Abstract
Introduction:
Based on previous studies, cardiovascular diseases, traffic accidents, traumas and cancers are the most important etiology of mortalities in emergency departments (ED). However, contradictory findings have been reported in relation to mortality in emergency departments. Therefore, the present study was undertaken to evaluate the role of clinical factors in mortality among patients referring to an emergency department in a third-level hospital in Tehran, Iran.
Methods:
In the present case-control study, all the patients over 18 years of age were evaluated, referring to the ED of Imam Hossein Hospital, Tehran, Iran, from the beginning of 2009 to the end of 2010. The patients died in the ED were placed in the case group and those discharged or hospitalized in other hospital wards in the control group. Demographic data, background diseases, and the final diagnoses were recorded. Chi-squared test, multivariate logistic regression, and Pearson’s correlation coefficient were used to evaluate the relationship between the variables mentioned above and patient mortality.
Results:
2907 patients (969 (59.9% male) in the case and 1938 (62.2% male) in the control groups) were evaluated. Cardiovascular diseases (39.2%), severe traumas (18.5%), and cerebrovascular accidents (17.7%) were the most frequent etiology of patient mortality in ED. Multivariate regression analysis showed that presentation with cardiovascular complaints (OR=7.3; 95% CI: 3.5-16.1; p<0.001), a history of hypertension (OR=5.4; 95% CI: 1.2-12.3; p<0.001), severe trauma (OR=4.6; 95% CI: 2.0-13.2; p<0.001), age over 60 (OR=3.8; 95% CI: 1.8-7.8; p<0.01) and a final diagnosis of renal disease (OR=3.4; 95% CI: 2.1-6.4; p<0.001) were factors that increased the odds of mortality in patients referring to the ED. Multivariate regression analysis in patients over 60 years showed that sepsis was an independent factor increasing the risk of death (OR=2.9; 95% CI: 1.3-5.9; p=0.009). A patient’s risk of death increases with an increase in the number of risk factors in that patient (r2=0.96; p=0.02).
Conclusion:
It appears the odds of mortality in patients referring to ED with cardiovascular complaints, a history of hypertensive, severe trauma, age over 60 and a final diagnosis of renal disease are higher versus other patients. In addition, the patients’ odds of death increase with an increase in the number of risk factors. Such an increase is more noticeable at age over 60.
Key Words: Emergency department, etiology, mortality, risk factor
Introduction
Patient mortality in emergency departments (ED) is a problem which has aggravated in recent years; in this context the mortality rate has increased 26% from 1998 to 2000 in the United States (1, 2). Previous studies have shown that cardiovascular conditions, traffic accidents, traumas and cancers are the most important etiology of mortalities in ED (3). However, the etiology differs in various geographical locations (4). For example, it has been reported that 15-60% of all the mortalities in hospitals occur in ED (5, 6). Such discrepancies in reports might be attributed to the type of referred patients, crowdedness, and whether the department is an educational center or not (7-9). In recent years, several attempts have been made to identify factors responsible for patient mortality (9-13). However, the results have been contradictory in most cases, i.e. some reports suggested a phenomenon or a medical condition as a risk factor while others rejected such claims. Therefore, more studies are needed to make a true judgment about the patient mortality in ED. The present study was carried out to evaluate the role of clinical factors and variables in the mortality of patients referring to the ED of a third-level hospital through 2009-2010.
Methods
Study design and setting
In the present case-control study patients, over 18 years of age were enrolled, referred to the ED of Imam Hossein Hospital (about 6000 admission/month) in Tehran, Iran, from the beginning of 2009 to the end of 2010. The protocol of the study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences. During the study period, researchers have observed the principles of Helsinki Declaration. Before beginning the study the patients, their family members, or acquaintances signed an informed consent form. Data were collected from patient files. For those cases who had file deficiencies, data were completed and collected during follow-ups.
