Abstract
Acute angle closure glaucoma is an ophthalmic emergency and can lead to blindness if left untreated. Several types of drugs have the potential to precipitate acute angle closure glaucoma. These include adrenergic, cholinergic and anticholinergic, antidepressants, anticoagulants and sulfa-based agents. This article provides a basic overview of the risk factors and pathophysiologic mechanisms involved in angle closure glaucoma and focuses on drug-induced angle closure glaucoma for the non-ophthalmologist. A PubMed search limited to the English language was conducted to find relevant literature for the purpose of this article. Most attacks occur in subjects unaware that they are at risk due to innately narrow iridocorneal angles. Clinicians should always review medications in patients presenting with symptoms of acute angle closure glaucoma. The aim of this article is to bring this ophthalmic condition to the attention of clinicians, particularly those outside the field of ophthalmology who commonly prescribe these medications or see these patients prior to referring to ophthalmologists.
Keywords: angle closure, glaucoma, drug-induced, iatrogenic
Introduction
Acute angle closure glaucoma is an ophthalmic emergency. Delayed recognition and treatment can result in blindness. Typical presenting symptoms are acute onset of ocular pain, headache, blurred vision, nausea and vomiting. Clinical findings on examination are a significantly elevated intraocular pressure (IOP) above 21 mm Hg, corneal oedema, redness, a mid-dilated and fixed pupil and a shallow anterior chamber.1,2
Risk factors for acute angle closure
General risk factors for acute angle closure glaucoma are advanced age, female gender, strong family history, hypermetropia and Eskimo or Asian ethnicity.3–5 Certain anatomical features can also increase one's risk, these include a thick crystalline lens, plateau iris configuration and narrow iridocorneal angles.1 Previous studies have shown that the majority of acute angle-closure glaucoma presentations due to pupillary block occur in subjects that are not aware they were at risk due to innately narrow iridocorneal angles.6 Patients known to have innately narrow angles should be referred to an ophthalmologist for further investigation with gonioscopy and to grade the level of risk for acute angle closure glaucoma. Figures 1A and 1B illustrate a shallow anterior chamber at presentation and closed iridocorneal angles on gonioscopy respectively.7
Figure 1.
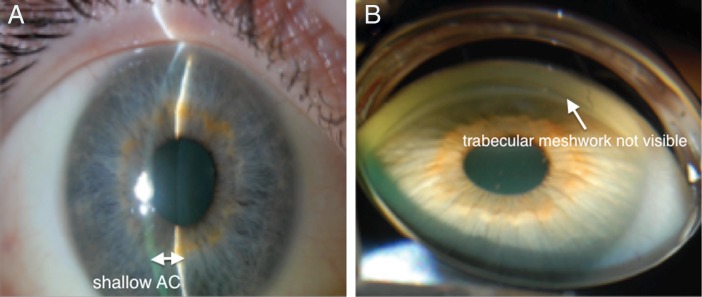
(A) shallow anterior chamber at presentation (B) closed iridocorneal angles on gonioscopy.
Pathophysiologic mechanisms of angle closure glaucoma
Pupillary block due to pupil dilatation is the most common mechanism of angle closure. It occurs when the pupil comes into contact with the lens and obstructs the aqueous flow from the posterior chamber to the anterior chamber. This causes an elevation in pressure within the posterior chamber, resulting in bowing of the peripheral iris anteriorly and apposition of the peripheral iris to the trabecular meshwork. Consequently, the aqueous cannot drain out and IOP rises (Figure 2).
Figure 2.
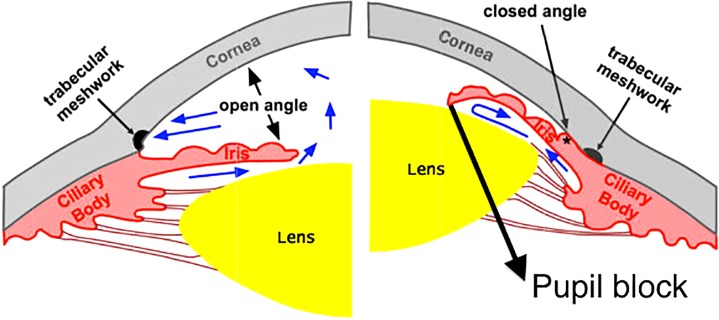
Mechanism of acute angle closure by pupil block by Melbourne Eye Centre available at http://melbourneeyecentre.com.au/glaucoma/closed-angle-glaucoma/.
