Abstract
Introduction:
Emergency department thoracotomy (EDT) may serve as the last survival chance for patients who arrive at hospital in extremis. It is considered as an effective tool for improvement of traumatic patients’ outcome. The present study was done with the goal of assessing the outcome of patients who underwent EDT and its predictive factors.
Methods:
In the present study, medical charts of 50 retrospective and 8 prospective cases underwent emergency department thoracotomy (EDT) were reviewed during November 2011 to June 2013. Comparisons between survived and died patients were performed by Mann-Whitney U test and the predictive factors of EDT outcome were measured using multivariate logistic regression analysis. P < 0.05 considered statistically significant.
Results:
Fifty-eight cases of EDT were enrolled (86.2% male). The mean age of patients was 43.27±19.85 years with the range of 18-85. The mean time duration of CPR was recorded as 37.12±12.49 minutes. Eleven cases (19%) were alive to be transported to OR (defined as ED survived). The mean time of survival in ED survived patients was 223.5±450.8 hours. More than 24 hours survival rate (late survived) was 6.9% (4 cases). Only one case (1.7%) survived to discharge from hospital (mortality rate=98.3%). There were only a significant relation between ED survival and SBP, GCS, CPR duration, and chest trauma (p=0.04). The results demonstrated that initial SBP lower than 80 mmHg (OR=1.03, 95% CI: 1.001-1.05, p=0.04) and presence of chest trauma (OR=2.6, 95% CI: 1.75-3.16, p=0.02) were independent predictive factors of EDT mortality.
Conclusion:
The findings of the present study showed that the survival rate of trauma patients underwent EDT was 1.7%. In addition, it was defined that falling systolic blood pressure below 80 mmHg and blunt trauma of chest are independent factors that along with poor outcome.
Key Words: Thoracotomy, emergency department, cardiopulmonary resuscitation, heart arrest, outcome assessment
Introduction:
Emergency department thoracotomy (EDT) may serve as the last survival chance for patients who arrive at hospital in extremis. This method was first described in 1896 (1). The purpose of EDT is immediate access to the chest cavity to (a) release of pericardial tamponed, (b) control of cardiac and intra-thoracic haemorrhage, (c) evacuate massive air embolism, (d) open cardiac massage, and (e) place a descending thoracic aortic cross-clamp (2). EDT is considered as an effective tool for improvement of traumatic patients’ outcome (3). Two indications were defined for EDT. The first is salvageable post traumatic cardiac arrest (patients sustaining witnessed penetrating trauma with <15 minutes of pre-hospital cardio pulmonary resuscitation (CPR), or witnessed blunt trauma with <5 minutes of pre-hospital CPR) and the second relates to persistent severe post traumatic hypotension (systolic blood pressure ≤60 mmHg) due to cardiac tamponed, intra-thoracic and intra-abdominal hemorrhage, as well as cervical air embolism. There are several accessible studies during two to three decades ago which have evaluated the efficiency of EDT and predictive factors of their outcomes (3-5). The findings of these projects were variable so that some researchers believe that performing of EDT causes to increase the longevity of the person while others do not have such an idea. The trauma mechanism (blunt or penetrating), injury location, transferring time duration, etc. are predictive factors mentioned as effective agents in EDT outcomes. Studies consider a survival rate between 1.4-18 % for patients after EDT (3, 6, 7). A recent review stated the necessity of developing specific guidelines for EDT in patients benefit from this procedure. In this review, Patients most likely to benefit from EDT were those with penetrating chest trauma, signs of life at scene or on arrival in the ED or pericardial tamponed (4). Of course, the high cost of EDT performing which is paid by the patient and health care system should not be disregarded. The treatment cost for each patient is between 13000-14000 dollars, while the cost of CPR is about 892-7200 dollars (8, 9). In addition, presentation of some blood-borne diseases in staffs, ethical issues, and bad neurological outcomes are the main obstacles of EDT (10-13). Thus, the present study was done with the goal of assessing the outcome of patients who underwent EDT and its predictive factors.
