Abstract
More than 40,000 species of spiders have been identified in the world. Spider bites is a common problem among people, however few of them are harmful but delay in treatment can cause death. Since the spider bites are risk full to human, they should be taken seriously, especially in endemic areas. Our objective in this review was to study about poisonous spiders and find out treatments of them. Therefore, we collected related articles from PubMed database and Google Scholar. Three important syndromes caused by spider bites are loxoscelism, latrodectism and funnel web spider syndrome. Many treatments are used but much more studies should have done to decrease the mortality. In this review, we describes different venomous spiders according to their appearance, symptoms after their bites and available treatments.
Key Words: Spiders, spider bites, spider venoms, black widow spider, emergency treatment
Introduction:
Spiders belong to a branch of invertebrate animals called arthropods. Arthropods have the largest number of species. Along with ticks, mites and scorpions, spiders fall into the subphylum chelicerata and class of arachnids (1, 2). The arachnid class has very diverse members in a way that more than 80,000 species belonging to that class have been identified to date. Spiders are a large group of arachnids belonging to the araneae order (1). More than 40,000 species of spider have been identified to date but the real number is estimated at 4 times more than that number (3). Except for two small groups in the arachnid family, all spiders have poison glands and release their secretions into their venom sacs near their chelicerae. However, the majority of spiders do not bite humans and except for a few cases, they are not harmful to the human being or other mammals (2).Spider bites are common but the majority of species create little clinical presentations (3). There is only one aggressive spider named funnel-web in Australia, which attacks the human being without provocation. The majority of venomous spiders are found in Latin America. These large spiders are quite aggressive and their venom is pharmacologically highly toxic. Their bite results in severe pain, neurotoxic effects, diaphoresis, severe allergic reaction and priapism (1). Other spiders normally exhibit aggressive behavior after being trapped, injured or provoked. The severity of reactions to spider venom depends on factors such as its amount, site of biting and its duration and age and health condition. Mortality due to spider bite is rare (2). Spider venom includes different peptides and substances affecting sodium, calcium and potassium channels in neurons and also glutamate and acetylcholine receptors (4).Spider bite victims develop symptoms such as pain and swelling in the site of biting, necrosis, pyrexia, pulmonary edema, respiratory distress, hypertension, kidney dysfunction and death. Treatment protocol in the case of critically ill patients includes supportive measures and antivenom injection. Respiratory support and monitoring the hemodynamic status of these patients are of fundamental importance (5). Highly venomous spiders, funnel-web in Australia and armadeiras (armed spiders) in South America require antivenom and intensive therapeutic interventions (6). Three important syndromes are caused by spider bites: latrodectism, loxoscelism, and funnel-web spider syndrome (7). Here, we discuss about poisonous spiders and find out treatments of them.
Introduction of venomous spiders
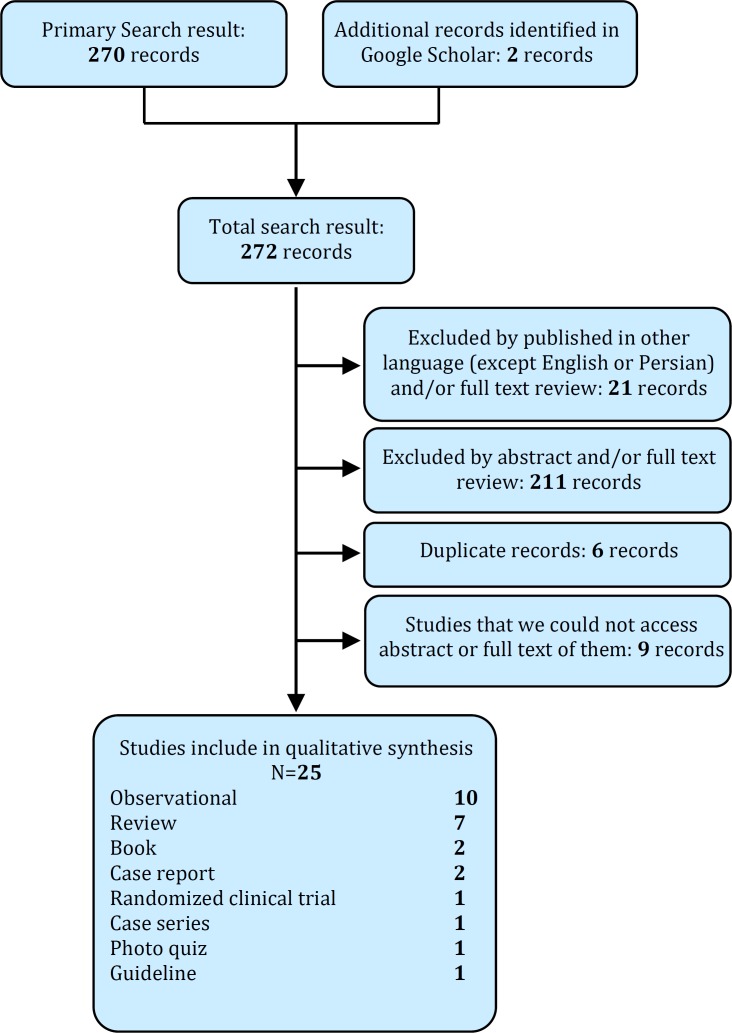
This section describes different venomous spiders according to their appearance, symptoms after their bites and available treatments. Therefore, we collected related articles from PubMed and Google scholar (Figure 1).
