups of individuals who may potentially benefit from statin therapy: patients with known atherosclerotic cardiovascular disease (ASCVD), low-density lipoprotein cholesterol ≥190 mg dl−1, diabetes and a ≥7.5% estimated 10-year risk of developing ASCVD determined by a risk calculator.3 However, these guidelines also suggest that in selected individuals not in the aforementioned groups, and for whom a decision to initiate statin therapy is otherwise unclear, additional risk factors such as a coronary artery calcium (CAC) score of ≥300 Agatsiton units or ≥75th percentile for age, sex and ethnicity can be considered.3 The European Society of Cardiology also included CAC in its 2012 European Guidelines on cardiovascular disease (CVD) prevention by stating that CAC should be considered for cardiovascular risk assessment in asymptomatic adults at moderate risk (Table 1).3–6
Table 1.
Recommendations for coronary artery calcium testing according to recent guidelines
| Guideline | Recommendations for CAC testing |
|---|---|
| 2013 American College of Cardiology/American Heart Association Guidelines3,4 | IIb indication; level of evidence B “if, after quantitative risk assessment, a risk-based treatment decision is uncertain, assessment (of CAC) may be considered to inform treatment decision making.”a |
| 2012 European Society of Cardiology Guidelines5 | IIa indication; level of evidence B “(CAC) should be considered for cardiovascular risk assessment in asymptomatic adults at moderate risk” |
| 2010 Appropriate Use Criteria for Cardiac CT6 | |
| Appropriate | Intermediate risk OR low risk and family history of premature CADb |
| Inappropriate | Low risk AND no family history of premature CADb |
| Uncertain | High risk |
CAD, coronary artery disease; ASCVD, atherosclerotic cardiovascular disease; LDL-C, low-density lipoprotein cholesterol.
After discussion with patient when decision to initiate statin therapy is unclear among selected individuals who are not in one of the four statin benefit groups, defined as those with (i) clinical atherosclerotic cardiovascular disease, (ii) primary elevation of LDL-C ≥190 mg dl−1, (iii) age of 40–75 years with diabetes and LDL-C of 70–189 mg dl−1 or (iv) age of 40–75 years without clinical ASCVD or diabetes and LDL-C of 70–189 mg dl−1 and estimated 10-year ASCVD risk ≥7.5%.
First-degree relative male <55 years of age or female <65 years of age.
The use of imaging to directly measure the burden of atherosclerosis can provide a more personalized risk assessment than using risk factor-based calculators. CAC scoring can be used to determine the actual presence and extent of calcified coronary artery plaque, whereas coronary CT angiography (CTA) visualizes calcified and non-calcified plaque, as well as the severity of luminal stenosis. While CAC testing is most commonly performed for risk assessment in asymptomatic individuals, coronary CTA is commonly performed in patients who have symptoms suggestive of underlying CHD. This review will discuss these two imaging modalities and how to use the results of these tests in patient management.
CORONARY ARTERY CALCIUM SCORING
Image acquisition
CAC scoring offers an inexpensive and reproducible technique to determine the actual presence and extent of calcified coronary artery plaque.7 It does not require contrast and can be performed on any patient who can hold their breath for 5–10 s.
Image acquisition guidelines for CAC testing have been previously published.8 No intravenous (i.v.) access is needed, and patients do not require any special preparation aside from practising how to hold their breath and remain still during the examination. While most centres do not administer any medications prior to CAC scanning, the use of beta blockers is optional and may have a small benefit in patients who have an elevated heart rate. Scans should be acquired using an axial mode with prospective electrocardiogram triggering during diastole. The scan settings include a tube voltage of 120 kV, while the tube current should be modified according to patient size in order to achieve a sufficient balance between radiation dose and image noise.
The amount of calcium is quantified using the Agatston score, which is based on multiplying each area of calcified plaque by the corresponding CT density.7
Prognostic data
CAC scoring has been shown to independently predict cardiovascular events as well as improve traditional risk prediction models.9,10 In particular, measurement of CAC improves both risk discrimination, as measured by the c-statistic, and reclassification of individuals into more accurate risk categories, as measured by net reclassification improvement.11–13 Several large observational studies have demonstrated that when added to standard risk prediction models, CAC has a significantly greater improvement in risk prediction than do other novel biomarkers or a combined biomarker panel.11–13 Importantly, the superior predictive capabilities of CAC scoring are owing to its ability to correctly reclassify patients into both high- and low-risk categories. In particular, individuals who do not have any coronary artery calcifications (CAC = 0) have an extremely low risk of CVD.14
Much attention has been focused on the utility of CAC scoring to enhance risk prediction for individuals at intermediate risk. However, it is important to note that CAC has significant prognostic value across a wide spectrum of age and risk factor profiles.15,16 Among individuals traditionally classified as low risk, either based on risk factor burden or calculated risk score, a high CAC score (≥100) is associated with an estimated 10-year all-CHD event rate of nearly 10%. By contrast, among individuals traditionally identified as high risk by risk factor burden or by the FRS, a CAC score of zero is associated with a remarkably low 10-year all-CHD event rate of roughly 3%. In fact, individuals with no risk factors and an elevated CAC score have nearly three times the event rate of those individuals with multiple risk factors and a CAC score of zero.15 Based on data from several large observational cohorts, CAC offers the potential for a refined and personalized risk estimate to help guide treatment decisions for primary prevention of CVD.17 Studies have also shown that patients with elevated CAC scores were more likely to be prescribed and adhere to lipid- and blood pressure-lowering therapies and aspirin, as well as improve their diets and level of physical activity.18–20
Limitations
Limitations and potential downsides of CAC include radiation exposure (although low, roughly 1 mSv, which is comparable to a mammogram) and incidental findings, such as pulmonary nodules, that may result in downstream tests, increased costs and patient anxiety.