Subjects
Patients died in the ED through 2009-2010 were included in the case group. The subjects in the control group consisted of patients discharged from ED or hospitalized in other wards of the hospital. The patients were followed up in a week after being discharged. Exclusion criteria consisted of having no interest in taking part of the study, outpatient admission, lack of possibility to follow the patient due to dropout from the study based on personal request (the control group) or transfer to other centers, and succumbing to death before being admitted into the ED. It should be pointed out that those who died in the control group during 48 hours after decision-making process were excluded from the study. The subjects were selected using a simple sampling technique. To this purpose, at the end of each day all the patients died in the ED were listed based on files’ number of which two files were randomly selected and evaluated. For each case, two control patients were randomly selected from the discharged or hospitalized patients of the same day. The number of subjects in each group was estimated at 117 subjects at α=0.05 and β=0.1 considering the odds ratio of 3.2 for death in patients with cardiovascular conditions based on previous studies (14).
Data collection
Data were collated and recorded by a trained emergency physician. Totally, 969 deceased patients during a two-year period were evaluated in the case group and 1938 ones in the control. Demographic data (age, gender and educational status), underlying diseases (diabetes, cardiovascular conditions, hypertension, cancer, AIDS, renal, and hepatic diseases), and the final diagnoses were recorded. The diagnoses were categorized into the eight groups of cardiac conditions (ischemic cardiac diseases, acute myocardial infarction, coronary atherosclerotic diseases, and cardiac insufficiency), renal diseases (acute renal insufficiency, nephritis, etc.), trauma, cancer, sepsis, pneumonia, cerebrovascular accident and others. Trauma was divided into two groups including minor and major traumas. Minor traumas consisted of muscle and tendon strains, sprains, and joint injuries; major traumas contained spinal cord injuries, intracranial injuries, penetrating abdominal injuries, blunt hemorrhagic abdominal injuries, and major chest injuries. Other conditions consisted of all the other diagnoses, including syncope, infection, psychological disorders, nervous system disorders, musculoskeletal disorders, skin and connective tissue disorders, and mild traumas.
Statistical analyses
Data were analyzed with STATA 11.0 statistical software. Chi-squared test and independent t-test were used to compare qualitative and quantitative variables, respectively. Subsequently, multivariate logistic regression was performed to determine independent risk factors of mortality. The results were reported as odds ratios (OR) at a 95% confidence interval. In addition, Pearson’s correlation coefficient was used to evaluate the correlation between the number of risk factors in one patient and odds of death. Statistical significance was defined as p<0.05.
Results
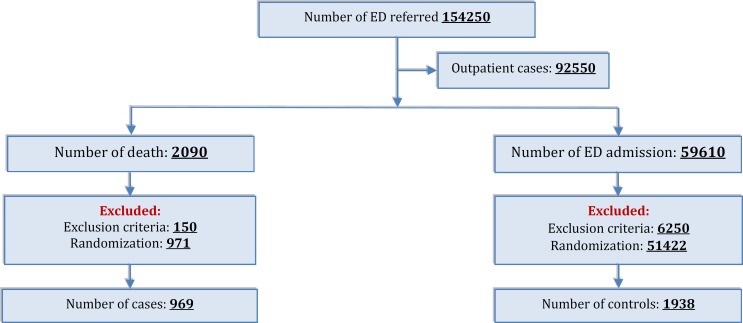
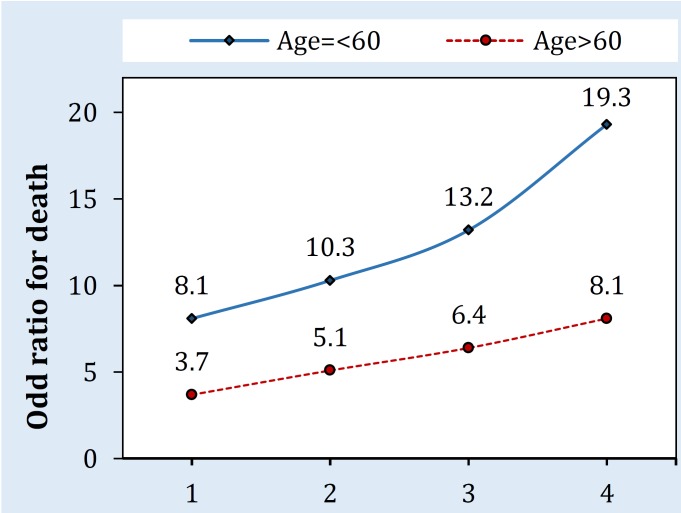