Other than pupillary block, other mechanisms of angle closure include plateau iris, lens-related and posterior segment pathologies such as aqueous misdirection, choroidal effusion or posterior segment tumours behind the lens that cause forward displacement of the lens-iris diaphragm.
Drugs causing acute angle closure glaucoma
Several types of drugs can induce acute angle closure glaucoma. Table 1 lists the different types and examples of drugs that can precipitate angle closure and their mechanisms of action.8
Table 1.
Drugs that have the potential to precipitate acute angle closure glaucoma.
| Class of drug | Example of drug | Route of administration | Mechanism of angle closure |
|
| |||
| Adrenergic agonists | Phenylephrine | Eye drops | Pupillary block |
|
| |||
| Ephedrine | Intravenous | Pupillary block | |
|
| |||
| Non-catecholamine adrenergic agonists | Naphazoline | Intranasal | Pupillary block |
|
| |||
| Salbutamol | Inhalation | Pupillary block | |
|
| |||
| Anticholinergics | Tropicamide | Eye drops | Pupillary block |
|
| |||
| Ipratropium bromide | Inhalation | Pupillary block | |
|
| |||
| Promethazine (antihistamine) | Oral | Pupillary block | |
|
| |||
| Botulinum toxin | Periocular (local) | Pupillary block | |
|
| |||
| Cholinergics | Pilocarpine | Eye drops | Forward displacement of lens-iris diaphragm |
|
| |||
| Medications with anticholinergic side effects | Imipramine (tricyclic antidepressant) | Oral | Pupillary block |
|
| |||
| Fluoxetine (serotonin reuptake inhibitor) | Oral | Pupillary block | |
|
| |||
| Sulfa-based agents | Topiramate | Oral | Ciliochoroidal effusion leading to forward displacement of lens-iris diaphragm |
|
| |||
| Acetazolamide | Oral | Ciliochoroidal effusion leading to forward displacement of lens-iris diaphragm | |
|
| |||
| Anticoagulants | Heparin | Subcutaneous | Forward displacement of lens-iris diaphragm |
|
| |||
Adrenergic agonists
Alpha-adrenergic agonists can precipitate acute angle closure glaucoma by pupillary block due to pupil dilatation in individuals with innately narrow iridocorneal angles. Phenylephrine (alpha-adrenergic agonist) eye drops are often administered by opticians and ophthalmologists to dilate the pupil for fundus examination, a prime example of iatrogenicity. The estimated incidence of acute angle closure glaucoma following diagnostic pupil dilatation has been reported to be 0.03 percent.9
Systemic ephedrine is often administered to manage hypotension, particularly in the setting of general anaesthesia. Whilst a diagnostic challenge (as physicians are more likely to have intraoperative corneal abrasions on the top of their differentials for a painful postoperative eye), Lentschener et al.,10 actually reported a case of postoperative acute angle closure glaucoma following non-ophthalmic surgery due to the use of intraoperative ephedrine. This serves as a cautionary tale as the effects, both positive or negative of intraoperative sympathomimetic drugs can be compounded by psychological stress, thus heightening the risk for acute angle closure glaucoma. Symptoms of acute angle closure glaucoma can easily be misinterpreted or overlooked in a recently anaesthetized patient. Hence, clinicians should have a low threshold to refer for an ophthalmic assessment in any patient complaining of vision loss or with a red eye postoperatively.
Non-catecholamine adrenergic agonists
Cases of acute angle closure glaucoma have been reported following administration of nasal ephedrine and naphazoline to treat epistaxis. The postulated mechanism of angle closure was reflux through the ipsilateral nasolacrimal duct. In fact, there was even one case where it was hypothesized that absorption of a nasal decongestant through the nasal mucosa used for a week triggered bilateral acute angle closure glaucoma in a patient.11,12 Adrenergic agents such as salbutamol are commonly found in nebulizers and inhalers used in the management of asthma, flu remedies or rectal suppositories. Salbutamol is a beta-2-adrenergic receptor agonist that stimulates beta-2-adrenergic receptors in the ciliary body to promote aqueous humour secretion. Angle closure is exacerbated by pupil dilatation caused by the parasympathetic inhibitory effect of ipratropium, often combined with salbutamol in nebulizers or inhalers. However, it should be noted that salbutamol does not induce angle closure when used alone. Therefore, caution should be exercised when prescribing or administering these medications together, many of which can be obtained over-the-counter.
