Abstract
Introduction:
Although the synergistic effects of opioids and other analgesic drugs such as non-steroidal anti-inflammatory drugs (NSAIDs) have been established in relieving acute pain due to renal calculi, no studies today have evaluated the concomitant administration of opiates and other drugs with analgesic effects, such as serotonin re-uptake inhibitors. Considering the high prevalence of renal colic, the present study was carried out to compare the effect of concomitant prescription of morphine and a placebo with that of morphine and citalopram on the management of acute pain due to renal calculi.
Methods:
The present double-blind randomized clinical trial was carried out from October 2012 to March 2013 in the Al-Zahra educational Hospital in Isfahan, Iran. 90 patients with acute renal colic pain were randomly divided into two groups of 45 subjects. The subjects in one group received morphine/ placebo and another one morphine/citalopram. The patients’ pain severity was determined by visual analogue scale (VAS) before and 20 minutes after administration of medications. In case of persistent pain, the second or even third dose was administered and the pain severity was once again determined. Data were analyzed with STATA 11.0 using chi-squared, two-way ANOVA, Bonferroni post hoc test, and log rank test.
Results:
The decrease in pain severity in the morphine/citalopram group was significantly compared to the morphine/placebo group and the time before administration of the medications (p<0.001). In contrast, administration of morphine/placebo did not have a significant effect on pain severity at this interval (p=0.32). Kaplan-Meier curve showed that the first injection was successful in relieving pain in 15 (33.3%) and 26 (57.8%) subjects in the morphine/placebo and morphine/citalopram groups, respectively. The second injection of these medications resulted in therapeutic success in 35 (87.8%) and 42 (95.6%) subjects in the above groups, respectively. Log rank test showed a significant difference in the treatment success between the two groups (p=0.001).
Conclusion:
It seems that the combination of citalopram and morphine sulfate causes increased efficacy and higher success rate in pain control of patients presented to the emergency department with a complaint of renal colic.
Key Words: Pain management, renal colic, morphine, citalopram, emergencies
Introduction
Renal colic is usually manifested clinically as a very painful and troublesome condition which appears unilaterally on the flank to the groin suddenly or periodically (1, 2). The condition afflicts 5-12% of the population in industrial societies at least once in their life and its recurrence rate is approximately 50% (1). The pain is usually attributed to contraction of ureter soft muscles in response to the presence of stone (3-5). Therefore, the most important consideration in the emergency management of renal colics is pain control/relief (5, 6). Various therapeutic strategies are employed to alleviate the pain due to renal calculi and some studies have recommended the use of NSAID, especially ketorolac, as the first analgesic for renal calculi (5, 7-10). However, disadvantages such as lack of availability, high cost, the risk of gastrointestinal hemorrhage, and acute renal insufficiency have led to a greater use of opioids such as meperidine and morphine or their concomitant use in clinical settings compared to NSAIDs (1, 11, 12). On the other hand, there is an ample evidence in relation to pain relief with the use of serotonin re-uptake inhibitors such as citalopram in patients with acute and chronic renal insufficiency, in cases of visceral pain, heat sensitivity, thermal pain, peritoneal dialysis, peritonitis and neuropathic injuries (13, 14). Although the synergistic effects of opioids such as morphine and the group of analgesics such as NSAIDs have been established on relieving acute pain due to renal stones, no studies today have evaluated the effects of concomitant administration of opioids and other analgesic agents, such as serotonin re-uptake inhibitions. Therefore, the present study was undertaken to evaluate the presence or absence of synergistic or additive analgesic effect of morphine and citalopram on relieving acute renal stone pain.
