Abstract
Introduction:
Restoration of normal anatomic alignment is a key component of the treatment of distal radius fractures (DRF). This study aimed to evaluate the accuracy of ultrasonography (US) in determining the adequacy of closed reduction in these fractures.
Methods:
DRF patients admitted to the emergency department of Al-Zahra Hospital, Isfahan, Iran from September 2011 to 2012, were enrolled. After closed reduction, the adequacy was investigated through both US and control plain radiography. Then, sensitivity, specificity, positive and negative predicative values of US in confirmation of closed reduction was evaluated. In addition, inter-rater agreement between the two diagnostic tools was analyzed by calculating Cohen’s kappa coefficient.
Results:
Finally, 154 patients were evaluated (females: 53.9%) with mean age of 40.03±14.7 (range: 22-73). US had sensitivity, specificity, positive and negative predictive value of 99.3% (95%CI: 96.2-99.9), 100.0% (95%CI: 62.9-100.0), 100.0% (95%CI: 97.5-100.0), and 88.9% (95%CI: 51.7-98.1) in confirmation of the adequate reduction, respectively. In addition, inter-rater reliability was 0.94 (95%CI: 0.89-0.99; p<0.0001).
Conclusion:
It seems that US could be considered as a highly sensitive, accurate, easy to use, noninvasive and safe tool for guidance and confirmation of closed reduction in DRF.
Key Words: Radius fractures, closed fractures, reduction, ultrasonography
Introduction
Distal radius fractures (DRF) is one of the most common cause of emergency department visits, comprising approximately one-sixth of fracture cases (1, 2). Except for trauma, pathological fractures due to osteoporosis, especially in elderly patients, is also one of the causes for this type of fracture (3, 4). Depending on the type of fracture, management is different, but generally it needs closed reduction, casting and future follow-up (5). Restoration of normal or nearly normal anatomic alignment is acknowledged as a key component of the treatment of DRF.
At present, plain radiography is used as a control standard for reducing DRF (6). Conditions such as inflammation of surrounding soft tissues prevent the physician from gaining adequate information about the reduction procedure carried out, which in turn can lead to requesting repeated radiographs. It can increase the need for sedation, unnecessary exposure to x-rays, and infliction of higher expenses (7). Recently, the use of ultrasonography (US) instead of plain radiography has been under consideration as a practical monitoring tool of closed reductions in extra-articular DRF (1, 2, 6). Accordingly, the present study was aimed to evaluate the accuracy of bedside US for determining the adequacy of DRF reduction compared with standard plain radiography.
Methods
Study design and setting
This cross sectional study has been performed from September 2011 to September 2012 in the emergency department of Al-Zahra Hospital, Isfahan, Iran. The study protocol was approved by Isfahan University of Medical Sciences Institutional Review Board and registered in www.clinicaltrial.gov by registration code: NCT01823692. An informed consent was fulfilled by all enrolled patients. Based on the study protocol, US and radiographic findings were compared in the same group of patients.
Participants
Patients undergoing sono-guided manipulation and reduction were enrolled over a twelve-month period, representing a convenience sample. Eligible patients were prospectively recruited based on the inclusion criteria as age>18 and diagnosis of DRF based on plain radiography. In addition, the exclusion criteria consisted of the following: open fractures, fractures with more than 20° angulation, intra-articular involvement, comminuted fractures with neurovascular compromise, patients requiring surgery due to other causes, need to intensive care, and patients’ refusal to participate in the study.