Anticholinergic agents
Tropicamide drops are commonly administered for the purpose of ocular fundus examination and have been associated with acute angle closure glaucoma. Other longer acting anticholinergic eye drops such as atropine and cyclopentolate, administered for ciliary muscle relaxation and pupil dilatation, are also known to precipitate angle closure.13
Nebulized ipratropium bromide is an antimuscarinic agent commonly administered in combination with salbutamol for patients presenting with acute asthma or exacerbation of chronic obstructive pulmonary disease. Several case reports have described its association with acute angle closure glaucoma.14–16 The postulated mechanism of angle closure is that ipratropium bromide escaping the oxygen mask and diffusing into the cornea, induces pupil dilatation and subsequent pupillary block. Therefore, clinicians should ensure that the oxygen masks are properly fitted and positioned in order to reduce the risk of contact between the cornea and medication. Kalra and Bone17 studied the effect of nebulized bronchodilator therapy on intraocular pressures in patients with glaucoma. They concluded that whilst it is relatively safe to use nebulized ipratropium bromide and salbutamol separately in patients with narrow-angle glaucoma, a combination of the two drugs carries a higher risk of inducing an attack of acute angle closure glaucoma in susceptible patients.
Antihistamines (H1 and H2 receptor blockers) can also induce acute angle closure glaucoma due to their anticholinergic properties. Promethazine has been reported to cause swelling of the lens that can in turn result in pupillary block. Ranitidine and cimetidine used in the treatment of gastroesophageal reflux and peptic ulcers have also been shown to increase intraocular pressure in individuals known to have glaucoma.2,6
Botulinum toxin
The cosmetic industry has seen a surge in the popularity of botulinum toxin use over the past decades. There is limited literature on the exact pathophysiology of acute angle closure glaucoma precipitated by periorbital botulinum toxin injections. Botulinum toxin is thought to induce acute angle closure glaucoma due to its anticholinergic effect on the sympathetic ganglia, preganglionic and postganglionic nerve terminals of the parasympathetic nervous system. This subsequently results in inhibition of the pupillary sphincter that causes pupil dilatation and pupillary block. Previous literature has recommended that patients receiving botulinum toxin injections for cosmetic reasons should undergo ophthalmic investigations including gonioscopy before starting treatment to evaluate their angle closure risk profile and determine if laser iridotomy is of any benefit.18 However, it is not always practical for physicians to send every patient receiving botulinum injections to an ophthalmologist for gonioscopy. A simpler method that can be used to estimate the depth of the anterior chamber is the use of the oblique penlight illumination test. The penlight is pointed temporally and parallel to the plane of the iris to shine the light nasally. An entirely illuminated iris signifies a wide-open anterior chamber. Patients with a shallow anterior chamber have a convex iris as it bows forward over the lens. Hence, the presence of a nasal shadow indicates a shallow anterior chamber.
Corridan et al.,19 reported a case of acute angle closure glaucoma precipitated by periorbital botulinum toxin injections for the treatment of blepharospasm. The postulated mechanism of angle closure was diffusion of the toxin from the injection site to the ciliary ganglion, thereby inducing pupil dilatation.
Cholinergic agents
Pilocarpine acts as an agonist on the parasympathetic nervous system that results in pupil constriction (miosis). Pilocarpine eye drops are used in the treatment of angle closure glaucoma for its miotic effect. It also helps in reducing the intraocular pressure by enhancing the aqueuous outflow. However, pilocarpine can induce acute angle closure glaucoma in its own right, as a result of forward displacement of the lens-iris diaphragm.6
Antidepressants
Tricyclic antidepressants e.g., clomipramine, imipramine, amitryptyline and selective serotonin reuptake inhibitors (SSRI) e.g., venlafaxine, citalopram, escitalopram, fluoxetine and paroxetine have been reported to precipitate acute angle closure glaucoma. The underlying mechanism is pupillary block caused by pupil dilatation, which is attributed to the significant anticholinergic and serotonergic side effects of these antidepressants.20–23 The role of serotonin in human ocular physiology however has yet to be determined. Clinicians should consider referring patients at increased risk of acute angle closure glaucoma for an ophthalmic assessment prior to prescribing SSRIs.