Figure 1.
Flowchart of study
a) The brown recluse spider
The brown recluse spider is recognized by the violin-shaped marking on its back (Figure 2). This spider takes rest during the day and is not aggressive but it will attack in the case of provocation. Patients are usually bitten by wearing clothes and shoes with spiders in them (2).
Figure 2.
Brown Recluse Spider. Photograph by Richard S.Vetter.Reproduced with permission from:australianmuseum.net.au
Loxoscelism syndrome is the symptoms caused by the bite of the brown recluse spider. This spider's bite is usually painless but it later becomes an inflammatory, hemorrhagic and painful lesion (8). Necrosis spreads a few days following the bite and loxoscelism syndrome results in dermatitis necrosis in the site of biting, around which becomes red, white and blue, respectively (9). The venom of this spider contains hyaluronidase and sphingomyelinase D enzymes and results in necrosis. Moreover, neutrophil activity and platelet aggregation and thrombosis exacerbate necrosis (8). Local manifestations of the bite of this spider include edema, inflammation, hemorrhage, damage to the vessel wall, thrombosis, and necrosis (10) but systematic symptoms including acute renal failure, rhabdomyolysis and intravascular hemolysis have also been reported (11). In some cases, severe coagulopathy can result in stroke (7).Considering extensive differential diagnosis for skin necrosis, the standard criteria for the diagnosis of loxoscelism syndrome is capturing the spider during biting or capturing it in the place where biting occurred and its confirmation by a reliable arachnologist(12).
Dapsone, antihistamines, colchicine, corticosteroids and hyperbaric oxygen have been used for treatment. Treatment with dapsone can alleviate bite marks and symptoms (8, 13). Antivenom reduces the size of the necrotic area. The faster the antivenom is administered, the less the manifestations. It has been proven useful during the first 4 hours after the bite but according to an investigation, it was useful even after 12 hours (14).
The bite-induced necrosis spreads in a few days and completes in a few weeks. Treatments include initial debridement and in later stages, after improvement of the inflammation, graft is used in case of severity (9).
b) Hobo spider
Hobo spider is a brown-colored spider with gray marks along its body (Figure 3). The reason for its name is its aggressive behavior following slight provocation. Symptoms induced by its bite are similar to those of the brown recluse spider but necrosis is rare and permanent scar is probable on the site of biting (12). The cause of necrosis is the hemolytic property of the venom or transmission of pathogenic bacteria inside the site of biting (15). The systemic symptoms of biting are reportedly cephalalgia and in some, rare cases anaphylaxis and death. The treatment is similar to that of the brown recluse spider. Moreover, resection should not be conducted before the completion of the necrosis process (8).
Figure 3.
Eratigena-Agrestis (Hobo) Spider. Reproduced with permission from:www.spiders.us
c) Black widow spider
Black widow spiders have a black hairless body. Males are smaller than females. Its major characteristic is a red marking on its abdomen similar to an hourglass (Figure 4). It is not aggressive under normal circumstances but attacks if disturbed, especially while protecting its egg sacs. Moreover, it is the most important venomous spider in North America and Australia (2, 3). Its venom is alpha-latrotoxin (neurotoxic venom) which results in the exocytosis of synaptic vesicles from parasympathetic terminals due to the stimulation of calcium-dependent mechanisms, releasing catecholamines and acetylcholine (8).