Methods:
Study design and setting
In the present study, medical charts of 50 retrospective and 8 prospective cases underwent emergency department thoracotomy (EDT) were reviewed to evaluate the outcome of EDT at Shahid Rajaee trauma center, Shiraz, Iran during November 2011 to June 2013. The study protocol was not interfere to the standard treatment and approved with local Ethic Committee.
Participants
All Cases performed emergency thoracotomies at ED were included while all operation room (OR) thoracotomies excluded (except for OR thoracotomies that were done following EDT). It was considered that a minimum sample size with 44 patients could be appropriate to evaluate EDT outcomes, based on 1.5% of the survival rate (14), α=0.05, power of 90% (β=0.1), and 0.3 error.
Data collection
Thoracotomies were performed by a general surgery senior resident or a general surgeon. EDT included a left anterolateral thoracotomy, pericardiotomy, open cardiac massage, and descending thoracic aorta clamping. Those who survived, had emergency OR thoracotomies. Information about patient’s age and sex, type of injury (blunt, penetrating), arrival vital signs such as systolic blood pressure (SBP), heart rate (HR), respiratory rate (RR), Glasgow Coma Scale (GCS), venous blood gas parameters (VBG), transfused packed red blood cells, insertion of central venous line (CVL), focused abdominal ultrasonography for trauma (FAST), chest x-ray (CXR), pelvic x-ray, deep peritoneal aspiration (DPA), EDT indications, and results were gathered.
Outcome
The early survivors was defined as those who survived to be transferred to operation room (OR) and late survivors as those who survived ≥ 24hours at Intensive care unit (ICU).
Statistical analysis
Data were analyzed by STATA version 11.0. Survival rate was defined as frequency and percentage. Comparisons between survived and died patients were performed by Mann-Whitney U test. Finally, for determining the predictive factors of EDT outcome multivariate logistic regression analysis was used. P < 0.05 considered statistically significant.
Results:
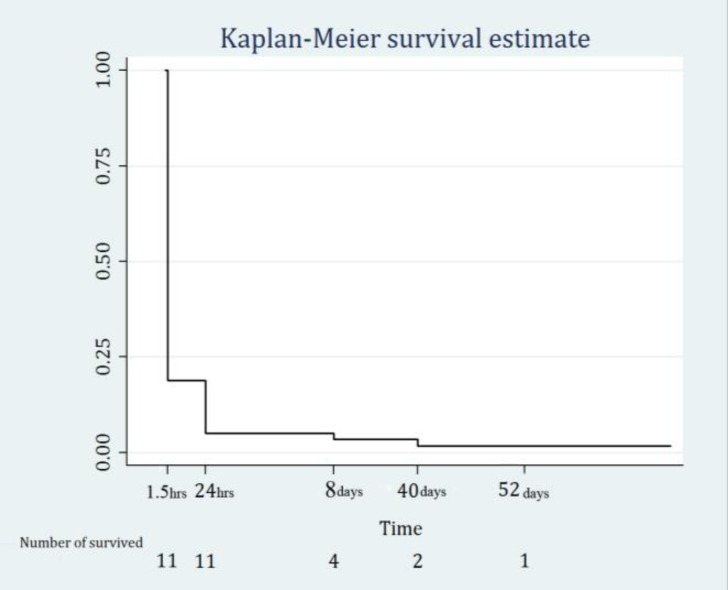
In this study, 58 cases underwent EDT following multiple trauma (94.8% blunt trauma) were examined. Table 1 shows the demographic and baseline characteristics of studied patients. The mean age of patients was 43.27±19.85 years with the range of 18-85 (86.2% male). The mean of SBP, HR, and RR on arrival to the ED were 62.10±45.12 mmHg, 83.31±50.24/minute (no detectable to 170), and 13.60±12.63/minute (no detectable to 47), respectively. In addition, the mean GCS of patients on