Antidepressants containing monoamine oxidase inhibitors such as tranylcypromine sulphate or phenelzine sulphate have weak anticholinergic effects. However, they have been reported to precipitate acute angle closure glaucoma when used in combination with other anticholinergic drugs.24
Antipsychotics including trifluoperazine, perphenazine and fluphenazine have also been reported to induce acute angle closure glaucoma, but have weaker anticholinergic effects than tricyclic antidepressants on ocular smooth muscle.2,6
Sulfa-based agents
Sulfa-based agents such as topiramate, acetazolamide and hydrochlorothiazide are among the few drugs that can induce “non-pupillary block” acute angle closure glaucoma. Lee et al.,25 have reported that sulfa-based drugs can cause shallowing of the anterior chamber, choroidal effusion, increased intraocular pressure, swelling of the lens and retinal oedema. The typical presentation is blurred vision due to forward displacement of the lens-iris diaphragm (myopia). The exact mechanism by which sulfa-based agents cause acute angle closure glaucoma is unknown. Ciliary body swelling and anterior choroidal effusion can both cause forward displacement of the iris-lens diaphragm resulting in obstruction to aqueous flow and subsequent acute angle closure glaucoma. Both mechanisms can also reduce the diameter of the ciliary body ring, leading to zonular laxity that facilitates lens thickening and further decreases the anterior chamber depth.26
Topiramate is commonly used for migraines and weight loss. Although some literature describe topiramate-induced as type B reactions i.e., idiosyncratic reactions, quite a number of reports have actually described cases of bilateral acute angle closure glaucoma induced by topiramate in patients with narrow angles.27–29 The main mechanism of angle closure precipitated by topiramate is choroidal effusion. Ultrasound images have shown that a contributing factor is topiramate-induced ciliary oedema causing relaxation of the zonules, which in turn increases the lens thickness. The resulting effect is anterolateral rotation of the ciliary body, forward displacement of the lens-iris diaphragm and consequent shallowing of the anterior chamber.30 More than 100 previously published cases of topiramate-induced angle closure described bilateral non-pupillary block acute angle closure glaucoma (only three cases of unilateral involvement) after taking the first doses of the medication. The attacks typically occurred between days 1 and 49 and resolved after discontinuing the causative agent.2 It is important to emphasize that topiramate induces mostly bilateral attack of angle closure glaucoma that occurs simultaneously in both eyes. The element of bilaterality is a clear sign that the acute attack is drug-induced.
Spadoni et al.,31 reported a case of permanent bilateral loss of vision following acute angle closure glaucoma induced by sulfamethoxazole-trimethoprim, despite stopping the medication.
The management of sulfa drug-induced acute angle closure glaucoma involves stopping the medication and controlling the intraocular pressure with topical or systemic steroid and cycloplegics. Topical miotics should be avoided as they have the potential of causing pupillary block. Moreover, laser iridotomy is of no benefit in these cases.32
Acetazolamide is routinely used in ophthalmic and neurologic practice to reduce intraocular and intracranial pressure. Incidentally, oral acetazolamide is commonly administered for one day following cataract surgery to prevent excessive intraocular pressure increases. A few case reports have described acute bilateral angle-closure glaucoma and choroidal effusion associated with acetazolamide administration following cataract surgery.33–35 Therefore, clinicians should consider this important adverse effect of acetazolamide in patients who develop acute angle-closure glaucoma after cataract surgery.
