Abstract
Introduction:
Burns can be very destructive, and severely endanger the health and lives of humans. It maybe cause disability and even psychological trauma in individuals. . Such an event can also lead to economic burden on victim’s families and society. The aim of our study is to evaluate epidemiology and outcome of burn patients referring to emergency department.
Methods:
This is a cross-sectional study was conducted by evaluation of patients’ files and forensic reports of burned patients’ referred to the emergency department (ED) of Akdeniz hospital, Turkey, 2008. Demographic data, the season, place, reason, anatomical sites, total body surface area, degrees, proceeding treatment, and admission time were recorded. Multinomial logistic regression was used to compare frequencies’ differences among single categorized variables. Stepwise logistic regression was applied to develop a predictive model for hospitalization. P<0.05 was defined as a significant level.
Results:
Two hundred thirty patients were enrolled (53.9% female). The mean of patients' ages was 25.3 ± 22.3 years. The most prevalence of burn were in the 0-6 age group and most of which was hot liquid scalding (71.3%). The most affected parts of the body were the left and right upper extremities. With increasing the severity of triage level (OR=2.2; 95% CI: 1.02-4.66; p=0.046), intentional burn (OR=4.7; 95% CI: 1.03-21.8; p=0.047), referring from other hospitals or clinics (OR=3.4; 95% CI: 1.7-6.6; p=0.001), and percentage of burn (OR=18.1; 95% CI: 5.42-62.6; p<0.001) were independent predictive factor for hospitalization. In addition, odds of hospitalization was lower in patients older than 15 years (OR=0.7; 95% CI: 0.5-0.91; p=0.035).
Conclusion:
This study revealed the most frequent burns are encountered in the age group of 0-6 years, percentage of <10%, second degree, upper extremities, indoor, and scalding from hot liquids. Increasing ESI severity, intentional burn, referring from other hospitals or clinics, and the percentage of burn were independent predictive factors for hospitalization.
Key Words: Emergency service, emergency room nursing, burns, hospital records
Introduction:
Burns can be very destructive, and severely endanger the health and lives of humans. It maybe cause disability and even psychological trauma in individuals. Such an event can also lead to economic burden on victim’s families and society (1). A vast majority (95%) of burn-related deaths occur in developing countries. Fire-related burns itself cause more than 300,000 deaths annually, in addition to a number of mortalities caused by scalding, electric burns, chemical burns or other types of burns (2). Like other types of trauma, children and elders have an increased frequency of burn incidents and mortality (3, 4). In developed countries, close to 90% of burning cases occur because of preventable incidents. Different training programs for all groups of the society, intended to prevent burns, are available (5). Since a national database regarding burn epidemiology is not available in Turkey, therefore obtaining definitive data about the risk factors and burns’ distribution is not possible in this country. Current national data on burns are either case reports belonged to various centers or regional outcomes based on descriptive studies (3). In Turkey, the data of the frequency, causes, and risk factors affect mortality should be collected, analyzed, and interpreted. Thus, measures especially for preventable types of burns should be planned. It has been observed that information contained in patient records is either not filled properly or at all, due to various causes such as shortage of health personnel, the sheer number of patients, serious illness, or trauma situations to which the intervention must be done quickly and health care providers’ experience negligence or unawareness of reporting (6). The aim of our study is to evaluate epidemiology and outcome of burn patients referring to emergency department.
Methods:
Study design and setting
This is a cross-sectional study, which was conducted by retrospective evaluation of registration data from burned patients for any reason and entered to the emergency department (ED) of Akdeniz University Hospital from January to December 2008. This study was conducted with the consent of the related department and approved by local ethics committee.
Participants
This was a retrospective study which all burn patients (242 cases), referred to the ED of Akdeniz hospital during the study period were evaluated. The incomplete patients’ files were excluded (12 cases). Finally, the data of 230 patients were entered to the study. Based on 65.7% hospitalization of burn patients (7), with considering α=0.05, and d=0.1, 84 patients were calculated as the minimum sample size.