Methods
Study design and setting
The present double-blind randomized clinical trial was carried out during a six-month period from October 2012 to March 2013 in the emergency department of Al-Zahra Hospital, Isfahan, Iran. The protocol of the study was prepared based on Helsinki declaration and approved by ethics committee of Isfahan University of Medical Sciences. The study was registered in Iranian registry of clinical trial (IRCT2014020812072N1). All patients signed consent form before including to the study. Participants
The subjects were patients with acute renal colic, referring to the emergency department of Al-Zahra Hospital. The inclusion criteria consisted of an age range of 18-55, a clinical diagnosis of acute colicky pain, pain severity of 7-10 based on visual analogue scale (VAS), and patients’ consent form to participate in the study. The exclusion criteria consisted of pregnancy or suspected of being pregnant, contraindication in relation to taking morphine and citalopram based on drug catalog, a history of dependence on opioids or SSRIs, receiving an analgesic during a six-hours period before presentation, peritonitis or peritoneal symptoms and signs, any disease preventing communication, and patient’s decision to leave the study.
Intervention
All the patients underwent a urine analysis and an ultrasound examination. The final diagnosis was reached in each patient based on initial clinical diagnosis using the examinations above. The patients were randomly assigned to two groups. The subjects in group one received an intravenous injection consisting of 5 mg of morphine sulfate plus placebo (normal saline with the same volume as that in group two) and subjects in group two received an intravenous injection consisting of 5 mg of morphine sulfate plus 20 mg of citalopram. During the study period, none of the patients, physicians and nurses, and the medical care team members were aware of the study procedures. Preparation and injection of medications were carried out by two nurses; the nurses prepared the medications were blind to drugs of each patient. All the syringes had the same shape. Randomization and registration of data were carried out by the chief researcher who was the only person aware of the study procedures. In order to confirm the diagnosis, all the patients were subjected to an ultrasound examination of kidneys and the urinary tract. The ultrasonography was not performed for patients with a documented history of renal calculi or patients recovering from renal calculi and referring with a similar episode. Visualization of a renal stone by a radiologist during ultrasound examination or a report of hydronephrosis on the painful side confirmed the diagnosis. Passage of stone through the urethra and direct visualization of stone confirmed the diagnosis, too. The medications were administered intravenously in the same manner for all the patients and each of them received a proper medications dose based on a timetable. Any drug side effect was managed by standard protocols of the emergency department.
Statistical analyses