CORONARY CT ANGIOGRAPHY
Image acquisition
Coronary CTA requires the administration of i.v. contrast to visualize non-calcified plaque and estimate the severity of luminal stenoses. It allows for high-resolution assessment of the presence, extent and severity of coronary plaque.21,22 Before performing a coronary CTA, contraindications, such as known iodine contrast allergy, inability to follow breath-hold instructions, pregnancy and renal insufficiency, should be reviewed. Additionally, potential patient-related technical issues that may interfere with the image quality, such as obesity and active cardiac arrhythmias, should be reviewed. To improve image quality, a slow and regular heart rate is preferred, usually <60 beats per minute. For individuals with faster heart rates, beta blockers can be prescribed. Nitrates may also be used to dilate the coronary arteries and improve image quality.23 Finally, electrocardiography leads should be positioned away from the field of view of the heart.
Current guidelines recommend the use of 64-detector or newer generation CT scanners.24 Since image quality depends on a number of parameters, the acquisition protocols should be individualized for each patient, aiming to achieve excellent image quality with the lowest radiation exposure possible. Whenever possible, low-dose protocols (such as axial acquisition using prospective electrocardiography triggering with low tube voltage and tube current) should be selected.25 During image acquisition, a high iodine concentration contrast media should be used with a high injection rate and optimal timing to ensure peak contrast opacification of the coronary arteries. Image acquisition is typically carried out during mid-diastole as this minimizes motion of the coronary arteries.
During image reconstruction, the thinnest slice thickness (typically, 0.50–0.75 mm) should be selected in order to optimize spatial resolution. The coronary CTA report should include a description of the amount and type of plaque, as well as the severity of luminal stenosis for each lesion.23
Prognostic data
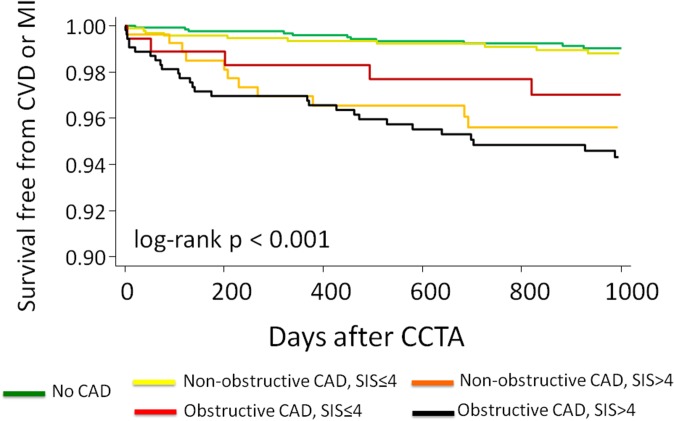
Studies have demonstrated that the presence and severity of CAD detected by coronary CTA adds prognostic value beyond traditional risk factors and symptoms.26,27 Currently, the greatest potential clinical value of coronary CTA is in the evaluation of low–intermediate patients with symptoms of possible coronary ischaemia.28 Among such patients, approximately one-third will be found to have no detectable CAD and thus excellent short- and long-term prognoses with a near zero coronary adverse event rate.27,29 Approximately, one-third of such patients will have non-obstructive CAD, a finding that does convey increased risk, particularly among patients with extensive coronary segment involvement.29–31 In fact, although the subgroup of patients with extensive non-obstructive CAD has not classically been a focus of CVD prevention or aggressive medical management, such patients have recently been demonstrated to have similar prognoses as those with obstructive CAD (Figures 1 and 2).30,31 Identification of this particular subgroup is a unique strength to an anatomic test, such as coronary CTA, since physiological stress tests such as single photon emission CT and stress echocardiography identify only flow-limiting CAD and do not characterize non-obstructive CAD burden.
Figure 1.
Rate of cardiovascular death or myocardial infarction according to the presence, severity and extent of coronary artery disease (CAD). There is a significant difference (p < 0.01) in rates for all comparisons except non-obstructive CAD with segment involvement score >4 and obstructive CAD with segment involvement score (SIS) ≤4. Reproduced from Bittencourt et al31 with permission from Lippincott Williams and Wilkins/Wolters Kluwer Health. pt, patient.
Figure 2.
Survival free from cardiovascular death or myocardial infarction according to the presence, severity and extent of coronary artery disease. CAD, coronary artery disease; CCTA, coronary CT angiography; CVD, cardiovascular death; MI, myocardial infarction; SIS, segment involvement score. Reproduced from Bittencourt et al31 with permission from Lippincott Williams and Wilkins/Wolters Kluwer Health.
Approximately, 15–20% of symptomatic patients without known prior disease undergoing coronary CTA may have potentially obstructive CAD (≥50% stenosis), a finding that is associated with a higher risk of cardiovascular events, especially when multivessel disease is present.32
The prognostic value of coronary CTA has been extensively proven among symptomatic patients in multiple settings including outpatient clinics and the emergency department.33 Indeed, coronary CTA has demonstrated value in females and males, as well as across multiple ethnicities.34,35 However, coronary CTA is not currently recommended for screening of asymptomatic patients owing to the low burden of CAD and overall benign prognosis among such patients.6 Special populations, such as select individuals with diabetes, continue to be evaluated for potential screening benefit in research studies, but such testing is not currently recommended for routine clinical use.36 In addition to evaluation of patients without known CAD, coronary CTA has demonstrated prognostic utility among patients with prior coronary artery bypass grafting.37,38
Limitations
Limitations of coronary CTA include decreased accuracy in patients with extensive calcified plaque or obesity (body mass index >40 kg m−2) and exposure to radiation and contrast. In addition, in comparison to functional tests such as myocardial perfusion imaging, the use of anatomical testing has the potential to lead to higher use of downstream invasive coronary angiography and coronary revascularizations.33 Finally, similar to CAC, coronary CTA has the potential to identify incidental findings that may require additional follow up and often contribute to patient anxiety. However, coronary CTA can also identify other clinically relevant findings to explain a patient's symptoms, such as aortic pathology, pulmonary disease or a hiatal hernia.
While a wide body of literature has established the prognostic value of CAD diagnosed by coronary CTA, an important limitation of this approach is the inability to determine the functional significance of anatomic lesions that are identified.39 While for many patients coronary anatomic information alone may be sufficient for diagnosis, risk assessment and patient management, concern exists regarding the potential for coronary CTA to trigger unnecessary downstream testing, coronary revascularization and increased cost relative to usual care.40,41 To address these issues, ongoing research efforts are examining ways to supplement conventional coronary CTA with additional CT-based physiological data, whether by combined rest and stress CT, mathematical modelling of cardiac physiology or inference of physiological flow from coronary transluminal contrast attenuation gradients.42–44 To date, most of these techniques remain investigational, and thus when lesions that are potentially flow limiting are identified among patients who are being considered for coronary revascularization, further testing is usually required in order to determine the presence and severity of ischaemia.