Finally, 2907 patients (969 cases and 1938 controls) were evaluated (Figure 1). The means and standard deviations of patient ages in the case and control groups were 67.4±9.6 and 46.8±11.7 years, respectively (p< 0.0001). There were 575 (59.3%) females and 1206 (62.2%) males in the case and control groups, respectively (p=0.13). In the case group, 562 (58%) patients had a history of hypertension, 251 (25.9%) cardiac diseases, 95 (9.8%) cancer, and 94 (9.7%) renal diseases. Chi-squared test showed a significant relationship between underlying diseases and mortality (Table 1). The most frequent final diagnoses in the case group consisted of cardiopulmonary diseases (39.2%), severe traumas (18.5%), cerebrovascular accident (17.7%), sepsis (13.1 %), renal diseases (3.7%), pneumonia (3.1%), and cancer (2.3%) in descending order (Table 2). Logistic regression showed that age over 60 (OR=3.8; 95% CI: 1.8-7.8; p=0.01), a history of hypertension (OR=5.4; 95% CI: 1.2-12.3; p<0.001), presentation with cardiac complaints (OR=7.3; 95% CI: 3.5-16.1; p<0.001), severe trauma (OR=4.6; 95% CI: 2.0-13.2; p<0.001), and renal diseases (OR=3.4; CI: 2.1-6.4; p<0.001) were independent factors that increased the odds of death in patients admitted into the ED. However, the odds of death were lower in patients with other diseases (OR=0.2; 95% CI: 0.06-0.9; p<0.001) (Table 3). Multivariate regression analysis of patients over 60 years showed that sepsis, as an independent factor, increased the odds of mortality in such patients (OR=2.9; 95% CI:1.3-5.9; p<0.009). Evaluation of the relationship between the presence of several risk factors in one patient and the death risk showed that the odds of death increased in an individual with the presence of several risk factors (r2=0.96; p=0.02) (Figure 2).
Figure 1.
Flowchart of patient selection
Table 1.
The separate subjects’ demographic data for the case and control groups
| Variable | Case | Control | P |
|---|---|---|---|
| Age (Mean ± SD) | |||
| Male | 69.9±10.2 | 48.2±12.5 | <0.0001 |
| Female | 64.7 ±6.8 | 45.1±11.0 | |
| Total | 67.4±9.6 | 46.8±11.7 | |
| Gender | |||
| Male | 575 (59.3) | 1206 (62.2) | 0.13 |
| Female | 394 (40.7) | 732 (37.8) | |
| Marital status | |||
| Single | 79 (87.2) | 126 (6.5) | 0.1 |
| Married | 890 (91.8) | 1812 (93.5) | |
| Educational status | |||
| < High school | 509 (52.5) | 1066 (55.0) | 0.2 |
| ≤ High school | 460 (47.5) | 870 (45.0) | |
| Underlying diseases | |||
| AIDS | 1 (0.1) | 3 (0.15) | 0.74 |
| Hepatic disease | 63 (6.5) | 192 (9.9) | 0.002 |
| Renal disease | 105 (10.8) | 238 (12.3) | 0.25 |
| Cancer | 22 (2.3) | 47 (2.4) | 0.8 |
| Cardiac disease | 251 (25.9) | 194 (10.0) | <0.0001 |
| Hypertension | 562 (58) | 341 (17.6) | <0.0001 |
| Diabetes | 166 (17.1) | 270 (13.9) | 0.02 |
Table 2.
The subjects’ final diagnosis stratifying for the case and control groups
| Disease | Case | Control | P | |
|---|---|---|---|---|
| Cardiac disease | 380 (39.2) | 215 (11.1) | <0.0001 | |
| Severe trauma | 179 (18.5) | 165 (8.5) | <0.0001 | |
| CVA | 172 (17.7) | 285 (14.7) | 0.03 | |
| Sepsis | 127 (13.1) | 296 (15.3) | 0.12 | |
| Renal disease | 36 (3.7) | 12 (0.6) | <0.0001 | |
| Pneumonia | 30 (3.1) | 44 (2.3) | 0.2 | |
| Cancer | 22 (2.3) | 47 (2.4) | 0.8 | |
| * Others | 23 (2.4) | 874 (45.1) | <0.0001 | |
Includes syncope, infections, psychological conditions, nervous system disorders, musculoskeletal diseases, skin and connective tissue conditions, and mild trauma. CVA: Cerebrovascular accident.