The sample size in the present study was calculated at 45 subjects in each group, by considering a 95% confidence interval, an 80% power of the test, the variance of pain severity 1.7, and the minimum significant difference 0.8. Data were analyzed using STATA ver. 11.0. Independent t-test and chi-squared test were used to evaluate the quantitative and qualitative variables, respectively. Two-way ANOVA and Bonferroni post hoc test were applied to assess inter- and intra-group differences in pain severity based on VAS at study intervals. Kaplan-Meier estimates were used to evaluate treatment success and log rank test to compare the treatment regiments. To this end, treatment success was defined as a decrease in pain severity at least three points on VAS. Statistical significance was defined at P<0.05.
Results
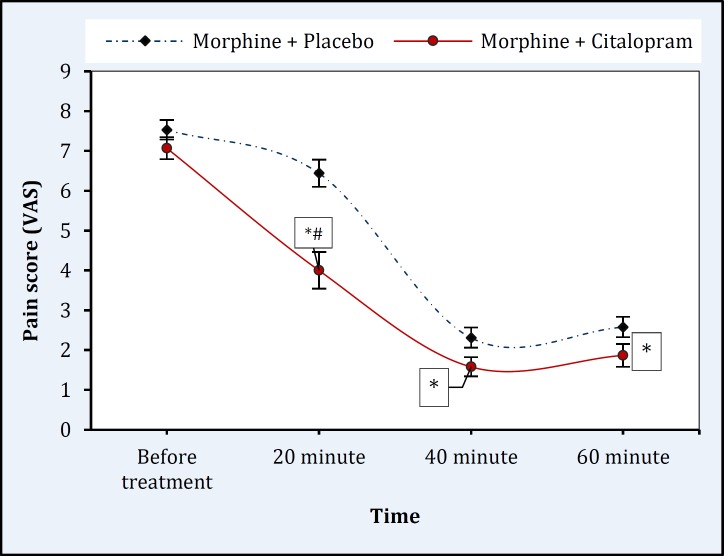
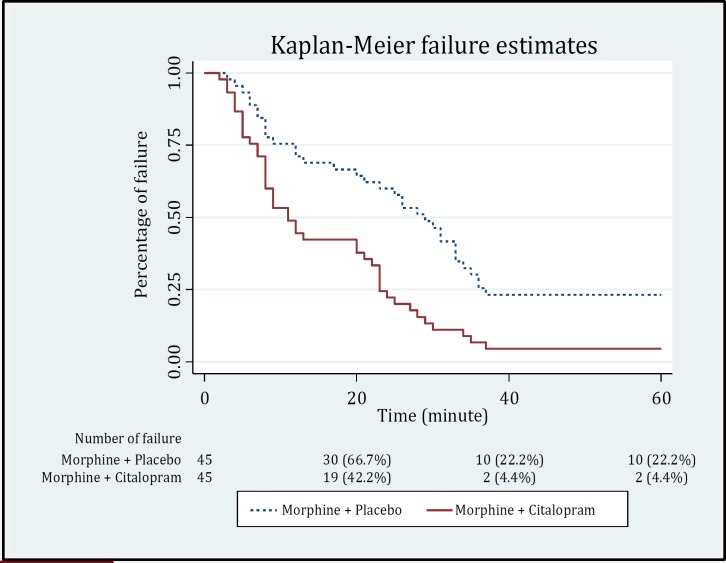
Ninety patients with acute colicky pain were equally assigned to two groups for treatment with morphine + placebo and morphine/citalopram. The mean ages of the subjects in two groups were 35.36±9.5 and 35.56±10.4 years, respectively (p=0.92). In the morphine/placebo and morphine/citalopram groups, 33 (73.3%) and 32 (71.1%) subjects were male, respectively (p=0.92). The mean VAS at the time of admission in the morphine/placebo and morphine/citalopram groups were 7.53±1.66 and 7.07±1.85, respectively (p=0.22). Twenty minutes after the first injection, the mean VAS decreased to 6.4±2.3 and 4.0±3.1 in the morphine/placebo and morphine/citalopram groups, respectively. The decrease in pain severity in the morphine/citalopram group was significantly compared to the morphine/placebo group and the time before administration of the medications (baseline) (p<0.001). In contrast, administration of morphine and placebo did not have a significant effect on pain severity at this interval (p=0.32). The mean pain severity 20 minutes after the second injection meaningfully decreased (40 minutes after the first injection) in the morphine/citalopram group [mean (SD)= 1.6 (1.6); p< 0.001] and in the morphine/placebo group [mean (SD)= 2.31 (1.72); p<0.001]. Pain severity was not considerably different between the two study groups (p>0.99). The third injection did not have any extra effect on pain intensity in both groups (p>0.99) (Figure 1). Two-way ANOVA showed that the therapeutic interventions resulted in a significant decrease in pain severity (df: 1.7; F=66.9; p<0.001). Kaplan-Meier curve showed that the first injection was successful in relieving pain in 15 (33.3%) and 26 (57.8%) subjects in the morphine/ placebo and morphine/citalopram groups, respectively. The second injection of these medications resulted in therapeutic success in 35 (87.8%) and 42 (95.6%) subjects in the above groups, respectively. Log rank test showed a remarkable difference in the treatment success between the two groups (p=0.001) (Figure 2).
Figure 1.
Time trend of pain severity in the morphine/placebo and morphine/citalopram groups. Data were presented as means and standard errors. * Significant difference compared to the period before treatment at P<0.001; # Significant difference with same time in the morphine/placebo group at P<0.001.
Figure 2.
The Kaplan-Meier curve to show the success rate in patients’ underling treatment with two drug regimens of morphine + placebo and morphine + citalopram. Log rank test showed a significant difference in treatment success between the two groups (P=0.001).