CONSIDERATIONS FOR PATIENT MANAGEMENT
In this section, we provide recommendations for patient management based on the results of CAC and coronary CTA testing. It is important to note that while CAC and coronary CTA findings can be useful in risk assessment, there is no randomized controlled trial data showing that treatment based on these tests can lead to improved patient outcomes. Such data are also lacking for other non-invasive imaging tests and for the various risk calculators that are used in clinical guidelines. It is unlikely that there will be any large randomized studies that compare CAC testing to traditional primary prevention algorithms that rely on the presence or absence of risk factors. While such a trial was previously proposed, it was not funded.45 Challenges related to the design of such a trial include the fact that a large number of patients would need to be randomized owing to the overall low event rates of most primary prevention cohorts and the larger number of patients who would be treated in the “non-CAC” arm owing to wider adoption of statin therapy by recent guidelines. While CAC testing has the potential of lowering cost by avoiding treatment in patients who have a CAC score of zero, further data are needed in this regard.
With regard to coronary CTA, the ongoing National Heart Lung and Blood Institute-sponsored Prospective Multicenter Imaging Study for Evaluation of Chest Pain trial is comparing functional and anatomic testing among stable patients with suspected CHD.46 This study may help determine whether treatment decisions based on coronary CTA, which will include initiation of preventive therapies in patients who are found to have non-obstructive plaque, could lead to improved patient outcomes.
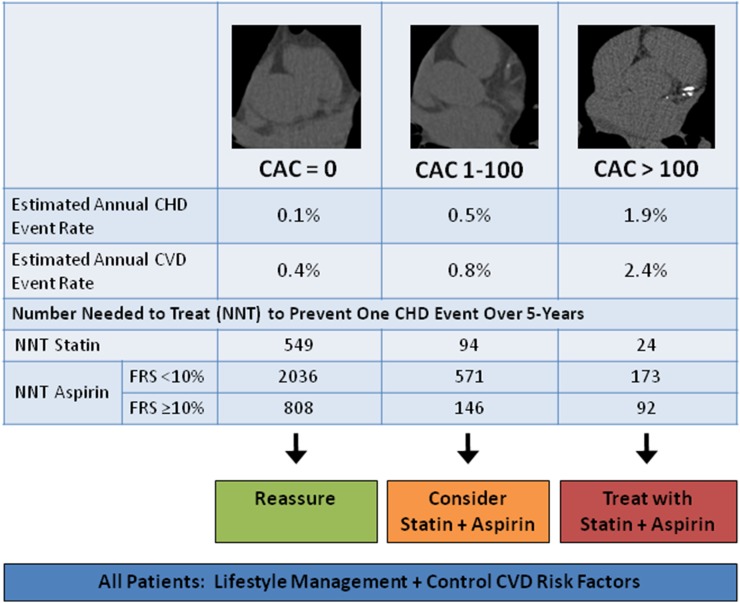
Coronary artery calcium: recommended management based on study findings
Several studies have explored future risk of ASCVD events stratified by CAC severity and have consistently demonstrated that patients with a CAC score of zero have excellent prognoses (Figure 3).47–49 Emphasis on lifestyle management (diet, exercise and smoking cessation) with treatment of modifiable ASCVD risk factors is recommended for these patients. Importantly, the number needed to treat (NNT) with aspirin and a statin in patients with a CAC of zero to prevent ASCVD is exceedingly high, and thus the small benefit of treating such individuals with pharmacotherapy may not justify the long-term risks and cost associated with their use. For example, it is estimated that aspirin therapy is associated with a number needed to harm approximately 442 patients to cause 1 major bleeding episode over a 5-year period compared with a NNT of 808 patients with a CAC of 0 and FRS >10% to prevent 1 CHD event in 5 years.49
Figure 3.
Coronary artery calcium (CAC) score prognosis and recommended treatment strategy. Note that the estimated number needed to harm with aspirin use is 442 patients to cause 1 major bleeding episode over a 5-year period. Thus, consider aspirin use in patients with CAC score of 1–100 when anticipated benefit exceeds risk [e.g., when Framingham risk score (FRS) ≥10%]. The amount of calcium is quantified using the Agatston score. CHD, coronary heart disease; CVD, cardiovascular disease.
When CAC is present, a CAC score of 1–100 is associated with an increased risk of future cardiac events (Figure 3). In these patients, statin and aspirin therapy should be considered, particularly in the presence of ASCVD risk factors with an intermediate-to-high FRS. Among patients with CAC >100, statin and aspirin therapy should be routinely recommended. In a study that explored whether a patient's CAC score could be used to define the target population to treat with a polypill (a combination of aspirin, a beta-blocker, an angiotensin-converting enzyme inhibitor and a statin) from participants in the Multi-Ethnic Study of Atherosclerosis, most events occurred in patients with a CAC score of >100.50 The NNT with a polypill over 5 years to prevent 1 CVD event ranged from 81 to 130 for patients with a CAC score of 0, 38–54 for patients with CAC scores between 1 and 100, and 18–20 for patients with a CAC score >100.50
Aside from preventive medical and lifestyle therapies, the vast majority of patients who have coronary artery calcifications do not require any further testing (e.g. stress testing), particularly as such testing or subsequent coronary revascularizations in asymptomatic individuals would not be expected to provide any benefit.51,52 In selected patients who have severe calcifications and have reduced exercise capacity (by history), or in whom it is uncertain if symptoms are present, functional testing with either exercise treadmill testing with or without myocardial perfusion imaging can be considered.