Table 3.
Odds ratio (OR) at a confidence interval of 95% for factors affecting patient mortality
| Factor | OR (CI: 95%) | P |
|---|---|---|
| Presentation with cardiac complaint | 7.3 (3.5-16.1) | <0.001 |
| A history of hypertension | 5.4 (1.2-12.3) | <0.001 |
| Presentation with severe trauma | 4.6 (2.0-13.2) | <0.001 |
| Age>60 | 3.8 (1.8-7.8) | 0.01 |
| A final diagnosis of renal disease | 3.4 (2.1-6.4) | <0.001 |
| Other disease* | 0.2 (0.06-0.9) | <0.001 |
Figure 2.
Association of number of risk factors and odds of death stratified by age.
Discussion:
The results of the present study showed that the odds of death in patients referring to ED with cardiac complaints, a history of hypertension, severe trauma, age over 60 and renal conditions, are higher than those in patients with other diseases. In addition, there is an increase in the odds of death with an increase in the number of risk factors. Such an increased risk is more prominent in patients over 60. Although the incidence of mortalities due to heart diseases has significantly decreased in recent years (from 64% to 49%), they still have the highest incidence rate (15, 16). The present study showed that cardiac complaints are the most important etiology of early death in patients referred to ED. Since studies have shown that the majority of deaths due to myocardial infarction take place during the first few hours after the appearance of symptoms and signs, the most important physiologic risk in cardiac patients is a delay in instituting therapeutic care. Thus, early management of such patients, especially for those who have myocardial infarction, might save their lives and decrease mortality rate. (17). Hypertension is an important and independent risk factor for patient mortality. The analyses carried out in the present study showed that the concomitant affliction with hypertension and cardiac disease increases the patient’s odds of death up to 10 times (OR=10.3; CI: 5.6-18.8; P<0.001). (18, 19). In addition, hypertension leads to cardiovascular disease; therefore, hypertension has direct effects on the mortality of patients referring to ED. It was estimated in 2004 that approximately 1 billion adults all over the world (333 million people in developed countries and 639 people in developing countries) have hypertension, 4 million of whom die due to the direct effects of hypertension (20, 21). Based on world health organization (WHO), it was estimated that high blood pressure accounts for 1 in 8 deaths and is the third killer all over the world (22). Therefore, evaluation of hypertension is of utmost importance in ED; however, in most cases, it ignored or did not pay adequate attention. In the present study, a final diagnosis of renal disease was one of the factors increasing the odds of death in patients referring to the ED. consistent with the results of previous studies it indicates a graded association between decreases in glomerular filtration rate and the risk of mortality, developing cardiovascular disease and hospitalization (23, 24). While some studies have not shown an independent effect of renal disease on increasing the risk of mortality others have reported that cardiovascular effects of renal diseases result in death (25-27). This discrepancy is attributed to the fact that renal disease can lead to cardiovascular disease (26, 28) and cardiovascular disease, in itself, can result in renal diseases (25, 28). As a result, it is not easy to make a distinction between the outcomes of these two diseases. That’s why patients with renal disease, who have cardiovascular diseases too, have more severe outcomes, including a decrease in life expectancy and an increase in the risk of mortality (29-31). In the present study, sepsis was a significant factor affecting the odds of death in patients over 60, consistent with the results of other studies in this age group (12). When the frequency of septic cases was evaluated in different age groups, it was shown that of 182 patients with sepsis in the case group, 86.3% were over 60 years; however, only 52.2% of patients in the control group were over 60.
Limitation
The study sample cannot completely reflect the situation of Iranian population and include all the ethnicities in Iran. However, based on some studies, data collected in a capital city may reflect an acceptable pattern of the whole country (32). Because the aim of the study was to evaluate the effect of clinical factors on the mortality, only clinical variables were evaluated. Therefore, it is advisable to design future studies for the evaluation of environmental, geographical and social aspects so that the effects of such factors can be analyzed, too. However, the present study was the only case-control study in the Mediterranean region to evaluate the important mortality risk factors in ED. Having a large sample size was one of the advantages of the study.
Conclusion:
It appears the odds of mortality in patients referring to ED with cardiovascular complaints, a history of hypertensive, severe trauma, age over 60 and a final diagnosis of renal disease are higher compare to other patients. In addition, the patients’ odds of death increase with an increase in the number of risk factors. Such an increase is more noticeable at age over 60.