Anticoagulants
Rare complications associated with anticoagulant therapy including massive vitreous, choroidal or subretinal haemorrhage, may induce acute angle-closure glaucoma. The mechanism for angle closure is the sudden forward displacement of the lens-iris diaphragm resulting from the detached retina or choroid. Risk factors are over-anticoagulation, nanophthalmos and exudative age-related macular degeneration.36–38
Since the mechanism of angle closure is non-pupillary block, peripheral iridotomy is not effective in these cases. It is suggested that the clinician should consider discontinuing the anticoagulant to prevent further haemorrhage, particularly in the contralateral eye.39
Conclusion
The presenting symptoms of patients with acute angle-closure glaucoma can be misleading because headache, blurred vision, abdominal pain, nausea and vomiting are non-specific symptoms. However, sudden onset of visual disturbance and a mid-dilated pupil are suggestive of acute angle-closure glaucoma. Hyperopic glasses (for long-sightedness) are a telltale sign for acute angle-closure glaucoma in patients presenting with these symptoms. It is not possible for clinicians prescribing these drugs to refer all patients for ophthalmic investigations. Moreover, it is difficult to identify all patients at risk of acute angle-closure glaucoma, as the majority of these patients are asymptomatic and unaware of the increased risk associated with innately narrow iridocorneal angles. Patients known to have angle closure glaucoma are typically treated with laser iridotomy, filtering surgery or cataract extraction to prevent attacks of acute angle-closure glaucoma. These patients who have undergone laser iridotomy should be able to safely take medications that have the potential to induce acute angle-closure glaucoma only by pupillary block. This educational review illustrates the importance for clinicians to be mindful of medications that can potentially precipitate acute angle-closure glaucoma. A careful history taking and obtaining a detailed list of both prescribed and non-prescribed medications– including discontinued ones–in patients presenting with acute angle-closure glaucoma can help identify the causative drug(s). Once the diagnosis is suspected, urgent medical intervention is required as appropriate and prompt management potentially can be sight saving.
References
- 1.Lai JS, Gangwani RA. Medication-induced acute angle closure attack. Hong Kong Med J. 2012;18(2):139–145. [PubMed] [Google Scholar]
- 2.Razeghinejad MR, Myers JS, Katz LJ. Iatrogenic glaucoma secondary to medications. Am J Med. 2011 Jan;124(1):20–25. doi: 10.1016/j.amjmed.2010.08.011. [DOI] [PubMed] [Google Scholar]
- 3.Wang L, Zhang X, Cai S, Ma J, Liu X, Wang N. Correlated or not: Glaucoma prevalence and modern industrialization. Med Hypotheses. 2011;76(2):220–224. doi: 10.1016/j.mehy.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 4.Tarongoy P, Ho CL, Walton DS. Angle-closure glaucoma: the role of the lens in the pathogenesis, prevention, and treatment. Surv Ophthalmol. 2009;54(2):211–225. doi: 10.1016/j.survophthal.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 5.Kavitha S, Zebardast N, Palaniswamy K, Wojciechowski R, Chan ES, Friedman DS, Venkatesh R, Ramulu PY. Family history is a strong risk factor for prevalent angle closure in a South Indian population. Ophthalmology. 2014 Nov;121(11):2091–2097. doi: 10.1016/j.ophtha.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 6.Lachkar Y, Bouassida W. Drug-induced acute angle closure glaucoma. Curr Opin Ophthalmo. 2007;18(2):129–133. doi: 10.1097/ICU.0b013e32808738d5. [DOI] [PubMed] [Google Scholar]
- 7.Liu Y, Rhee DJ. Acute bilateral angle closure. JAMA Ophthalmol. 2013;131(9):1231–1232. doi: 10.1001/jamaophthalmol.2013.5186. [DOI] [PubMed] [Google Scholar]