Intervention
After registration of demographic data, the patients underwent manipulation and reduction by one emergency medicine specialist under Bier block regional anesthesia or procedural sedation-analgesia. This physician passed a comprehensive training course regarding to sono-guided reduction, and determining the sufficiency of reduction based on US findings. US was performed in a long axis in both anterior-posterior and lateral views (Figures 1 and 2). When the distal and proximal cortices aligned into a straight line (less than 3 mm difference), the reduction was defined as successful. Follow-up plain radiographs were also obtained in the anterior-posterior and lateral views (gold standard) and reviewed by one blinded radiologist. If plain radiographs had the following criteria, the reduction was considered successful: 1) normal radial inclination of 15-25°; 2) radial height at least 5 mm or higher; 3) volar/palmar tilt -10° to +20° (8) (Figure 3). Finally, proper fixation was applied. Distal radius was defined as a distance less than 3 cm from the radio-carpal joint (9).
Figure 1.
Anterior-posterior view: (A) before reduction; (B) after reduction
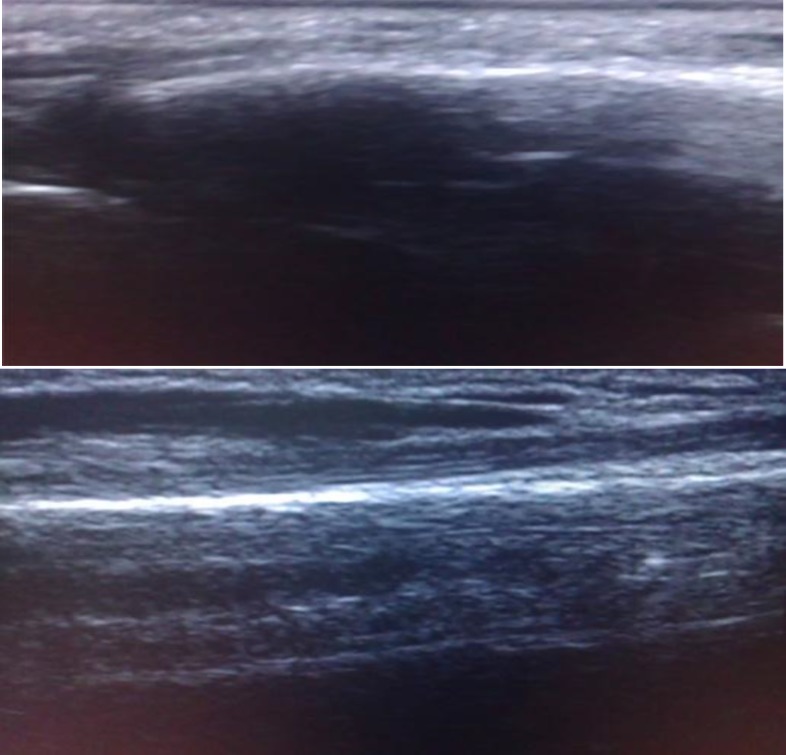
Figure 2.
Lateral view: (A) before reduction; (B) after reduction
Figure 3.
Conventional Radiographic Parameters. From left to right: Radial inclination; radial height; volar tilt
Statistical analysis
Following a descriptive analysis, the sensitivity, specificity, and positive and negative predicative values were calculated. In addition, Cohen’s kappa coefficient was used to evaluate inter-rater reliability between US and radiographic findings. Kappa index values <0.2, 0.21-0.4, 0.41-0.6, 0.61-0.8 and >0.8 were considered weak, rather weak, moderate, good, and excellent, respectively. Data were analyzed by SPSS version 20.0 and statistical significance was defined at p<0.05.
Results
Of the 180 patients initially enrolled in the study, 26 were excluded in the final analysis (10 with open fractures, six angulation>20°, five intra-articular involvement and five neurovascular compromise). Finally, 154 patients participated in this study (53.9% female; 55.2% right hand DRF) with mean age of 40.03±14.7 (range: 22-73). Table 1 present the baseline characteristics of these patients. Based on US and radiographic findings successful reduction was confirmed in 145 (94.2%) and 146 (94.8%) cases, respectively. US had sensitivity, specificity, positive and negative predictive value of 99.3%, 100.0%100.0%, and 88.9% in confirmation of successful reduction, respectively (Table 2). In addition, inter-rater agreement of reduction success between the two assessment methods was 99.35%. In addition, inter-rater reliability based on Cohen’s kappa coefficient was 0.94 (95% CI: 0.89-0.99; p<0.0001).