arrival was 6.81±4.62. The mean interval time between ED arrival and EDT performance was 42.12±67.50 minutes (0-429). The mean time duration of CPR was recorded as 37.12±12.49 minutes. Eleven cases (19%) were alive to be transported to OR (defined as ED survived). Table 1 shows the demographic and baseline characteristics of ED survived patients. The mean time of survival in ED survived patients was 223.5±450.8 hours. Table 2 summarizes the diagnostic and therapeutic interventions during EDT. More than 24 hours survival rate (late survived) was 6.9% (4 cases). Only one case (1.7%) survived to discharge from hospital (mortality rate=98.3%) (Figure 1). Among different variables including age (p=0.3), sex (p=0.6), type of trauma (p=0.8), associated injuries (p>0.05), SBP (p=0.01), HR (p=0.09), RR (p=0.04), GCS (p=0.02), VBG parameters (p>0.05), FAST results (p=0.26), DPA results (0.67), EDT indication (0.38), and duration of CPR (p=0.04) there were only a significant relation between ED survival and SBP, GCS, CPR duration, and chest trauma (p=0.04). Table 3 shows the results of multivariate logistic regression analysis. The results demonstrated that initial SBP lower than 80 mmHg (OR=1.03, 95% CI: 1.001-1.05, p=0.04) and presence of chest trauma (OR=2.6, 95% CI: 1.75-3.16, p=0.02) were independent predictive factors of EDT mortality.
Table 1.
Demographic and baseline characteristics of studied patients
| Variable |
Total
N (%) |
ED survived
N (%) |
|---|---|---|
| Age | ||
| 18-29 | 21 (36.2) | 3 (27.3) |
| 30-44 | 13 (22.4) | 2 (18.2) |
| 45-59 | 9 (15.5) | 1 (9.1) |
| >60 | 15 (25.9) | 5 (45.4) |
| Gender | ||
| Male | 50 (86.2) | 10 (90.9) |
| Female | 8 (13.8) | 1 (9.1) |
| Type of trauma | ||
| Car to car accident | 11 (19.0) | 2 (18.2) |
| Car to pedestrian | 21 (36.2) | 3 (27.3) |
| Car turn over | 6 (10.3) | 2 (18.2) |
| Motor to car accident | 9 (15.5) | 1 (9.1) |
| Motor turn over | 2 (3.45) | 1 (9.1) |
| Fall | 4 (6.9) | 1 (9.1) |
| Gun Shot | 3 (5.2) | 1 (9.1) |
| Other | 2 (3.45) | 0 (0) |
| Associated injuries | ||
| Pericardial tamponade | 3 (5.2) | 1 (9.1) |
| Rib fracture | 10 (17.2) | 1 (9.1) |
| Hemothorax | 50 (86.2) | 1 (9.1) |
| Great vessels injury | 3 (5.2) | 1 (9.1) |
| Lung injury | 4 (6.9) | 0 (0) |
| Cardiac injury | 2 (3.4) | 1 (9.1) |
| Head trauma | 34 (58.6) | 5 (15.4) |
| Abdominal trauma | 11 (19) | 3 (27.3) |
| Extremities trauma | 24 (41.4) | 5 (15.4) |
| EDT indication | ||
| Cardiac arrest | 28 (48.2) | 7 (63.6) |
| Shock | 30 (51.8) | 4 (36.4) |
| Shock index | ||
| >0.8 | 50 (86.2) | 10 (90.9) |
| <=0.8 | 8 (13.8) | 1 (9.1) |
Table 2.