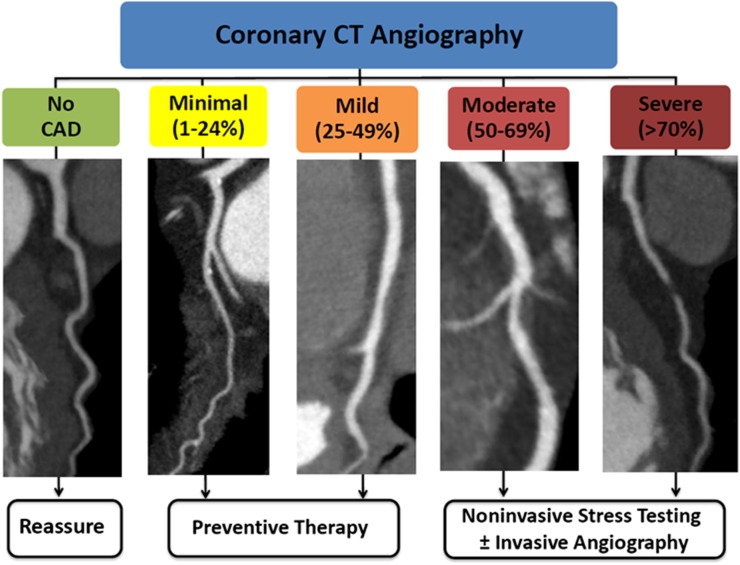
Coronary CT angiography: potential impact on downstream testing, management and outcomes
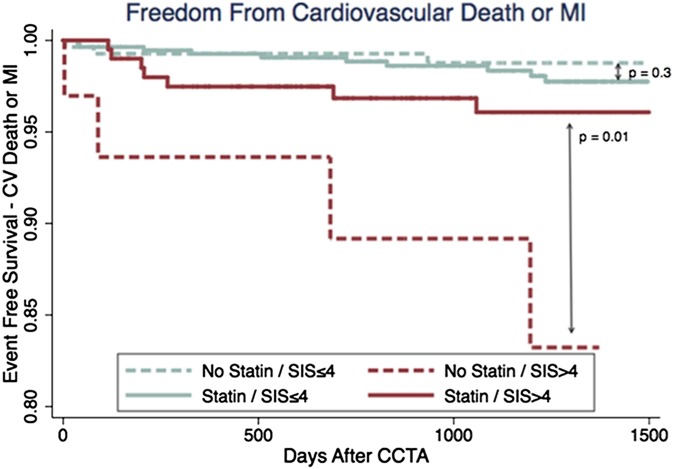
Multiple observational studies have shown that coronary CTA impacts downstream testing and patient management with the potential to guide preventive medical therapies and improve CAD risk factor control.32,53–57 Among non-invasive cardiac tests, coronary CTA may offer a particular advantage in its ability to visualize non-obstructive CAD, and therefore identify patients who may benefit from preventive CAD therapies when functional testing would have otherwise been normal. Hulten et al32 followed 2839 patients without prior CAD who were referred for coronary CTA and found that among patients with non-obstructive CAD that involved at least 4 segments, treatment with statin therapy was associated with improved event-free survival over a mean follow up of 3 years (p < 0.01) (Figure 4).58 While prospective studies are needed to examine the potential impact of coronary CTA on outcomes, these data provide support to the hypothesis that coronary CTA-based patient management may lead to improved patient outcomes.
Figure 4.
coronary artery disease (CAD) severity identified by coronary CT angiography and recommended management. Patients with a normal coronary CT angiography can be safely reassured. Follow-up for preventive therapy is recommended for non-obstructive (<50%) CAD. For obstructive CAD (≥50% stenosis), further testing is recommended to guide management. Adapted from Cheezum et al58 with permission from Informa Healthcare.
When deciding on patient medical management following coronary CTA, the decision to treat patients with pharmacotherapy should be based on the prognostic value of coronary CTA findings while considering guideline recommendations for the primary and secondary prevention of ASCVD.4,59 The 2013 ACC/AHA guidelines recommend primary prevention statin therapy when the 10-year risk of ASCVD is ≥7.5% (moderate- to high-intensity statin; Class I indication) or 5.0–7.5% (moderate intensity statin; Class IIa indication).4 While no recommendations were made in these guidelines regarding the management of coronary CTA findings, a reasonable approach is to extrapolate data relating CAD burden to the risk of future ASCVD events.
Coronary CT angiography: recommended management based on test findings
Normal
Among patients with stable and acute chest pain, studies have consistently shown that a normal coronary CTA reliably excludes obstructive CAD and is associated with a very low rate of downstream cardiac events. Thus, a patient with no plaque or stenosis on coronary CTA requires no further evaluation. This result provides an opportunity to reassure patients regarding the absence of CAD, while focusing on risk factor control and lifestyle therapies.32
Non-obstructive coronary artery disease
Management of non-obstructive CAD should be individualized to the patient and based on integrating clinical ASCVD risk factors as well as the extent of plaque. Statin use is recommended when multiple coronary segments have plaque (Figure 5).32 Additionally, multiple high-risk plaque features have been shown to be associated with a higher risk of future acute coronary syndrome (e.g. positive remodelling, low-attenuation plaque and spotty calcification).32,60 Although no data exist to suggest that targeted management of high-risk plaque features results in improved clinical outcomes, moderate- to high-intensity statin therapy remains reasonable in this setting and has been shown by serial coronary CTA to improve non-calcified plaque, low-attenuation plaque and necrotic core volumes.61 Additionally, very high-intensity statin therapy resulted in significant regression of atherosclerosis by several intravascular ultrasound (IVUS) parameters, including change in percent atheroma volume (considered the most rigorous IVUS measure), in the ASTEROID trial.62 Patients with non-obstructive CAD should not be falsely reassured regarding the absence of significant luminal stenoses, as a substantial proportion of myocardial infarctions occurs in patients with non-obstructive plaque, and follow-up counselling with attention to ASCVD risk factor control is required for many of these patients.
Figure 5.
Event-free survival according to the presence or absence of statin therapy post-coronary CT angiography among patients with non-obstructive coronary artery disease, stratified by extent of disease according to segment involvement score (SIS). CCTA, coronary CT angiography; CV, cardiovascular; MI, myocardial infarction. Reproduced from Hulten et al32 with permission from Wolters Kluwer Health.