Figure 4.
Black Widow Spider (Photograph by Eric R. Eaton. Reproduced with permission from bugeric.blogspot.com
The symptoms induced by the bite of this spider are called latrodectism. The pain from its bite is similar to that of a pinprick. A lesion similar to the target lesion can be observed in the site of biting (16).Latrodectism starts in a few minutes with the development of pain through the whole body and symptoms such as emesis, respiratory failure, delirium, partial paralysis of limbs, abdominal muscle cramps, hypertension, pyrexia, fasciculation and muscle spasm are developed within a few hours (17). Symptoms may be mistaken with acute abdomen. Mortality following biting is less than 1 % and the risk of death following biting is high in two age spectrums. Bites usually occur during warm months (7). The chelicerae of this spider rarely leave a mark. Following the bite, erythema, diaphoresis and piloerection are observed around the site of bite in 25 % of the cases (3). Diagnosis is based on the patient's history. While it can be difficult in children, hypertension, distress, diaphoresis and irritability can suggest diagnosis in these cases (18).
The treatment of these patients consists of using muscle relaxants, narcotics, analgesics, intravenous calcium and antivenom. Narcotics and benzodiazepines relieve muscle spasms. Antivenom treatment is recommended for children, pregnant women the elderly and also patients with severe local symptoms, severe pains necessitating repeated administration of narcotics and systematic symptoms (3). In the case of IV administration, the antivenom should be diluted and injected slowly (17). However, some centers have recommended IM administration in order to reduce its complications. In the case of IM administration, the effect is delayed and symptoms take longer to improve (3) (within 1-5 days). Some may suffer from chronic pains even after proper antivenom treatment (18).
d) Armadeiras (armed spiders)
Armed spiders have long arms. Since they often hide in banana boxes, they are known as banana bunch spiders by locals (Figure 5).The symptom of its bite is severe pain which is observed in 96 % of patients (18). The bite of this spider can cause respiratory failure and death at both ends of the age spectrum (8). Its venom is neurotoxic thus stimulates the autonomic nervous system (tachycardia, hypertension, diaphoresis and salivation), priapism, dizziness and visual disturbances (19). This venom is recommended to be used for controlling permanent pathological pains due to its different compounds and its effect on pain neurons (20).
Figure 5.
Phoneutria, commonly known as Brazilian wandering spider or armed spider. Image source:wikipedia.org
Patients receive supportive treatment including pain and symptom control. There is antivenom for the treatment of these patients but it is used in few cases (21). With regard to the probability of respiratory failure in these patients, it is contradictory to use narcotics for pain control. Therefore, local nerve block anesthesia is recommended (8).
e) Funnel-web spider
Funnel-web spider, the most dangerous spider in the world, is aggressive in the absence of provocation (Figure 6) (3). The structure of this spider’s web is funnel-shaped, hence the name (8).The venom of this spider is neurotoxin and contains a large amount of peptides (22, 23). Delta atracotoxin, one of the peptides in the venom, delay the activation of voltage-dependent sodium channels resulting in repeated stimulation and release of massive neurotransmitters in nerve endings (24). Robustoxin is another toxin in the venom of this spider which is a fatal peptide and can be used for immunization (25).
Figure 6.
Funnel Web Spider (Reproduced with permission from australianmuseum.net.au
Local symptoms include pain, diaphoresis, hives and piloerection. Systemic symptoms include stimulation of the parasympathetic system (nausea, emesis, salivation, sialorrhea and tearing), cardiovascular system (hypertension, mostly tachycardia and in some rare cases bradycardia and hypotension), nervous system (fasciculation and perioral paresthesia), non-cardiac pulmonary edema (more prevalent in children), agitation, and cephalalgia(3).