Data collection
The data was collected from patients’ files, forensic reports, and computerized records. Age, gender, the season, place (the location burn occurred), and reason of the burns, the anatomical sites of the burns, total body surface area and degrees of the burns, proceedings before and during hospitalization, and admission time were recorded. For calculation of the burn degree, the higher available value was used. Causes of burns were analyzed into five main groups include hot liquid (water, milk, tea, soup, etc.), flame, electrical, chemical, contact with hot objects, and chemical. Burn sites in patients were anatomically classified as head and neck, anterior trunk, posterior trunk, right and left upper extremity, right and left lower extremity, and genital. Patients were divided as those discharged from hospital, hospitalized, dispatched to other ward, and rejected treatment. The triage level was assessed based on emergency severity index version IV (ESI). The percentage of burn was calculated based on rule of nines (8).
Statistical analysis
The obtained data was recorded and analyzed using SPSS version 21.0. Quantitative data were presented as mean ± standard deviation, while qualitative data as frequencies and percentages. Multinomial logistic regression was used to compare frequencies’ differences among single categorized variables. Stepwise logistic regression was applied to develop a predictive model for hospitalization. P<0.05 was defined as a significant level.
Results:
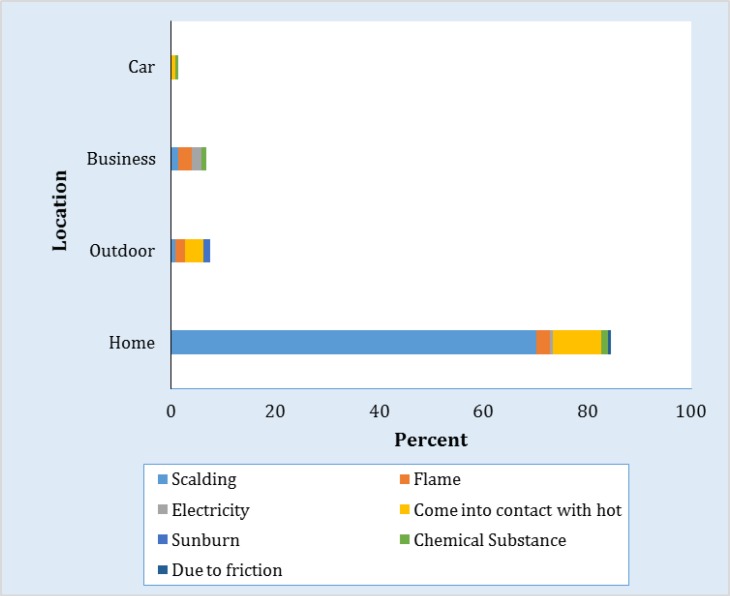
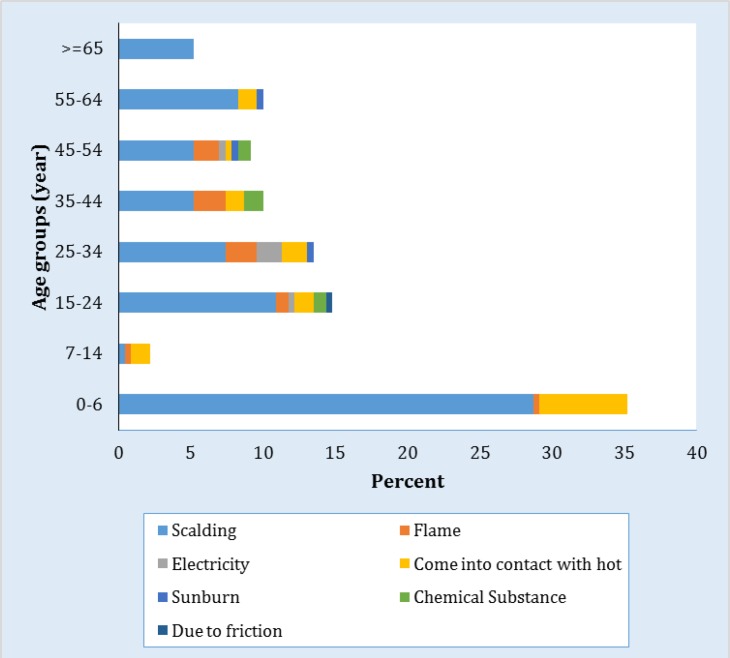
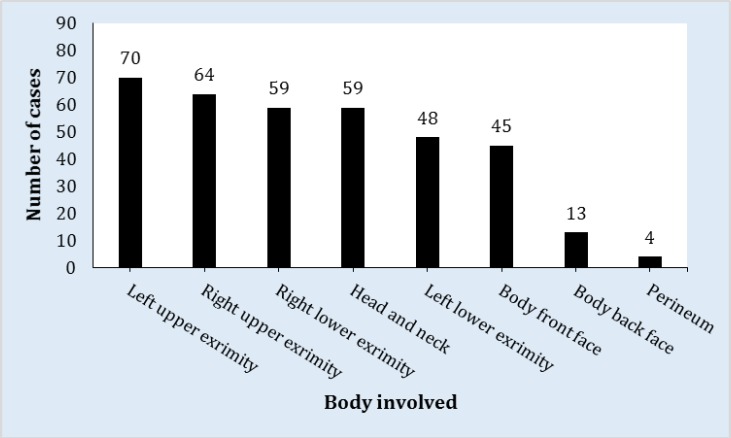
Findings of the retrospective evaluation showed that of 230 patients admitted to ED with burns, 124 (53.9%) of them were women and 106 (46.1%) men. Patients' ages ranged between 0-86 years and the average of age was 5.3 ± 22.3 years. Table 1 is summarized the background information of the studied subjects. When patients were analyzed according to age group, it was determined that most of