- 8.Rudkin AK, Gray TL, Awadalla M, Craig JE. Bilateral simultaneous acute angle closure glaucoma precipitated by non-prescription cold and flu medication. Emerg Med Australas. 2010;22(5):477–479. doi: 10.1111/j.1742-6723.2010.01338.x. [DOI] [PubMed] [Google Scholar]
- 9.Wolfs RC, Grobbee DE, Hofman A, de Jong PT. Risk of acute angle-closure glaucoma after diagnostic mydriasis in nonselected subjects: the Rotterdam Study. Invest. Ophthalmol. Vis. Sci. 1997;38:2683–2687. [PubMed] [Google Scholar]
- 10.Lentschener C, Ghimouz A, Bonnichon P, Parc C, Ozier Y. Acute postoperative glaucoma after nonocular surgery remains a diagnostic challenge. Anesth Analg. 2002;94:1034–1035. doi: 10.1097/00000539-200204000-00049. [DOI] [PubMed] [Google Scholar]
- 11.Zenzen CT, Eliott D, Balok EM. Acute angle-closure glaucoma associated with intranasal phenylephrine to treat epistaxis. Arch Ophthalmol. 2004;122:655–656. doi: 10.1001/archopht.122.4.655. [DOI] [PubMed] [Google Scholar]
- 12.Khan MAJ, Watt LL, Hugkulstone CE. Bilateral acute angle-closure glaucoma after use of FenoxTM nasal drops. Eye. 2002;16:662–663. doi: 10.1038/sj.eye.6700125. [DOI] [PubMed] [Google Scholar]
- 13.Brooks AM, West RH, Gillies WE. The risk of precipitating acute angle-closure glaucoma with the clinical use of mydriatic agents. Med J Aust. 1986;145:34–36. doi: 10.5694/j.1326-5377.1986.tb113739.x. [DOI] [PubMed] [Google Scholar]
- 14.De Saint Jean M, Boursier T, Borderie V. Acute closure-angle glaucoma after treatment with ipratropium bromide and salbutamol aerosols. J Fr Ophthalmol. 2000;23:603–605. [PubMed] [Google Scholar]
- 15.Lellouche N, Guglielminotti J, de Saint-Jean M, Alzieu M, Maury E, Offenstadt G. Acute glaucoma in the course of treatment with aerosols of ipratropium bromide and salbutamol. Presse Med. 1999 May;28(19):1017. [PubMed] [Google Scholar]
- 16.Reuser T, Flanagan DW, Borland C, Bannerjee DK. Acute angle closure glaucoma occurring after nebulized bronchodilator treatment with ipratropium bromide and salbutamol. J R Soc Med. 1992;85(8):499–500. doi: 10.1177/014107689208500828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kalra L, Bone MF. The effect of nebulized bronchodilator therapy on intraocular pressures in patients with glaucoma. Chest. 1988 Apr;93(4):739–741. doi: 10.1378/chest.93.4.739. [DOI] [PubMed] [Google Scholar]
- 18.Zheng L, Azar D. Angle-closure glaucoma following periorbital botulinum toxin injection. Clin Experiment Ophthalmol. 2014 Sep-Oct;42(7):690–693. doi: 10.1111/ceo.12293. [DOI] [PubMed] [Google Scholar]
- 19.Corridan P, Nightingale S, Mashoudi N, Williams AC. Acute angle closure glaucoma following botulinum toxin injection for blepharospasm. Br J Ophthalmol. 1990;74:309–310. doi: 10.1136/bjo.74.5.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Epstein NE, Goldbloom DS. Oral imipramine and acute angle-closure glaucoma. Arch Ophthalmol. 1995;113:698. doi: 10.1001/archopht.1995.01100060020008. [DOI] [PubMed] [Google Scholar]
- 21.Schlingemann RO, Smit AA, Lunel HF, Hijdra A. Amaurosis fugax on standing and angle-closure glaucoma with clomipramine. Lancet. 1996;347:465. doi: 10.1016/s0140-6736(96)90041-0. [DOI] [PubMed] [Google Scholar]
- 22.Browning AC, Reck AC, Chisholm IH, Nischal KK. Acute angle closure glaucoma presenting in a young patient after administration of paroxetine. Eye. 2000;14:406–408. doi: 10.1038/eye.2000.106. [DOI] [PubMed] [Google Scholar]
- 23.Ng B, Sanbrook GMC, Malouf AJ, Agarwal SA. Venlafaxine and bilateral acute angle closure glaucoma. Med J Aust. 2002;176:241. doi: 10.5694/j.1326-5377.2002.tb04386.x. [DOI] [PubMed] [Google Scholar]