Obstructive coronary artery disease
In patients with potentially obstructive CAD (stenosis ≥50%), further testing is generally recommended to determine the haemodynamic significance of these lesions. Functional testing, such as non-invasive stress imaging or invasive fractional flow reserve, is particularly important to minimize unnecessary revascularization, as approximately half of patients with >50% stenosis on coronary CTA will have no resultant ischaemia.39 To guide testing after coronary CTA, appropriate use criteria for the detection and risk of stable ischaemic heart disease and diagnostic angiography are available.63
Among patients with obstructive CAD, preventative therapies, including aspirin and statin therapy and management of ASCVD risk factors, are routinely recommended. Follow-up is critical to monitor adherence and response to therapy in these patients, as the prevalence of undertreatment remains high even among patients with high-risk imaging abnormalities. Among 1703 patients undergoing myocardial perfusion imaging or coronary CTA in the Study of Myocardial Perfusion and Coronary Anatomy Imaging Roles in CAD study, for example, the majority of patients with moderate-to-severe imaging abnormalities lacked one or more standard therapies (aspirin, statin and beta-blocker) 90-days post-imaging.64
CONCLUSION
While risk factors can be used to identify individuals with possible CAD, CAC scoring and coronary CTA detect the actual presence of disease. In asymptomatic individuals without known CAD, knowledge regarding the presence or absence of CAC can lead to a more precise estimation of risk. Such information has the potential to match more aggressive therapies for those at higher risk while avoiding pharmacotherapy in those with no CAC. However, ongoing debate regarding incorporation of CAC among risk-based primary prevention strategies has limited the widespread use of this test. Among symptomatic patients, the results of coronary CTA can provide important prognostic information regarding a patient's future risk of major adverse cardiac events, and thus help guide the initiation or intensification of preventive therapies. While a strength of coronary CTA is its ability to identify the full spectrum of CAD, including non-obstructive plaque, in order to limit coronary revascularizations to patients who are most likely to benefit from it, functional testing may be required to determine the haemodynamic significance of lesions that are potentially flow limiting.
REFERENCES
- 1.Yusuf S, Reddy S, Ounpuu S, Anand S. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation 2001; 104: 2746–53. [DOI] [PubMed] [Google Scholar]
- 2.National Cholesterol Education Program (NCEP) Expert Panel on Detection Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation 2002; 106: 3143–421. [PubMed] [Google Scholar]
- 3.Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. ; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation 2014; 129(Suppl. 2): S1–45. doi: 10.1161/01.cir.0000437738.63853.7a [DOI] [PubMed] [Google Scholar]
- 4.Goff DC, Jr, Lloyd-Jones DM, Bennett G, Coady S, D'Agostino RB, Gibbons R, et al. ; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation 2014; 129(Suppl. 2): S49–73. doi: 10.1161/01.cir.0000437741.48606.98 [DOI] [PubMed] [Google Scholar]
- 5.Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren M, et al. ; European Association for Cardiovascular Prevention & Rehabilitation (EACPR); ESC Committee for Practice Guidelines (CPG). European guidelines on cardiovascular disease prevention in clinical practice (version 2012). The fifth joint task force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts). Eur Heart J 2012; 33: 1635–701. doi: 10.1093/eurheartj/ehs092 [DOI] [PubMed] [Google Scholar]
- 6.Taylor AJ, Cerqueira M, Hodgson JM, Mark D, Min J, O'Gara P, et al. ; American College of Cardiology Foundation Appropriate Use Criteria Task Force Society of Cardiovascular Computed Tomography American College of Radiology American Heart Association American Society of Echocardiography American Society of Nuclear Cardiology North American Society for Cardiovascular Imaging Society for Cardiovascular Angiography and Interventions; Society for Cardiovascular Magnetic Resonance. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography. A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. Circulation 2010; 122: e525–55. doi: 10.1161/CIR.0b013e3181fcae66 [DOI] [PubMed] [Google Scholar]
- 7.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990; 15: 827–32. [DOI] [PubMed] [Google Scholar]
- 8.Voros S, Rivera JJ, Berman DS, Blankstein R, Budoff MJ, Cury RC, et al. ; Society for Atherosclerosis Imaging and Prevention Tomographic Imaging and Prevention Councils Society of Cardiovascular Computed Tomography. Guideline for minimizing radiation exposure during acquisition of coronary artery calcium scans with the use of multidetector computed tomography: a report by the society for atherosclerosis imaging and prevention tomographic imaging and prevention councils in collaboration with the society of cardiovascular computed tomography. J Cardiovasc Comput Tomogr 2011; 5: 75–83. doi: 10.1016/j.jcct.2011.01.003 [DOI] [PubMed] [Google Scholar]
- 9.Greenland P, LaBree L, Azen SP, Doherty TM, Detrano RC. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA 2004; 291: 210–15. [DOI] [PubMed] [Google Scholar]
- 10.Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med 2008; 358: 1336–45. doi: 10.1056/NEJMoa072100 [DOI] [PubMed] [Google Scholar]