Diagnostic and therapeutic interventions during emergency department thoracotomy
| Interventions | Total n (%) | ED survived n (%) |
|---|---|---|
| Pack cell | 48 (82.8) | 10 (90.9) |
| Chest tube | 32 (55.2) | 6 (54.6) |
| Central venous line | 41 (70.7) | 11 (100) |
| Chest x-ray | 18 (31.3) | 5 (45.4) |
| Pelvic x-ray | 3 (5.2) | 1 (9.1) |
| FAST | ||
| Positive | 12 (34.3) | 4 (50.0) |
| Negative | 23 (65.7) | 4 (50.0) |
| Deep peritoneal lavage | ||
| Positive | 15 (39.5) | 3 (33.3) |
| Negative | 23 (60.5) | 6 (66.6) |
Focused abdominal ultrasonography for trauma.
Figure 1.
Survival estimation of EDT patients
Table 3.
The results of multivariate logistic regression analysis regarding the predictive factors of outcome
| Factors | Odds ratio | 95% confidence interval | P value |
|---|---|---|---|
| Systolic blood pressure | 1.03 | 1.001-1.05 | 0.04 |
| Blunt chest trauma | 2.6 | 1.75-3.16 | 0.02 |
Discussion:
The findings of the present study showed that the rate of final survival of trauma patients underwent EDT was 1.7%. In addition, it was defined that falling systolic blood pressure below 80 mmHg and blunt trauma of chest are independent factors that along with poor outcome. Based on trauma guidelines, thoracotomy in patients with penetrating injuries, those who have vital signs, and referring to the ED within the first 15 minutes after injury have appropriate outcomes (5). However, some researchers believe that EDT performing in patients with blunt trauma and ischemia can be helpful (15, 16). The present findings are compatible with previous studies. It is probable that blood pressure over 80 mmHg be representative of less duration from the initial injury. Because in initial steps of damage compensatory mechanisms are performed and try to keep blood pressure in the normal range. However, in case of patient deterioration, these mechanisms cannot maintain the homeostasis and this gradually leads to disappear the vital signs of the patient. As a result, although in this study the time interval between the occurrence of the event and EDT performing didn’t have any effect on the patients’ outcome, because of affecting the level of blood pressure, it can be stated that patients referred sooner to the ED have more survival chance. One of the reasons that this time interval had no effect on patients’ outcome was that recording the times of rate in their study population, while Boyd et al. had 7% (10, 17). In a review of 463 cases, Lorenz et al. events, ambulance arrival, and EDT performing were not accurate and consequently their findings were not reliable. Passos et al. studies revealed that lots of ischemia times were not accurately recorded and thus evaluation of time interval between ischemia and EDT performing was not accessible (17). On-arrival systolic blood pressure significantly correlated with those who reached OR. It seems that systolic blood pressure on presentation could be considered as predictive factor in both early and late survivors. Wyrick et al. found that the absence of on-arrival signs of life could be a predictive factor among their early mortality group (18). In addition, profound (blood pressure <60mmHg) and mild shock (blood pressure 60-90 mmHg) were associated with survival rates of 56% and 64%, respectively in cases with penetrating cardiac trauma and resultant cardiac arrest in one study (8). Millham et al. declared that EDT survivors had a detectable pulse or blood pressure either in pre-hospital or on presentation to ED (7). In comparison with some studies, we had a nearly similar outcomes based on cases who were alive and transported to OR. Considering to 98.3% mortality rate for cases in this study and the fact that the majority of them sustained blunt trauma, it was suggested that EDT for cases of blunt trauma should be meticulously