- 24.Richa S, Yazbek JC. Ocular adverse effects of common psychotropic agents: a review. CNS Drugs. 2010;24:501–526. doi: 10.2165/11533180-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 25.Quaglito LB, Barella K, Abreu NJM, Quaglito EM. Topiramate-associated acute, bilateral, angle-closure glaucoma: case report. Arg Bras Oftalmol. 2013 Jan-Feb;76(1):48–49. doi: 10.1590/s0004-27492013000100014. [DOI] [PubMed] [Google Scholar]
- 26.Panday VA, Rhee DJ. Review of sulfonamide-induced acute myopia and acute bilateral angle-closure glaucoma. Compr Ophthalmol Update. 2007 Sep-Oct;8(5):271–276. [PubMed] [Google Scholar]
- 27.Lee GC, Tam CP, Danesh-Meyer HV, Myers JS, Katz LJ. Bilateral angle closure glaucoma induced by sulphonamide-derived medications. Clin Experiment Ophthalmol. 2007;35:55–58. doi: 10.1111/j.1442-9071.2006.01365.x. [DOI] [PubMed] [Google Scholar]
- 28.Levy J, Yagev R, Petrova A, Lifshitz T. Topiramate-induced bilateral angle-closure glaucoma. Can J Ophthalmol. 2006;41:221–225. doi: 10.1139/I06-012. [DOI] [PubMed] [Google Scholar]
- 29.Rhee DJ, Ramos-Esteban JC, Nipper KS. Rapid resolution of topiramate-induced angle-closure glaucoma with methylprednisolone and mannitol. Am J Ophthalmol. 2006;141:1133–1134. doi: 10.1016/j.ajo.2006.01.021. [DOI] [PubMed] [Google Scholar]
- 30.Ikeda N, Ikeda T, Nagata M, Mimura O. Ciliochoroidal effusion syndrome induced by sulfa derivatives. Arch Ophthalmol. 2002;120:1775. doi: 10.1001/archopht.120.12.1775. [DOI] [PubMed] [Google Scholar]
- 31.Spadoni VS, Pizzol MM, Muniz CH, Melamed J, Fortes Filho JB. Bilateral angle-closure glaucoma induced by trimethoprim and sulfamethoxazole combination: a case report. Arq Bras Oftalmol. 2007;70:517–520. doi: 10.1590/s0004-27492007000300023. [DOI] [PubMed] [Google Scholar]
- 32.Fraunfelder FW, Fraunfelder FT, Keates EU. Topiramate-associated acute, bilateral, secondary angle-closure glaucoma. Ophthalmology. 2004;111:109–111. doi: 10.1016/j.ophtha.2003.04.004. [DOI] [PubMed] [Google Scholar]
- 33.Parthasarathi S, Myint K, Singh G, Mon S, Sadasivam P, Dhillon B. Bilateral acetazolamide-induced choroidal effusion following cataract surgery. Eye (Lond) 2007 Jun;21(6):870–872. doi: 10.1038/sj.eye.6702741. [DOI] [PubMed] [Google Scholar]
- 34.Mancino R, Varesi C, Cerulli A, Aiello F, Nucci C. Acute bilateral angle-closure glaucoma and choroidal effusion associated with acetazolamide administration after cataract surgery. J Cataract Refract Surg. 2011 Feb;37(2):415–417. doi: 10.1016/j.jcrs.2010.12.032. [DOI] [PubMed] [Google Scholar]
- 35.Malagola R, Arrico L, Giannotti R, Pattavina L. Acetazolamide-induced cilio-choroidal effusion after cataract surgery: unusual posterior involvement. Drug Des Devel Ther. 2013;7:33–36. doi: 10.2147/DDDT.S38324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schlote T, Freudenthaler N, Gelisken F. Anticoagulative therapy in patients with exudative age-related macular degeneration: acute angle closure glaucoma after massive intraocular hemorrhage. Ophthalmologe. 2005;102:1090–1096. doi: 10.1007/s00347-004-1096-z. [DOI] [PubMed] [Google Scholar]
- 37.Caronia RM, Sturm RT, Fastenberg DM, Berke SJ, Weintraub J. Bilateral secondary angle-closure glaucoma as a complication of anticoagulation in a nanophthalmic patient. Am J Ophthalmol. 1998;126:307–309. doi: 10.1016/s0002-9394(98)00101-9. [DOI] [PubMed] [Google Scholar]
- 38.Neudorfer M, Leibovitch I, Goldstein M, Loewenstein A. Massive choroidal hemorrhage associated with low molecular weight heparin therapy. Blood Coagul Fibrinolysis. 2002;13:257–259. doi: 10.1097/00001721-200204000-00012. [DOI] [PubMed] [Google Scholar]
- 39.Pesin SR, Katz LJ, Augsburger JJ, Chien AM, Eagle RC., Jr Acute angle-closure glaucoma from spontaneous massive hemorrhagic retinal or choroidal detachment. An updated diagnostic and therapeutic approach. Ophthalmology. 1990 Jan;97(1):76–84. doi: 10.1016/s0161-6420(90)32639-8. [DOI] [PubMed] [Google Scholar]