them were in the 0-6 age group with 81 cases (35.2%). Multinomial logistic regression showed a significant difference among burn prevalence in age groups (p<0.0001). Based on this analysis, the prevalence of burn was significantly higher in ages under 7 years. Noticing to burn dates, the most admissions were in July with 13.9% (n=32) and the less in December with 4.8% (n=10) (p<0.001). One hundred ninety (82.6%) cases of burns occurred at home, 17 (7.4%) outdoors, 15 (6.5%) workplace, 3 (1.3%) inside a vehicle, and 5 (2.2%) unclear (p<0.001) (Figure 1). The most common cause of burns was hot liquid scalding, 71.3% (n=164), followed by contact with hot object 15.2% (n=35) (p<0.001). The most frequent percent and degree of burn were <10% (76.0%; p<0.001) and second-degree (67.8%; p<0.001), respectively. Figure 2 presents causes of burn in different age groups. As it can be seen, burn with boiling water is the most common reason of burn except the ages of 7-14 years. Also, in ages over 64 this is the only cause of burn. The most affected parts of the body are the left (n=70) and right upper extremities (n=64), while the least affected are genital (n=4) (p<0.001) (Figure 3). The majority of patients (70.9%) did not apply any treatment for their burns while at home. Two hundred thirteen cases (92.6%) were treated and dressed in the ED. While 79.6% of patients were discharged from the ED, 17.8% of them hospitalized. The length of hospitalization for 13% of the patients was 9 days or less (Table 2). Multivariate logistic regression demonstrated that with increasing the severity of ESI (OR=2.2; 95% CI: 1.02-4.66; p=0.046), intentional burn (OR=4.7; 95% CI: 1.03-21.8; p=0.047), referring from other hospitals or clinics (OR=3.4; 95% CI: 1.7-6.6; p=0.001), and percentage of burn (OR=18.1; 95% CI: 5.42-62.6; p<0.001) were independent predictive factor for hospitalization. In addition, odds of hospitalization was lower in patients older than 15 years (OR=0.7; 95% CI: 0.5-0.91; p=0.035) (Table 3).
Table 1.