selected. As mentioned before, only one survivor was discharged (1.7%). Rhee et al. in a study of cases underwent EDT over 25 years, reported an overall survival rate of 7.4% (19). Champion et al. displayed 11 % survival. found 13% of overall survival rate (20). The major cause of such discrepancy arises from the types of injuries which was studied; so that in the present project, 55 (94.8%) of patients suffered from blunt trauma. In the text review, also when the findings limited to EDTs, which were performed in blunt trauma, the survival rate of patients has been noticeably decreased. For example, Brown et al. reported no survivor among their 11 blunt trauma cases (16). Others found blunt trauma cases survival rates of 0% (10, 12), 0.6% (11), 2% (8),6% (5), and 12.5% (15). Tan et al. reported 8 (12%) neurologically intact blunt trauma survivors (4). Balkan et al. revealed six patients who underwent EDT for blunt cardiac trauma and (one case) 16.7% survival rate (12). Capote et al. found 93% mortality rate for blunt trauma cases (8). Also, Champion et al. reported five patients survived to operation room with three cases who died in OR and two ones expired on fifth postoperative day (in addition to their ten cases discharged) (20). Thirty-three cases of Mollberg et al. study (27.5%) survived to reach OR, while seven (5.8%) survived to discharge (12). The current study in comparison with the previously mentioned studies, had eleven cases (19%) were referred to operation room and four (6.9%) survived OR to reach ICU and one (1.7%) survived to discharge. Despite of EDT advantages, the costs and risks associated with indiscriminate performance of EDT is high. Several study have demonstrated that EDT is correlated with increased risk of exposure to blood-borne pathogens and permanent neurologic impairment (3, 6). Also, some studies have revealed (21, 22). Recently, Seamon et al. reported that 74% of survived patients had long-term social, cognitive, functional, or psychological impairment after EDT (3). Noticing to different ideas about the resultants of EDT, a definitive comment regarding its performing on different patients is dependent on more studies. One of the important aspects, which should be considered in future studies, is categorizing the patients in terms of clinical factors such as trauma mechanism.
Conclusion:
The findings of the present study showed that the survival rate of trauma patients underwent EDT was 1.7%. In addition, it was defined that falling systolic blood pressure below 80 mmHg and blunt trauma of chest are independent factors that along with poor outcome.
Acknowledgments:
The authors kindly appreciate the staffs of the trauma center of Shahid Rajaei hospital, Shiraz, Iran.
Conflict of interest:
None
Funding support:
None
Authors’ contributions:
All authors passed four criteria for authorship contribution based on recommendations of the International Committee of Medical Journal Editors.
References
- 1.Flynn TC, Ward RE, Miller PW. Emergency department thoracotomy. Ann Emerg Med. 1982;11(8):413–6. doi: 10.1016/s0196-0644(82)80037-1. [DOI] [PubMed] [Google Scholar]
- 2.Sersar SI, AlAnwar MA. Emergency thoracotomies: Two center study. J Emerg Trauma Shock. 2013;6(1):11–5. doi: 10.4103/0974-2700.106319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seamon MJ, Chovanes J, Fox N, et al. The use of emergency department thoracotomy for traumatic cardiopulmonary arrest. Injury. 2012;43(9):1355–61. doi: 10.1016/j.injury.2012.04.011. [DOI] [PubMed] [Google Scholar]
- 4.Tan B, Pothiawala S, Ong M. Emergency thoracotomy: a review of its role in severe chest trauma. Minerva Chir. 2013;68(3):241–50. [PubMed] [Google Scholar]