Table 1.
Patients’ baseline characteristics
| Variables | Number (%) |
|---|---|
| Age (year) | |
| 22-35 | 80 (52.0) |
| 36-50 | 33 (21.4) |
| 51-65 | 27 (17.5) |
| >66 | 14 (9.1) |
| Gender | |
| Male | 71 (46.1) |
| Female | 83 (53.9) |
| Side of fracture | |
| Left | 64 (41.6) |
| Right | 85 (55.2) |
| Both hands | 5 (3.2) |
| Anesthesia | |
| Procedural sedation | 141 (91.6) |
| Bier block | 13 (8.4) |
Table 2.
Accuracy of ultrasonography in confirmation of adequate reduction compare to radiography
| Screening characteristics | Value (%) | 95% CI |
|---|---|---|
| Sensitivity | 99.3 | 96.2-99.9 |
| Specificity | 100.0 | 62.9-100.0 |
| Positive predictive value | 100.0 | 97.5-100.0 |
| Negative predictive value | 88.9 | 51.7-98.1 |
| Positive likelihood ratio | --- | --- |
| Negative likelihood ratio | 0.01 | 0.00-0.05 |
CI: Confidence interval
Discussion
The results of the present study showed a high rate of similarity between US and radiographic findings in confirmation of adequate reduction. It seems that a sensitivity of 99.3% and a specificity of 100% make US a reliable tool for evaluation of successful reduction. Sono-guided reduction is an accurate, simple, and safe technique that provides the considerable advantage of real-time observation. In addition US should decrease the number of reduction attempts and consequently fewer traumas to the surrounding soft tissues (8).
Previous studies have been reported the sensitivity and specificity of US in confirming the adequacy of reduction between 94%-96% and 56%-97%, respectively (2, 10). Considering the limitation of US in observation of the articular surface, because of their deep-seated position and blocked by carpal component, we excluded all patients with intra-articular fractures. This fact could explain the high sensitivity and specificity of this study. Multiple studies have been declared the successful utility of sono-guided reduction for different type of fractures. Ang et al. stated that US guidance is effective and recommended it for routine use in the reduction of DRF (8). Eckert et al confirm that ultrasound is an applicable and safe alternative tool to x-rays in non-displaced forearm fractures (10). Chern et al. depicted that all parameters measured on the US and radiographic findings showed remarkable restoration of anatomic alignment after reduction, and all indicators were the same on the two types of images (11).
Some inherent characteristics of US such as: inability to bone penetration, observation of articular surface, and measurement of conventional radiographic parameters); unlike successful rate in different age (12, 13); quality and quantity of the training courses; and operator dependency; are among limitations in the widespread use of US for guidance and confirmation of closed fracture reduction in ED. Therefore, our result may not be applicable to other age groups, or other fracture sites. In addition, although we standardized the initial training for the physicians, our study size was too small to make meaningful subgroup analysis based on level of training or prior US experience. Finally, while US has some limitations that prevent it from completely replacing conventional radiography, it can facilitate the reduction and prevent repeated reduction attempts.
Conclusion:
It seems that US could be considered as a highly sensitive, accurate, easy to use, noninvasive and safe tool for guidance and confirming of closed reduction in DRF.
Acknowledgment
We thank the Emergency Department staff of Al-Zahra Hospital for helping us in conducting this study.
Conflict of interest:
None
Funding support:
This study was supported financially by Isfahan University of Medical Sciences, Isfahan, Iran.
Authors’ contributions:
All authors met all four recommended criteria of International Committee of Medical Journal Editors for authorship contribution.