- 11.Yeboah J, McClelland RL, Polonsky TS, Burke GL, Sibley CT, O'Leary D, et al. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individuals. JAMA 2012; 308: 788–95. doi: 10.1001/jama.2012.9624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kavousi M, Elias-Smale S, Rutten JH, Leening MJ, Vliegenthart R, Verwoert GC, et al. Evaluation of newer risk markers for coronary heart disease risk classification: a cohort study. Ann Intern Med 2012; 156: 438–44. doi: 10.7326/0003-4819-156-6-201203200-00006 [DOI] [PubMed] [Google Scholar]
- 13.Rana JS, Gransar H, Wong ND, Shaw L, Pencina M, Nasir K, et al. Comparative value of coronary artery calcium and multiple blood biomarkers for prognostication of cardiovascular events. Am J Cardiol 2012; 109: 1449–53. doi: 10.1016/j.amjcard.2012.01.358 [DOI] [PubMed] [Google Scholar]
- 14.Sarwar A, Shaw LJ, Shapiro MD, Blankstein R, Hoffmann U, Cury RC, et al. Diagnostic and prognostic value of absence of coronary artery calcification. JACC Cardiovasc Imaging 2009; 2: 675–88. doi: 10.1016/j.jcmg.2008.12.031 [DOI] [PubMed] [Google Scholar]
- 15.Silverman MG, Blaha MJ, Krumholz HM, Budoff MJ, Blankstein R, Sibley CT, et al. Impact of coronary artery calcium on coronary heart disease events in individuals at the extremes of traditional risk factor burden: the multi-ethnic study of atherosclerosis. Eur Heart J 2013; 35: 2232–41. doi: 10.1093/eurheartj/eht508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tota-Maharaj R, Blaha MJ, McEvoy JW, Blumenthal RS, Muse ED, Budoff MJ, et al. Coronary artery calcium for the prediction of mortality in young adults <45 years old and elderly adults >75 years old. Eur Heart J 2012; 33: 2955–62. doi: 10.1093/eurheartj/ehs230 [DOI] [PubMed] [Google Scholar]
- 17.Blaha MJ, Silverman MG, Budoff MJ. Is there a role for coronary artery calcium scoring for management of asymptomatic patients at risk for coronary artery disease?: clinical risk scores are not sufficient to define primary prevention treatment strategies among asymptomatic patients. Circ Cardiovasc Imaging 2014; 7: 398–408. doi: 10.1161/CIRCIMAGING.113.000341 [DOI] [PubMed] [Google Scholar]
- 18.Nasir K, McClelland RL, Blumenthal RS, Goff DC, Jr, Hoffmann U, Psaty BM, et al. Coronary artery calcium in relation to initiation and continuation of cardiovascular preventive medications: the multi-ethnic study of atherosclerosis (MESA). Circ Cardiovasc Qual Outcomes 2010; 3: 228–35. doi: 10.1161/CIRCOUTCOMES.109.893396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Orakzai RH, Nasir K, Orakzai SH, Kalia N, Gopal A, Musunuru K, et al. Effect of patient visualization of coronary calcium by electron beam computed tomography on changes in beneficial lifestyle behaviors. Am J Cardiol 2008; 101: 999–1002. doi: 10.1016/j.amjcard.2007.11.059 [DOI] [PubMed] [Google Scholar]
- 20.Rozanski A, Gransar H, Shaw LJ, Kim J, Miranda-Peats L, Wong ND, et al. Impact of coronary artery calcium scanning on coronary risk factors and downstream testing the EISNER (early identification of subclinical atherosclerosis by noninvasive imaging research) prospective randomized trial. J Am Coll Cardiol 2011; 57: 1622–32. doi: 10.1016/j.jacc.2011.01.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miller JM, Rochitte CE, Dewey M, Arbab-Zadeh A, Niinuma H, Gottlieb I, et al. Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med 2008; 359: 2324–36. doi: 10.1056/NEJMoa0806576 [DOI] [PubMed] [Google Scholar]
- 22.Budoff MJ, Dowe D, Jollis JG, Gitter M, Sutherland J, Halamert E, et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (assessment by coronary computed tomographic angiography of individuals undergoing invasive coronary angiography) trial. J Am Coll Cardiol 2008; 52: 1724–32. doi: 10.1016/j.jacc.2008.07.031 [DOI] [PubMed] [Google Scholar]
- 23.Abbara S, Arbab-Zadeh A, Callister TQ, Desai MY, Mamuya W, Thomson L, et al. SCCT guidelines for performance of coronary computed tomographic angiography: a report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr 2009; 3: 190–204. doi: 10.1016/j.jcct.2009.03.004 [DOI] [PubMed] [Google Scholar]
- 24.American College of Cardiology Foundation Task Force on Expert Consensus Documents, Mark DB, Berman DS, Budoff MJ, Carr JJ, Gerber TC, Hecht HS, et al. ACCF/ACR/AHA/NASCI/SAIP/SCAI/SCCT 2010 expert consensus document on coronary computed tomographic angiography: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. J Am Coll Cardiol 2010; 55: 2663–99. doi: 10.1016/j.jacc.2009.11.013 [DOI] [PubMed] [Google Scholar]
- 25.Halliburton SS, Abbara S, Chen MY, Gentry R, Mahesh M, Raff GL, et al. ; Society of Cardiovascular Computed Tomography. SCCT guidelines on radiation dose and dose-optimization strategies in cardiovascular CT. J Cardiovasc Comput Tomogr 2011; 5: 198–224. doi: 10.1016/j.jcct.2011.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chow BJ, Wells GA, Chen L, Yam Y, Galiwango P, Abraham A, et al. Prognostic value of 64-slice cardiac computed tomography severity of coronary artery disease, coronary atherosclerosis, and left ventricular ejection fraction. J Am Coll Cardiol 2010; 55: 1017–28. doi: 10.1016/j.jacc.2009.10.039 [DOI] [PubMed] [Google Scholar]
- 27.Andreini D, Pontone G, Mushtaq S, Bartorelli AL, Bertella E, Antonioli L, et al. A long-term prognostic value of coronary CT angiography in suspected coronary artery disease. JACC Cardiovasc Imaging 2012; 5: 690–701. doi: 10.1016/j.jcmg.2012.03.009 [DOI] [PubMed] [Google Scholar]
- 28.Moshage WE, Achenbach S, Seese B, Bachmann K, Kirchgeorg M. Coronary artery stenoses: three-dimensional imaging with electrocardiographically triggered, contrast agent-enhanced, electron-beam CT. Radiology 1995; 196: 707–14. [DOI] [PubMed] [Google Scholar]