Distribution of characteristics of burns of patients (N = 230)
| Variable | N (%) |
|---|---|
| Gender | |
| Female | 124 (53.9) |
| Male | 106 (46.1) |
| Age | |
| 0-6 | 81 (35.2) |
| 7-14 | 5 (2.2) |
| 15-24 | 34 (14.8) |
| 25-34 | 31 (13.5) |
| 35-44 | 23 (10.0) |
| 45-54 | 21 (9.1) |
| 55-64 | 23 (10.0) |
| 65 and over | 12 (5.2) |
| The season of burn | |
| Spring | 57 (24.8) |
| Summer | 71 (30.9) |
| Autumn | 59 (30.9) |
| Winter | 43 (30.9) |
| Burn that place | |
| Home | 190 (82.6) |
| Outdoor | 17 (7.4) |
| Business Location | 15 (6.5) |
| Car | 3 (1.3) |
| Unspecified | 5 (2.2) |
| Application received | |
| First 30 minutes | 86 (37.4) |
| The first 31 to 60 minutes | 54 (23.5) |
| The first 61 to 120 minutes | 15 (6.5) |
| The first two hours and more | 75 (32.6) |
| Burn reason | |
| Scalding | 164 (71.3 |
| Flame | 18 (7.8) |
| Electricity | 6 (2.6) |
| Come into contact with hot | 31 (13.5) |
| Sunburn | 3 (1.3) |
| Chemical Substance | 7 (3.0) |
| Due to friction | 1 (0.4) |
| Percentage of burn | |
| Less than 10% | 175 (76.1) |
| From 10 to 19% | 18 (7.8) |
| 20-29% | 8 (3.5) |
| 30-39% | 4 (1.7) |
| 40-49% arsine | 1 (0.4) |
| Between 50-59% | 3 (1.3) |
| unspecified | 121 (52.6) |
| Degree of burn | |
| 1 degree | 56 (24.3 |
| 2 degree | 110 (47.8) |
| 3 degree | 2 (0.9) |
| 1 and 2 degree | 46 (20.0) |
| 2 and 3 degree | 5 (2.2) |
| 1, 2, 3 degree | 2 (0.9) |
| unspecified | 9 (3.9) |
Figure 1.
cause of burn based on place
Figure 2.
The causes of burn based on age groups
Figure 3.
Distribution of Patients According to the Affected Anatomical Localizations
Table 2.
Distribution of the applications for burns (N = 230)
| Variable | N (%) |
|---|---|
| First Respond after Burns | |
| Applying water | 22 (9.6) |
| Applying ice | 16 (7.0) |
| Applying toothpaste, Tomato Sauce, Detergent and Shoe Polish | 6 (2.6) |
| Applying Bepanthen or Aloe Vera | 23 (10.0) |
| No application | 163 (70.9) |
| Treatment and Applications in Hospital | |
| Debridement and graft applied | 11 (4.8) |
| Medical dressing and treatment | 219 (95.2) |
| Disposition | |
| Discharged | 183 (79.6) |
| Hospitalizing in plastic and reconstructive surgery department | 30 (13.0) |
| Hospitalizing in reanimation unit | 8 (3.5) |
| Hospitalizing in eye department | 3 (1.3) |
| Referring to another healthcare organization | 4 (1.7) |
| Abandoning the emergency service | 1 (0.4) |
| Refusing the treatment | 1 (0.4) |
| Hospitalization Duration | |
| Hospitalization duration between 1-9 days | 30 (13.0) |
| Hospitalization duration between 10-19 days | 5 (2.2) |
| Hospitalization duration between 20-29 days | 2 (0.9) |
| Hospitalization duration between 30 days and over | 4 (1.7) |
| Not hospitalized | 189 (82.2) |
Table 3.
Independent risk factors for burn related hospitalization
| Variable | Odd ratio | 95% confidence interval | p |
|---|---|---|---|
| Increasing severity of ESI | 2.2 | 1.02-4.66 | 0.046 |
| Intentional burn | 4.7 | 1.03-21.8 | 0.047 |
| Refer from other hospital or clinics | 3.4 | 1.70-6.60 | 0.001 |
| Percentage of burn | 18.1 | 5.42-62.6 | <0.001 |
| Age over 15 years | 0.7 | 0.50-0.91 | 0.035 |
Discussion:
This study revealed that the most burn incidents occur in the 0-6 year’s age group and are a result of scalding. Both upper extremities were affected more frequently than other regions. Domestic burns are most common location of burn and second-degree burns encountered more frequently. In addition, increasing the severity of ESI, intentional burn, referring from other hospital or clinics, and the percentage of burn were independent predictive factors for hospitalization. Odds of hospitalization was lower in patients older than 15 years.