Treatment includes supportive measures, elastic bandage for blocking lymph flow, limb immobilization and rapid transportation to the hospital. Antivenom is the definite cure and should be administered up to 15 minutes after opening the bandage. In the case of uncertainty about the bite and exhibition of the first systemic symptoms, 2 vials of antivenom are administered and in the case of severe symptoms 4 vials are administered. Other therapeutic measures include hemodynamic support, ventilatory support and the administration of tetanus vaccine. These measures reduce the risk of neurological complications and mortality and improve the performance of patients after being discharged (7).
f) Tarantula
Tarantula is recognized by its hairy 3-inch brown or black colored body (Figure 7). This type of spider is kept as pet (8). Its venom is not dangerous for the human being and merely creates lesions without any specific systemic reaction except for pyrexia. Tarantula’s defense mechanism is the hair on its body which stands out and moves when alarmed (2). If these hairs enter the eye, they can result in the inflammation of all of the layers of the eye. Eye wash and topical corticosteroids are recommended in the case of uveitis (8).
Figure 7.
Tarantula Spider (Mexican Red Legged Tarantula) Photograph byRicBolzan. Reproduced with permission fromaustralianmuseum.net.au
Recommendations for future
The human being has always been frightened of spiders but few of them are venomous and thus real threat to human health. However, since venomous spiders are sometimes fatal, bites should be taken care of. Moreover, it is recommended to be adequately familiar with necessary treatments. With regard to the identification of venomous spiders in our country including widow spider, which exists in the majority of provinces, healthcare personnel must be familiar with the symptoms of the bites of venomous spiders and it is essential to prepare antivenoms in the country for the treatment of spider bites. Finally, further domestic investigations are necessary on the distribution of venomous spiders and suspected cases of spider bite should be reported to related centers to reduce the damages caused by biting.
Acknowledgments:
We acknowledge Managers of www.spiders.us; www.australianmuseum.net.au; www.bugeric.blogspot.com; and www.wikipedia.org sites for let us to use their own images.
Conflict of interest:
None
Funding support:
None
Authors’ contributions:
All authors passed four criteria for authorship contribution based on recommendations of the International Committee of Medical Journal Editors.
References
- 1.Hickman C, Roberts L, Keen S, Larson A, I’Anson H, Eisenh-our D. Integrated principles of zoology. 14 ed. China: McGraw-Hill; 2008. pp. 402–12. [Google Scholar]
- 2.Diaz JH, Leblanc KE. Common spider bites. Am Fam Physician. 2007;75(6):869–73. [PubMed] [Google Scholar]
- 3.Braitberg G, Segal L. Spider bites: assessment and manage-ment. Aust Fam Physician. 2009;38(11):862–7. [PubMed] [Google Scholar]
- 4.Rajendra W, Armugam A, Jeyaseelan K. Toxins in anti-noci-ception and anti-inflammation. Toxicon. 2004;44(1):1–17. doi: 10.1016/j.toxicon.2004.04.014. [DOI] [PubMed] [Google Scholar]
- 5.Ahmed KZ, Bushra R. Antivenom therapy of spider bite en-venomation. Pak J Pharmacol. 2008;25(2):39–45. [Google Scholar]
- 6.Vetter RS, Isbister GK. Medical aspects of spider bites. Annu Rev Entomol. 2008;53:409–29. doi: 10.1146/annurev.ento.53.103106.093503. [DOI] [PubMed] [Google Scholar]
- 7.Garcia H, Tanowitz H, Del Brutto O. In: Neurological effects of venomous bites and stings: snakes, spiders, and scorpions. Neuroparasitology and Tropical Neurology: Handbook of Clin-ical Neurology Series. Aminoff, Boller, Swaab., editor. 2013. pp. 349–68. [DOI] [PubMed] [Google Scholar]
- 8.Tintinalli JE, Stapczynski JS, Ma OJ, Cline D, Cydulka R, Meckler G. Tintinalli's emergency medicine: a comprehensive study guide. McGraw-Hill Medical; 2011. pp. 1344–54. [Google Scholar]