- 29.Hulten EA, Carbonaro S, Petrillo SP, Mitchell JD, Villines TC. Prognostic value of cardiac computed tomography angiography: a systematic review and meta-analysis. J Am Coll Cardiol 2011; 57: 1237–47. doi: 10.1016/j.jacc.2010.10.011 [DOI] [PubMed] [Google Scholar]
- 30.Lin FY, Shaw LJ, Dunning AM, Labounty TM, Choi JH, Weinsaft JW, et al. Mortality risk in symptomatic patients with nonobstructive coronary artery disease: a prospective 2-center study of 2,583 patients undergoing 64-detector row coronary computed tomographic angiography. J Am Coll Cardiol 2011; 58: 510–19. doi: 10.1016/j.jacc.2010.11.078 [DOI] [PubMed] [Google Scholar]
- 31.Bittencourt MS, Hulten E, Ghoshhajra B, O'Leary D, Christman MP, Montana P, et al. Prognostic value of nonobstructive and obstructive coronary artery disease detected by coronary computed tomography angiography to identify cardiovascular events. Circ Cardiovasc Imaging 2014; 7: 282–91. doi: 10.1161/CIRCIMAGING.113.001047 [DOI] [PubMed] [Google Scholar]
- 32.Hulten E, Bittencourt MS, Singh A, O'Leary D, Christman MP, Osmani W, et al. Coronary artery disease detected by coronary CT angiography is associated with intensification of preventive medical therapy and lower LDL cholesterol. Circ Cardiovasc Imaging 2014; 7: 629–38. doi: 10.1161/CIRCIMAGING.113.001564 [DOI] [PubMed] [Google Scholar]
- 33.Hulten E, Pickett C, Bittencourt MS, Villines TC, Petrillo S, Di Carli MF, et al. Outcomes after coronary computed tomography angiography in the emergency department: a systematic review and meta-analysis of randomized, controlled trials. J Am Coll Cardiol 2013; 61: 880–92. doi: 10.1016/j.jacc.2012.11.061 [DOI] [PubMed] [Google Scholar]
- 34.Min JK, Dunning A, Lin FY, Achenbach S, Al-Mallah M, Budoff MJ, et al. Age- and sex-related differences in all-cause mortality risk based on coronary computed tomography angiography findings results from the International Multicenter CONFIRM (coronary CT angiography evaluation for clinical outcomes: an international multicenter registry) of 23,854 patients without known coronary artery disease. J Am Coll Cardiol 2011; 58: 849–60. doi: 10.1016/j.jacc.2011.02.074 [DOI] [PubMed] [Google Scholar]
- 35.Hulten E, Villines TC, Cheezum MK, Berman DS, Dunning A, Achenbach S, et al. Usefulness of coronary computed tomography angiography to predict mortality and myocardial infarction among Caucasian, African and East Asian ethnicities [from the CONFIRM (coronary CT angiography evaluation for clinical outcomes: an international multicenter) registry]. Am J Cardiol 2013; 111: 479–85. doi: 10.1016/j.amjcard.2012.10.028 [DOI] [PubMed] [Google Scholar]
- 36.Hulten E, Bittencourt MS, O'Leary D, Shah R, Ghoshhajra B, Christman MP, et al. Cardiometabolic risk is associated with atherosclerotic burden and prognosis: results from the partners coronary computed tomography angiography registry. Diabetes Care 2014; 37: 555–64. doi: 10.2337/dc13-1431 [DOI] [PubMed] [Google Scholar]
- 37.Mushtaq S, Andreini D, Pontone G, Bertella E, Bartorelli AL, Conte E, et al. Prognostic value of coronary CTA in coronary bypass patients: a long-term follow-up study. JACC Cardiovasc Imaging 2014; 7: 580–9. doi: 10.1016/j.jcmg.2014.04.003 [DOI] [PubMed] [Google Scholar]
- 38.Chow BJ, Ahmed O, Small G, Alghamdi AA, Yam Y, Chen L, et al. Prognostic value of CT angiography in coronary bypass patients. JACC Cardiovasc Imaging 2011; 4: 496–502. doi: 10.1016/j.jcmg.2011.01.015 [DOI] [PubMed] [Google Scholar]
- 39.Blankstein R, Di Carli MF. Integration of coronary anatomy and myocardial perfusion imaging. Nat Rev Cardiol 2010; 7: 226–36. doi: 10.1038/nrcardio.2010.15 [DOI] [PubMed] [Google Scholar]
- 40.Shreibati JB, Baker LC, Hlatky MA. Association of coronary CT angiography or stress testing with subsequent utilization and spending among Medicare beneficiaries. JAMA 2011; 306: 2128–36. doi: 10.1001/jama.2011.1652 [DOI] [PubMed] [Google Scholar]
- 41.Hulten E, Goehler A, Bittencourt MS, Bamberg F, Schlett CL, Truong QA, et al. Cost and resource utilization associated with use of computed tomography to evaluate chest pain in the emergency department: the rule out myocardial infarction using computer assisted tomography (ROMICAT) study. Circ Cardiovasc Qual Outcomes 2013; 6: 514–24. doi: 10.1161/CIRCOUTCOMES.113.000244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hulten EA, Bittencourt MS, Ghoshhajra B, Blankstein R. Stress CT perfusion: coupling coronary anatomy with physiology. J Nucl Cardiol 2012; 19: 588–600. doi: 10.1007/s12350-012-9546-5 [DOI] [PubMed] [Google Scholar]
- 43.Min JK, Leipsic J, Pencina MJ, Berman DS, Koo BK, van Mieghem C, et al. Diagnostic accuracy of fractional flow reserve from anatomic CT angiography. JAMA 2012; 308: 1237–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Choi JH, Min JK, Labounty TM, Lin FY, Mendoza DD, Shin DH, et al. Intracoronary transluminal attenuation gradient in coronary CT angiography for determining coronary artery stenosis. JACC Cardiovasc Imaging 2011; 4: 1149–57. doi: 10.1016/j.jcmg.2011.09.006 [DOI] [PubMed] [Google Scholar]
- 45.Ambrosius WT, Polonsky TS, Greenland P, Goff DC, Jr, Perdue LH, Fortmann SP, et al. Design of the value of imaging in enhancing the wellness of your heart (VIEW) trial and the impact of uncertainty on power. Clin Trials 2012; 9: 232–46. doi: 10.1177/1740774512436882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Douglas PS, Hoffmann U, Lee KL, Mark DB, Al-Khalidi HR, Anstrom K, et al. ; PROMISE Investigators. PROspective Multicenter Imaging Study for Evaluation of chest pain: rationale and design of the PROMISE trial. Am Heart J 2014; 167: 796–803.e1. doi: 10.1016/j.ahj.2014.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Blaha MJ, Budoff MJ, DeFilippis AP, Blankstein R, Rivera JJ, Agatston A, et al. Associations between C-reactive protein, coronary artery calcium, and cardiovascular events: implications for the JUPITER population from MESA, a population-based cohort study. Lancet 2011; 378: 684–92. doi: 10.1016/S0140-6736(11)60784-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nasir K, Shaw LJ, Budoff MJ, Ridker PM, Pena JM. Coronary artery calcium scanning should be used for primary prevention: pros and cons. JACC Cardiovasc Imaging 2012; 5: 111–18. doi: 10.1016/j.jcmg.2011.11.007 [DOI] [PubMed] [Google Scholar]