Panjeshahin et al. (9), Saadat et al. (10) and several other studies found that burn injuries were more common in females (11). While, Duzgun et al. (12) were determined that 61.7% and 54.8% of the patients were male. In this study it was seen that males less than woman were exposed to burns at a rate of 0.9:1. Because women spend more time at home than men, they are more exposed to home accidents and especially higher incidence of burns.
Study conducted by Kocaturk et al. (13) revealed that the mean age of burn experiencing was 21.3 years, while Gunay et al. (14) showed it as 22 years old. Additionally, more than half of these cases occurred in individuals under 14 years of age. Anlatıcı et al. (15) declared that burns happened in patients of 0-4 years old at a rate of 28% and Haberal et al. (16) demonstrated that the children constituted 56.7% of all patients experienced burns. The result of this study showed the higher incidence of burn among patients in 0-6 years’ age group.
The incidence of burn in summer was highly prevalent in this study unlike other reviews (17, 18). Chien et al.(17) and Dedovic et al. (18) stated that spring is the most common season to experience a burn and Sarıtas et al. (19) displayed that the majority of patients were admitted in winter (16%) and in the spring (30.7%). It was suggested that the rate of burn cases increase in Antalya during summer because of the fact that people spend more time at home because of the high temperature and summer holidays.
Home was the most frequent place of burn followed by outdoor, workplace, and inside of a vehicle. A literature review showed that the majority of burn cases occur indoors in developing countries similar to our study (20, 21). The arrival time to the hospital were observed 67.4% within 2 hours and 32.6% after 2 hours. Similarly, Cöl et al. (22) reported that 85.7% of burn patients referred to ED within the first 2 hours of the event. Santas et al. (19) stated that while 67% of the patients were discharged from ED after the first intervention, 16% of them hospitalized similar to the values in the present project. The most common cause of burns was scalding which was lined with some other studies (14, 23-26), although some reviews presented that other causes such as flame are more common (9, 11).This discrepancy may be due to the differences in burned population, jobs, and cultures.
In addition, the three most common burn sites included the left and right upper extremity, and head and neck similar to other studies (22, 27). The literatures stated that since persons experienced the burn trauma usually use his hands as a reflex to protect themselves, the most frequently burned sites of patients are hands, arms, face, and legs (28). Al et al. stated that 69.6% of patients applied cold water, burn ointment, or medical treatment, whereas 60.4% of them either did not apply the first aids or used it incorrectly (29). In the present project, because the majority of the patients (66.4%) referred to the ED within the first two hours, the number of patients who did not perform any medication was quite high.
Alcohol, drug intoxication (30), sex, inhalation injury, total body, surface area of burn, and total body surface area of burn were suggested in the several studies as hospitalization predictive factors (31). It was demonstrated that in addition to total body surface area (percentage of burn), age, increasing ESI severity, intentional burns, and referring from other hospitals or clinics were independent predictive values of hospitalization.
This study had some limitations; it was conducted retrospectively, only in one center and with small sample size.
Conclusion:
This study revealed the most frequent burns are encountered in the age group of 0-6 years, percentage of <10%, second degree, upper extremities, indoor, and scalding from hot liquids. Increasing ESI severity, intentional burn, referring from other hospitals or clinics, and the percentage of burn were independent predictive factors for hospitalization.
Acknowledgments:
The authors appreciate the insightful cooperation of staffs of the Emergency Department of Akdeniz University Hospital of Antalya, Turkey.
Conflict of interest:
None
Funding support:
None
Authors’ contributions:
All authors passed four criteria for authorship contribution based on recommendations of the International Committee of Medical Journal Editors.