- 5.Cothren CC, Moore EE. Emergency department thoracotomy for the critically injured patient: Objectives, indications, and outcomes. World J Emerg Surg. 2006;1(1):4. doi: 10.1186/1749-7922-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lorenz HP, Steinmetz B, Lieberman J, Schecter WP, Macho JR. Emergency thoracotomy: survival correlates with physiologic status. J Trauma. 1992;32(6):780–8. doi: 10.1097/00005373-199206000-00020. [DOI] [PubMed] [Google Scholar]
- 7.Millham FH, Grindlinger GA. Survival determinants in patients undergoing emergency room thoracotomy for penetrating chest injury. J Trauma. 1993;34(3):332–6. doi: 10.1097/00005373-199303000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Rhee PM, Acosta J, Bridgeman A, Wang D, Jordan M, Rich N. Survival after emergency department thoracotomy: review of published data from the past 25 years. J Am Coll Surg. 2000;190(3):288–98. doi: 10.1016/s1072-7515(99)00233-1. [DOI] [PubMed] [Google Scholar]
- 9.Rabinovici R, Bugaev N. Resuscitative Thoracotomy: An Update. Scand J Surg. 2014;103(2):112–9. doi: 10.1177/1457496913514735. [DOI] [PubMed] [Google Scholar]
- 10.Burlew CC, Moore EE. Initial Trauma Management, Resuscitative Thoracotomy. Encyclopedia Intensive Care Med. 2012:1238–44. [Google Scholar]
- 11.Khorsandi M, Skouras C, Shah R. Is there any role for resuscitative emergency department thoracotomy in blunt trauma? Interact Cardiovasc Thorac Surg. 16(4):509–16. doi: 10.1093/icvts/ivs540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mollberg NM, Glenn C, John J, et al. Appropriate use of emergency department thoracotomy: implications for the thoracic surgeon. Ann Thorac Surg. 2011;92(2):455–61. doi: 10.1016/j.athoracsur.2011.04.042. [DOI] [PubMed] [Google Scholar]
- 13.Powell DW, Moore EE, Cothren CC, et al. Is emergency department resuscitative thoracotomy futile care for the critically injured patient requiring prehospital cardiopulmonary resuscitation? . J Am Coll Surg. 2004;199(2):211–5. doi: 10.1016/j.jamcollsurg.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 14.Vassiliu P, Yilmaz T, Degiannis E. On the Ideal Emergency Thoracotomy Incision. World J Surg. 2014;38(4):1001–2. doi: 10.1007/s00268-013-2253-9. [DOI] [PubMed] [Google Scholar]
- 15.Thomas MO, Ogunleye EO. Emergency Thoracotomy: Indications and Management Challenges in a Developing World. World J Cardiovasc Surg. 2012;2:1. [Google Scholar]
- 16.Brown SE, Gomez GA, Jacobson LE, Scherer 3rd T, McMillan RA. Penetrating chest trauma: should indications for emergency room thoracotomy be limited? Am Surg. 1996;62(7):530–3. [PubMed] [Google Scholar]
- 17.Passos EM, Engels PT, Doyle JD, et al. Societal costs of inappropriate emergency department thoracotomy. J Am Coll Surg. 2012;214(1):18–25. doi: 10.1016/j.jamcollsurg.2011.09.020. [DOI] [PubMed] [Google Scholar]
- 18.Wyrick DL, Dassinger MS, Bozeman AP, Porter A, Maxson RT. Hemodynamic variables predict outcome of emergency thoracotomy in the pediatric trauma population. J Pediatr Surg. 2014 doi: 10.1016/j.jpedsurg.2014.03.020. [In press] [DOI] [PubMed] [Google Scholar]
- 19.Mazzorana V, Smith RS, Morabito DJ, Brar HS. Limited utility of emergency department thoracotomy. The American surgeon. 1994;60(7):516–20. [PubMed] [Google Scholar]
- 20.Champion J, McKernan J. Comparison of minimally invasive thoracoscopy versus open thoracotomy for staging lung cancer. Int Surg. 1995;81(3):235–6. [PubMed] [Google Scholar]
- 21.Velmahos GC, Degiannis E, Souter I, Allwood AC, Saadia R. Outcome of a strict policy on emergency department thoracotomies. Arch Surg. 1995;130(7):774–7. doi: 10.1001/archsurg.1995.01430070096019. [DOI] [PubMed] [Google Scholar]
- 22.Keller D, Kulp H, Maher Z, Santora TA, Goldberg AJ, Seamon MJ. Life after near death: Long-term outcomes of emergency department thoracotomy survivors. Journal of Trauma and Acute Care Surgery. 2013;74(5):1315–20. doi: 10.1097/TA.0b013e31828c3db4. [DOI] [PubMed] [Google Scholar]