- 9.Garza Ocañas L, Mifuji RM. Cutaneous Loxoscelism. N Engl J Med. 2013;369(5):495–500. doi: 10.1056/NEJMicm1212607. [DOI] [PubMed] [Google Scholar]
- 10.Isbister GK, Fan HW. Spider bite. The Lancet. 2011;378(9808):2039–47. doi: 10.1016/S0140-6736(10)62230-1. [DOI] [PubMed] [Google Scholar]
- 11.Malaque C, Santoro ML, Cardoso JLC, et al. Clinical picture and laboratorial evaluation in human loxoscelism. Toxicon. 2011;58(8):664–71. doi: 10.1016/j.toxicon.2011.09.011. [DOI] [PubMed] [Google Scholar]
- 12.Bennett RG, Vetter RS. An approach to spider bites. Erroneous attribution of dermonecrotic lesions to brown recluse or hobo spider bites in Canada. Can Fam Physician. 2004;50(8):1098–101. [PMC free article] [PubMed] [Google Scholar]
- 13.Bogdán S, Barabás J, Zacher G, et al. Total upper lip necrosis and loxoscelism caused by violin spider bite. Orv Hetil. 2005;146(45):2317–21. [PubMed] [Google Scholar]
- 14.Pauli I, Minozzo JC, Henrique da Silva P, Chaim OM, Veiga SS. Analysis of therapeutic benefits of antivenin at different time intervals after experimental envenomation in rabbits by venom of the brown spider (Loxosceles intermedia) Toxicon. 2009;53(6):660–71. doi: 10.1016/j.toxicon.2009.01.033. [DOI] [PubMed] [Google Scholar]
- 15.Gaver-Wainwright MM, Zack RS, Foradori MJ, Lavine LC. Misdiagnosis of spider bites: bacterial associates, mechanical pathogen transfer, and hemolytic potential of venom from the hobo spider, Tegenaria agrestis (Araneae: Agelenidae) J Med Entomol. 2011;48(2):382–8. doi: 10.1603/me09224. [DOI] [PubMed] [Google Scholar]
- 16.Shlamovitz GZ. Man With Back Pain. Ann Emerg Med. 2011;58(5):496–500. doi: 10.1016/j.annemergmed.2011.03.057. [DOI] [PubMed] [Google Scholar]
- 17.Nordt SP, Clark RF, Lee A, Berk K, Lee Cantrell F. Examin-ation of adverse events following black widow antivenom use in california. Clin Toxicol. 2012;50(1):70–3. doi: 10.3109/15563650.2011.639714. [DOI] [PubMed] [Google Scholar]
- 18.Monte AA, Bucher-Bartelson B, Heard KJ. A US perspective of symptomatic Latrodectus spp. envenomation and treatm-ent: a national poison data system review. Ann Pharmacother. 2011;45(12):1491–8. doi: 10.1345/aph.1Q424. [DOI] [PubMed] [Google Scholar]
- 19.Gewehr C, Oliveira SM, Rossato MF, et al. Mechanisms involved in the nociception triggered by the venom of the armed spider phoneutria nigriventer. PLoS Negl Trop Dis. 2013;7(4):e2198. doi: 10.1371/journal.pntd.0002198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Souza AH, Ferreira J, Cordeiro Mdo N, et al. Analgesic effect in rodents of native and recombinant Ph alpha 1beta toxin, a high-voltage-activated calcium channel blocker isolat-ed from armed spider venom. Pain. 2008;140(1):115–26. doi: 10.1016/j.pain.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 21.Isbister GK, Graudins A, White J, Warrell D. Antivenom treatment in arachnidism: antivenoms. Clin Toxicol. 2003;41(3):291–300. doi: 10.1081/clt-120021114. [DOI] [PubMed] [Google Scholar]
- 22.Liu J, Gao J, Yun Y, Hu Z, Peng Y. Bioaccumulation of mer-cury and its effects on survival, development and web-weaving in the Funnel-Web spider agelena labyrinthica (Aran-eae: Agelenidae) Bull Environ Contam Toxicol. 2013;90(5):558–62. doi: 10.1007/s00128-013-0966-y. [DOI] [PubMed] [Google Scholar]
- 23.Palagi A, Koh J, Leblanc M, et al. Unravelling the complex venom landscapes of lethal Australian funnel-web spiders (Hexathelidae: Atracinae) using LC-MALDI-TOF mass spectr-ometry. J Proteomics. 2013;80:292–310. doi: 10.1016/j.jprot.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 24.Pineda SS, Wilson D, Mattick JS, King GF. The lethal toxin from Australian funnel-web spiders is encoded by an intronl-ess gene. PLoS One. 2012;7(8):e43699. doi: 10.1371/journal.pone.0043699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Comis A, Tyler M, Mylecharane E, Spence I, Howden M. Immunization with a synthetic robustoxin derivative lacking disulphide bridges protects against a potentially lethal chall-enge with funnel-web spider (Atrax robustus) venom. J Biosci. 2009;34(1):35–44. doi: 10.1007/s12038-009-0007-5. [DOI] [PubMed] [Google Scholar]