References
- 1.Edelman LS. Social and economic factors associated with the risk of burn injury. Burns. 2007;33(8):958–65. doi: 10.1016/j.burns.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 2.Peck M, Molnar J, Swart D. A global plan for burn prevention and care. Bull World Health Organ. 2009;87(10):802–3. doi: 10.2471/BLT.08.059733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Simsek ME, Özgenel GY, Kahveci R, Akin S, Özbek S, Tufan F. Outcomes of elderly burn patients requiring hospitalization. Aging Male. 2014(0):1–3. doi: 10.3109/13685538.2014.920317. [DOI] [PubMed] [Google Scholar]
- 4.Zayakova Y, Vajarov I, Stanev A, Nenkova N, Hristov H. Epidemiological analysis of burn patients in East Bulgaria. Burns. 2014;40(4):683–8. doi: 10.1016/j.burns.2013.08.016. [DOI] [PubMed] [Google Scholar]
- 5.Liao C-C, Rossignol AM. Landmarks in burn prevention. Burns. 2000;26(5):422–34. doi: 10.1016/s0305-4179(00)00026-7. [DOI] [PubMed] [Google Scholar]
- 6.Kutlu L, Turasoy S, Koşar N, Ökdemir P. A Retrospective Evaluation of the Medical Records of Burn Patients Presenting at the Emergency Polyclinic of a University Hospital. J Edu Res Nursing. 2006;3(2):40–4. [Turkish] [Google Scholar]
- 7.Sakallıoğlu A, Başaran Ö, Tarım A, Türk E, Kut A, Haberal M. Burns in Turkish children and adolescents: nine years of experience. Burns. 2007;33(1):46–51. doi: 10.1016/j.burns.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 8.Dibildox M, Jeschke MG, Herndon DN. Burn Injury, Rule of Nines. Encyclopedia of Intensive Care Medicine. Springer; 2012. pp. 417–9. [Google Scholar]
- 9.Panjeshahin M-R, Lari AR, Talei A-R, Shamsnia J, Alaghehbandan R. Epidemiology and mortality of burns in the South West of Iran. Burns. 2001;27(3):219–26. doi: 10.1016/s0305-4179(00)00106-6. [DOI] [PubMed] [Google Scholar]
- 10.Saadat M. Epidemiology and mortality of hospitalized burn patients in Kohkiluye va Boyerahmad province (Iran): 2002–2004. Burns. 2005;31(3):306–9. doi: 10.1016/j.burns.2004.10.012. [DOI] [PubMed] [Google Scholar]
- 11.Aghakhani N, Rahbar N, Feizi A. Epidemiology of burn injuries in west Azerbaijan province, western Iran. Iran Red Crescent Med J. 2009;11(1):85–9. [Google Scholar]
- 12.Düzgün AP, Senel E, Ozmen MM, Kulaçoğlu H, Işik Y, Coşkun F. The evaluation of the patients admitted to a burn center in Turkey. Ulusal travma ve acil cerrahi dergisi= Turkish journal of trauma & emergency surgery: TJTES. 2003;9(4):250–6. [PubMed] [Google Scholar]
- 13.Kocaturk BK, Teyin M, Balcı Y, Esiyok B. Evaluation of burn cases presenting in the Osmangazi University Hospital emergency room Turkiye Klinikleri. J Med Sci. 2005;25(3):400–6. [Google Scholar]
- 14.Gunay K, Taviloglu K, Eskioglu E, Ertekin C. A study of epidemiology and mortality in burn patients. Ulus Travma Acil Cerrahi Derg . 1995;2(1):205–8. [Turkish] [Google Scholar]
- 15.Anlatici R, Ozerdem OR, Dalay C, Kesiktas E, Acarturk S, Seydaoglu G. A retrospective analysis of 1083 Turkish patients with serious burns. Burns. 2002;28(3):231–7. doi: 10.1016/s0305-4179(01)00095-x. [DOI] [PubMed] [Google Scholar]