Acknowledgments:
We acknowledge all staffs of Imam Hossein Hospital, Tehran, Iran.
Conflict of interest:
None
Funding support:
None
Authors’ contributions:
Hossein Alimohammadi, Farzaneh Mirmohammadi, and Kamran Heidari have designed the study. Farzaneh Mirmohammadi, Farahnaz Bidarizerehpoosh, and Shahram Keikha collected the data. Ali Shahrami analyzed the data. Anita Sabzghabaie wrote the first draft. All authors read and approved the final version of the manuscript.
References
- 1.Ly N, McCaig LF. National Hospital Ambulatory Medical Care Survey: 2000 outpatient department summary. Adv Data. 2002(327):1–7. [PubMed] [Google Scholar]
- 2.Olsen JC, Buenefe ML, Falco WD. Death in the emergency department. Ann Emerg Med. 1998;31(6):758–65. doi: 10.1016/s0196-0644(98)70236-7. [DOI] [PubMed] [Google Scholar]
- 3.Zheng ZJ, Croft JB, Giles WH, Mensah GA. Sudden cardiac death in the United States, 1989 to 1998. Circulation. 2001;104(18):2158–63. doi: 10.1161/hc4301.098254. [DOI] [PubMed] [Google Scholar]
- 4.Wall M, Huang J, Oswald J, McCullen D. Factors associated with reporting multiple causes of death. BMC Med Res Methodol. 2005;5(1):4–17. doi: 10.1186/1471-2288-5-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jarman B, Gault S, Alves B, et al. Explaining differences in English hospital death rates using routinely collected data. BMJ. 1999;318(7197):1515–20. doi: 10.1136/bmj.318.7197.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nelson P. Death in the Emergency Department :The Forgotten Tragedy. J Pain Symptom Manage. 2011;41(1):215–9. [Google Scholar]
- 7.Halm EA, Chassin MR. Why do hospital death rates vary? . N Engl J Med. 2001;345(9):962–4. doi: 10.1056/NEJM200108303450911. [DOI] [PubMed] [Google Scholar]
- 8.Hoot NR, Aronsky D. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52(2):126–36. doi: 10.1016/j.annemergmed.2008.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shapiro NI, Wolfe RE, Moore RB, Smith E, Burdick E, Bates DW. Mortality in Emergency Department Sepsis (MEDS) score: A prospectively derived and validated clinical prediction rule. Crit Care Med. 2003;31(3):670–5. doi: 10.1097/01.CCM.0000054867.01688.D1. [DOI] [PubMed] [Google Scholar]
- 10.Baker M, Clancy M. Can mortality rates for patients who die within the emergency department, within 30 days of discharge from the emergency department, or within 30 days of admission from the emergency department be easily measured? . Emerg Med J. 2006;23(8):601–3. doi: 10.1136/emj.2005.028134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cameron PA, Richardson DB. Increase in patient mortality at 10 days associated with emergency department overcrow-ding. Med J Aust. 2006;184(5):213–6. doi: 10.5694/j.1326-5377.2006.tb00204.x. [DOI] [PubMed] [Google Scholar]
- 12.Caterino JM, Kulchycki LK, Fischer CM, Wolfe RE, Shapiro NI. Risk factors for death in elderly emergency department patients with suspected infection. J Am Geriatr Soc. 2009;57(7):1184–90. doi: 10.1111/j.1532-5415.2009.02320.x. [DOI] [PubMed] [Google Scholar]
- 13.Salazar A, Bardés I, Juan A, Olona N, Sabido M, Corbella X. High mortality rates from medical problems of frequent emergency department users at a university hospital tertiary care centre. Eur J Emerg Med. 2005;12(1):2–5. doi: 10.1097/00063110-200502000-00002. [DOI] [PubMed] [Google Scholar]
- 14.van Dam RM, Li T, Spiegelman D, Franco OH, Hu FB. Combined impact of lifestyle factors on mortality: prospective cohort study in US women. BMJ. 2008;337:a1440. doi: 10.1136/bmj.a1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.De Vivo MJ, Stuart Krause J, Lammertse DP. Recent trends in mortality and causes of death among persons with spinal cord injury. Arch Phys Med Rehabil. 1999;80(11):1411–9. doi: 10.1016/s0003-9993(99)90252-6. [DOI] [PubMed] [Google Scholar]