References
- 1.Chen L, Kim Y, Moore CL. Diagnosis and guided reduction of forearm fractures in children using bedside ultrasound. Pediatr Emerg Care. 2007;23(8):528–31. doi: 10.1097/PEC.0b013e318128f85d. [DOI] [PubMed] [Google Scholar]
- 2.Chinnock B, Khaletskiy A, Kuo K, Hendey GW. Ultrasound-guided reduction of distal radius fractures. J Emerg Med. 2011;40(3):308–12. doi: 10.1016/j.jemermed.2009.09.018. [DOI] [PubMed] [Google Scholar]
- 3.Adams BD. Effects of radial deformity on distal radioulnar joint mechanics. J Hand surg. 1993;18(3):492–8. doi: 10.1016/0363-5023(93)90098-N. [DOI] [PubMed] [Google Scholar]
- 4.Cuenca J, Martinez A, Herrera A, Domingo J. The incidence of distal forearm fractures in Zaragoza (Spain) Chirurgie de la main. 2003;22(4):211–5. doi: 10.1016/s1297-3203(03)00057-x. [DOI] [PubMed] [Google Scholar]
- 5.Krackhardt T, Dilger J, Flesch I, Höntzsch D, Eingartner C, Weise K. Fractures of the distal tibia treated with closed reduction and minimally invasive plating. Arch Orthop Trauma Surg. 2005;125(2):87–94. doi: 10.1007/s00402-004-0778-y. [DOI] [PubMed] [Google Scholar]
- 6.Ackermann O, Liedgens P, Eckert K, et al. Ultrasound diagnosis of juvenile forearm fractures. J Med Ultrason. 2010;37(3):123–7. doi: 10.1007/s10396-010-0263-x. [DOI] [PubMed] [Google Scholar]
- 7.Durston W, Swartzentruber R. Ultrasound guided reduction of pediatric forearm fractures in the ED. Am J Emerg Med. 2000;18(1):72–7. doi: 10.1016/s0735-6757(00)90054-8. [DOI] [PubMed] [Google Scholar]
- 8.Ang S-H, Lee S-W, Lam K-Y. Ultrasound-guided reduction of distal radius fractures. Am J Emerg Med. 2010;28(9):1002–8. doi: 10.1016/j.ajem.2009.05.022. [DOI] [PubMed] [Google Scholar]
- 9.Mallmin H, Ljunghall S. Incidence of Colles' fracture in Uppsala: a prospective study of a quarter-million population. Acta Orthop. 1992;63(2):213–5. doi: 10.3109/17453679209154826. [DOI] [PubMed] [Google Scholar]
- 10.Eckert K, Ackermann O, Schweiger B, Radeloff E, Liedgens P. Sonographic diagnosis of metaphyseal forearm fractures in children: a safe and applicable alternative to standard X-rays. Pediatr Emerg Care. 2012;28(9):851–4. doi: 10.1097/PEC.0b013e318267a73d. [DOI] [PubMed] [Google Scholar]
- 11.Chern T-C, Jou I-M, Lai K-A, Yang C-Y, Yeh S-H, Cheng S-C. Sonography for monitoring closed reduction of displaced extra-articular distal radial fractures. J Bone Joint Surg. 2002;84(2):194–203. doi: 10.2106/00004623-200202000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Chang H, Tay S, Chan B, Low C. Conservative treatment of redisplayed collies' fractures in elderly patients older than 60 years old-anatomical and functional outcome. Hand Surg. 2001;6(02):137–44. doi: 10.1142/s0218810401000606. [DOI] [PubMed] [Google Scholar]
- 13.Anzarut A, Johnson JA, Rowe BH, Lambert RG, Blitz S, Majumdar SR. Radiologic and patient-reported functional outcomes in an elderly cohort with conservatively treated distal radius fractures. J Hand surg. 2004;29(6):1121–7. doi: 10.1016/j.jhsa.2004.07.002. [DOI] [PubMed] [Google Scholar]