- 16.Haberal M, Oner Z, Bayraktar U, Bilgin N. Epidemiology of adults' and childrens' burns in a Turkish burn center. Burns. 1987;13(2):136–40. doi: 10.1016/0305-4179(87)90103-3. [DOI] [PubMed] [Google Scholar]
- 17.Chien W-C, Pai L, Lin C-C, Chen H-C. Epidemiology of hospitalized burns patients in Taiwan. Burns. 2003;29(6):582–8. doi: 10.1016/s0305-4179(03)00133-5. [DOI] [PubMed] [Google Scholar]
- 18.Dĕdovic Z, Brychta P, Koupilova I, Suchanek I. Epidemiology of childhood burns at the Burn Centre in Brno, Czech Republic. Burns. 1996;22(2):125–9. doi: 10.1016/0305-4179(95)00106-9. [DOI] [PubMed] [Google Scholar]
- 19.Sarıtas A, Cıkman M, Candar M, Kandıs H, Baltacı D. Retrospective Analysis of Judicial Burn Cases Admitted to Our Clinic: 4-Year Experience. Duzce Med J. 2011;13(3):29–33. [Turkish] [Google Scholar]
- 20.Demirel Y, Col C, Ozen M. Evaluation of the patients treated in the Ankara Numune Hospital burn centre in one year. Cumhuriyet Med J. 2001;23(1):15–20. [Google Scholar]
- 21.Guzel A, Soyoral L, Oncu MR, Cakır C. Analysis of Patients who were Admitted to Burn Unit and Operated. Van Med J. 2012;19(1):1–7. [Google Scholar]
- 22.Çol M, Çol C, Afsar ZO, D Ç. An Epidemiological Analysis of Burned Cases Admitted by Ankara Numune Hospital. Health Soc Assist Found J. 1994;4(2):22–3. [Google Scholar]
- 23.Wasiak J, Spinks A, Ashby K, Clapperton A, Cleland H, Gabbe B. The epidemiology of burn injuries in an Australian setting, 2000–2006. Burns. 2009;35(8):1124–32. doi: 10.1016/j.burns.2009.04.016. [DOI] [PubMed] [Google Scholar]
- 24.Song C, Chua A. Epidemiology of burn injuries in Singapore from 1997 to 2003. Burns. 2005;31(1):S18–S26. doi: 10.1016/j.burns.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 25.Ansari-Lari M, Askarian M. Epidemiology of burns presenting to an emergency department in Shiraz, South Iran. Burns. 2003;29(6):579–81. doi: 10.1016/s0305-4179(03)00066-4. [DOI] [PubMed] [Google Scholar]
- 26.Kurtoŭlu M, Alimoğlu O, Ertekin C, Güloğlu R, Taviloğlu K. Evaluation of severe burns managed in intensive care unit. Ulusal travma ve acil cerrahi dergisi= Turkish journal of trauma & emergency surgery. TJTES. 2003;9(1):34–6. [Turkish] [PubMed] [Google Scholar]
- 27.Han TH, Kim JH, Yang MS, et al. A retrospective analysis of 19,157 burns patients: 18-year experience from Hallym Burn Center in Seoul, Korea. Burns. 2005;31(4):465–70. doi: 10.1016/j.burns.2004.11.014. [DOI] [PubMed] [Google Scholar]
- 28.Erkuran MK, Ceylan A, Düzenli E, Büyükcam F. Burn cases that are hospitalized in Sanlıurfa Education & Research Hospital. Abant Med J. 2013;2(2):123–9. [Google Scholar]
- 29.Al B, Gullu MN, Okur H, Ozturk H, Kara İH, Aldemir M. The epidemiology of scald and flame burns in east and South anatolia regions. J Med Invest. 2005;3(1):14–21. [Google Scholar]
- 30.Grobmyer S, Maniscalco S, Purdue G, Hunt J. Alcohol, drug intoxication, or both at the time of burn injury as a predictor of complications and mortality in hospitalized patients with burns. J Burn Care Res. 1996;17(6):532–9. doi: 10.1097/00004630-199611000-00010. [DOI] [PubMed] [Google Scholar]
- 31.Burd A. Outcome analysis of 286 severely burned patients: retrospective study. Hong Kong Med J. 2002;8(4):235–9. [PubMed] [Google Scholar]