- 49.Miedema MD, Duprez DA, Misialek JR, Blaha MJ, Nasir K, Silverman MG, et al. Use of coronary artery calcium testing to guide aspirin utilization for primary prevention: estimates from the multi-ethnic study of atherosclerosis. Circ Cardiovasc Qual Outcomes 2014; 7: 453–60. doi: 10.1161/CIRCOUTCOMES.113.000690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bittencourt MS, Blaha MJ, Blankstein R, Budoff M, Vargas JD, Blumenthal RS, et al. Polypill therapy, subclinical atherosclerosis, and cardiovascular events-implications for the use of preventive pharmacotherapy: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol 2014; 63: 434–43. doi: 10.1016/j.jacc.2013.08.1640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Young LH, Wackers FJ, Chyun DA, Davey JA, Barrett EJ, Taillefer R, et al. ; DIAD Investigators. Cardiac outcomes after screening for asymptomatic coronary artery disease in patients with type 2 diabetes: the DIAD study: a randomized controlled trial. JAMA 2009; 301: 1547–55. doi: 10.1001/jama.2009.476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Muhlestein JB, Lappé DL, Lima JA, Rosen BD, May HT, Knight S, et al. Effect of screening for coronary artery disease using CT angiography on mortality and cardiac events in high-risk patients with diabetes: the FACTOR-64 randomized clinical trial. JAMA 2014; 312: 2234–43. doi: 10.1001/jama.2014.15825 [DOI] [PubMed] [Google Scholar]
- 53.Blankstein R, Murphy MK, Nasir K, Gazelle GS, Batlle JC, Al-Mallah M, et al. Perceived usefulness of cardiac computed tomography as assessed by referring physicians and its effect on patient management. Am J Cardiol 2010; 105: 1246–53. doi: 10.1016/j.amjcard.2009.12.040 [DOI] [PubMed] [Google Scholar]
- 54.LaBounty TM, Devereux RB, Lin FY, Weinsaft JW, Min JK. Impact of coronary computed tomographic angiography findings on the medical treatment and control of coronary artery disease and its risk factors. Am J Cardiol 2009; 104: 873–7. doi: 10.1016/j.amjcard.2009.05.024 [DOI] [PubMed] [Google Scholar]
- 55.Ovrehus KA, Bøtker HE, Jensen JM, Munkholm H, Johnsen SP, Nørgaard BL. Influence of coronary computed tomographic angiography on patient treatment and prognosis in patients with suspected stable angina pectoris. Am J Cardiol 2011; 107: 1473–9. doi: 10.1016/j.amjcard.2011.01.024 [DOI] [PubMed] [Google Scholar]
- 56.Cheezum MK, Hulten EA, Smith RM, Taylor AJ, Kircher J, Surry L, et al. Changes in preventive medical therapies and CV risk factors after CT angiography. JACC Cardiovasc Imaging 2013; 6: 574–81. doi: 10.1016/j.jcmg.2012.11.016 [DOI] [PubMed] [Google Scholar]
- 57.Uretsky S, Rozanski A, Supariwala A, Thotakura G, Kanneganti S, Satyanarayana N, et al. Clinical outcomes following a strategy of optimized medical management and selective “downstream” procedures following coronary computed tomography angiography. Int J Cardiol 2013; 165: 468–73. doi: 10.1016/j.ijcard.2011.08.852 [DOI] [PubMed] [Google Scholar]
- 58.Cheezum MK, Bittencourt MS, Hulten EA, Scirica BM, Villines TC, Blankstein R. Coronary computed tomographic angiography in the emergency room: state of the art. Expert Rev Cardiovasc Ther 2014; 12: 241–53. doi: 10.1586/14779072.2014.877345 [DOI] [PubMed] [Google Scholar]
- 59.Smith SC, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, et al. ; World Heart Federation and the Preventive Cardiovascular Nurses Association. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation 2011; 124: 2458–73. doi: 10.1161/CIR.0b013e318235eb4d [DOI] [PubMed] [Google Scholar]
- 60.Motoyama S, Sarai M, Narula J, Ozaki Y. Coronary CT angiography and high-risk plaque morphology. Cardiovasc Interv Ther 2013; 28: 1–8. doi: 10.1007/s12928-012-0140-1 [DOI] [PubMed] [Google Scholar]
- 61.Zeb I, Li D, Nasir K, Malpeso J, Batool A, Flores F, et al. Effect of statin treatment on coronary plaque progression - a serial coronary CT angiography study. Atherosclerosis 2013; 231: 198–204. doi: 10.1016/j.atherosclerosis.2013.08.019 [DOI] [PubMed] [Google Scholar]
- 62.Nissen SE, Nicholls SJ, Sipahi I, Libby P, Raichlen JS, Ballantyne CM, et al. ; ASTEROID Investigators. Effect of very high-intensity statin therapy on regression of coronary atherosclerosis: the ASTEROID trial. JAMA 2006; 295: 1556–65. [DOI] [PubMed] [Google Scholar]
- 63.Wolk MJ, Bailey SR, Doherty JU, Douglas PS, Hendel RC, Kramer CM, et al. ; American College of Cardiology Foundation Appropriate Use Criteria Task Force. ACCF/AHA/ASE/ASNC/HFSA/HRS/SCAI/SCCT/SCMR/STS 2013 multimodality appropriate use criteria for the detection and risk assessment of stable ischemic heart disease: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons. J Am Coll Cardiol 2014; 63: 380–406. doi: 10.1016/j.jacc.2013.11.009 [DOI] [PubMed] [Google Scholar]
- 64.Hachamovitch R, Nutter B, Hlatky MA, Shaw LJ, Ridner ML, Dorbala S, et al. ; SPARC Investigators. Patient management after noninvasive cardiac imaging results from SPARC (study of myocardial perfusion and coronary anatomy imaging roles in coronary artery disease). J Am Coll Cardiol 2012; 59: 462–74. doi: 10.1016/j.jacc.2011.09.066 [DOI] [PubMed] [Google Scholar]