- 16.Melanie W, Jinzhou H, John O, Diane MC. Factors asso-ciated with reporting multiple causes of death. BMC Med Res Methodol. 2005;5:4:4–17. doi: 10.1186/1471-2288-5-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cannon CP, Gibson CM, Lambrew CT, et al. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000;283(22):2941–7. doi: 10.1001/jama.283.22.2941. [DOI] [PubMed] [Google Scholar]
- 18.Frankel FM, Duong N, Shil AB. Association of Hypertension With Mortality. Am J Hypertens. 2010;23(5):452–3. doi: 10.1038/ajh.2010.23. [DOI] [PubMed] [Google Scholar]
- 19.Gombojav B, Yi S-W, Sull JW, Nam CM, Ohrr H. Combined effects of cognitive impairment and hypertension on total mortality in elderly people: the Kangwha Cohort study. Gerontology. 2011;57(6):490–6. doi: 10.1159/000323759. [DOI] [PubMed] [Google Scholar]
- 20.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. The Lancet. 2005;365(9455):217–23. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 21.Lawes CM, Hoorn SV, Rodgers A. Global burden of blood-pressure-related disease, 2001. The Lancet. 2008;371(9623):1513–8. doi: 10.1016/S0140-6736(08)60655-8. [DOI] [PubMed] [Google Scholar]
- 22.World Health Organization. A global brief on hypertension. Silent killer, global public health crisis. Genev: World Health Organization; 2013. [Google Scholar]
- 23.Gabayan GZ, Derose SF, Asch SM, et al. Patterns and Pred-ictors of Short-Term Death After Emergency Department Disc-harge. Ann Emerg Med. 2011;58(6):551–8. doi: 10.1016/j.annemergmed.2011.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Go AS, Chertow GM, Fan D, McCulloch CE, Hsu C. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351(13):1296–305. doi: 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 25.Ma K, Greene E, Raij L. Cardiovascular risk factors in chronic renal failure and hemodialysis populations. Am J Kidney Dis. 1992;19(6):505–11. doi: 10.1016/s0272-6386(12)80827-4. [DOI] [PubMed] [Google Scholar]
- 26.Muntner P, He J, Hamm L, Loria C, Whelton PK. Renal insufficiency and subsequent death resulting from cardiovasc-ular disease in the United States. J Am Soc Nephrol. 2002;13(3):745–53. doi: 10.1681/ASN.V133745. [DOI] [PubMed] [Google Scholar]
- 27.Sarnak MJ, Levey AS, Schoolwerth AC, et al. Kidney disease as a risk factor for development of cardiovascular disease. Circulation. 2003;108(17):2154–69. doi: 10.1161/01.CIR.0000095676.90936.80. [DOI] [PubMed] [Google Scholar]
- 28.McCullough PA, Wolyn R, Rocher LL, Levin RN, O’Neill WW. Acute renal failure after coronary intervention: inciden-ce, risk factors, and relationship to mortality. Am J Med. 1997;103(5):368–75. doi: 10.1016/s0002-9343(97)00150-2. [DOI] [PubMed] [Google Scholar]
- 29.Collins AJ, Foley RN, Herzog C, et al. US Renal Data System 2010 Annual Data Report. Am J Kidney Dis. 2011;57(1):1–9. doi: 10.1053/j.ajkd.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 30.Foley RN, Collins AJ. End-stage renal disease in the United States: an update from the United States Renal Data System. J Am Soc Nephrol. 2007;18(10):2644–8. doi: 10.1681/ASN.2007020220. [DOI] [PubMed] [Google Scholar]
- 31.Goodman WG, Goldin J, Kuizon BD, et al. Coronary-artery calcification in young adults with end-stage renal disease who are undergoing dialysis. N Engl J Med. 2000;342(20):1478–83. doi: 10.1056/NEJM200005183422003. [DOI] [PubMed] [Google Scholar]
- 32.Hosseini M, Carpenter R, Mohammad K. Growth of child-ren in Iran. Ann Hum Biol. 1998;25(3):249–61. doi: 10.1080/03014469800005612. [DOI] [PubMed] [Google Scholar]