Discussion
Based on the findings of present study, combination of morphine sulfate and citalopram has significantly higher success rate in pain control of renal colic during the first 20-minute period in comparison to morphine alone. However, administration of morphine and placebo did not have a noteworthy effect on pain severity at this interval. There were no meaningful differences in the second and third dose administrations between two groups regarding changes in pain severity (figure 1). But, the results of the log rank test revealed a significantly higher success rate in morphine/citalopram group at the same time. It means that, although the two groups were able to equal changes in pain severity during a 60-minute period, but the failure rate was considerably higher in patients received morphine alone. Previous studies have shown that use of morphine results in an increase of serotonin levels in the brain; also, use of citalopram increases serotonin concentration by inhibiting its re-uptake (15). On the other hand, the tranquilizing effect of citalopram helps relieving pain in these patients. Sacerdote et al. concluded that the analgesic effect of some antidepressant seems to be related to an activation of the endogenous opioid system mediated by serotonin (16). Therefore, it seems that the combination of a serotonin re-uptake inhibitor and morphine sulfate have synergistic effects regarding pain control. Since citalopram has a minimum side effects compared to other inhibitors of serotonin re-uptake inhibitors, it could be considered as a suitable choice for this object. Campo and their colleague revealed the potential effects of citalopram for functional pediatric recurrent abdominal pain control (17). A randomized double-blind study showed a moderate analgesic effect of citalopram in patients with Pain disorder and declared that it appears to be not correlated to changes in depressive scores (18). Also, citalopram had a positive effect on chronic pelvic pain control and relieving peripheral neuropathic pain in diabetic patients (19, 20). The present study showed that citalopram in combination with morphine causes to increase the efficacy of morphine in relieving the pain of renal colic. Further studies are needed to evaluate of action mechanisms and potential complications.
Limitation
Although the VAS is a standard scoring system for evaluation of pain severity, the use of functional (21) and behavioral (22) indices, as an adjunct to VAS, could be more accurate. However, the study power of 99% made the findings of the study valid.
Conclusion:
It seems that the combination of citalopram and morphine sulfate causes to an increased efficacy and higher success rate in pain control of patients presented to the emergency department with a complaint of renal colic.
Acknowledgments:
We acknowledge all staffs of emergency department and dialysis unit of Al-Zahra hospital, Isfahan, Iran.
Conflict of interest:
None
Funding support:
None
Authors’ contributions:
All authors passed four criteria for authorship contribution based on recommendations of International Committee of Medical Journal Editors.
References
- 1.Curhan GC, Willett WC, Rimm EB, Stampfer MJ. Family history and risk of kidney stones. J Am Soc Nephrol. 1997;8(10):1568–73. doi: 10.1681/ASN.V8101568. [DOI] [PubMed] [Google Scholar]
- 2.Safdar B, Degutis LC, Landry K, Vedere SR, Moscovitz HC, D’Onofrio G. Intravenous morphine plus ketorolac is superior to either drug alone for treatment of acute renal colic. Ann Emerg Med. 2006;48(2):173–81. doi: 10.1016/j.annemergmed.2006.03.013. [DOI] [PubMed] [Google Scholar]
- 3.Labrecque M, Dostaler L-P, Rousselle R, Nguyen T, Poirier S. Efficacy of nonsteroidal anti-inflammatory drugs in the treatment of acute renal colic: a meta-analysis. Arch Intern Med. 1994;154(12):1381–7. [PubMed] [Google Scholar]
- 4.Segura JW, Preminger GM, Assimos DG, et al. Ureteral stones clinical guidelines panel summary report on the management of ureteral calculi. J Urol. 1997;158(5):1915–21. doi: 10.1016/s0022-5347(01)64173-9. [DOI] [PubMed] [Google Scholar]
- 5.Holdgate A, Pollock T. Nonsteroidal anti-inflammatory drugs (NSAIDs) versus opioids for acute renal colic. Cochrane Database Syst Rev. 2004;1:CD004137. doi: 10.1002/14651858.CD004137.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Teichman JM. Acute renal colic from ureteral calculus. N Engl J Med. 2004;350(7):684–93. doi: 10.1056/NEJMcp030813. [DOI] [PubMed] [Google Scholar]
- 7.Tramŕr DM, Williams J, Carroll D, Wiffen P, Moore R, McQuay H. Comparing analgesic efficacy of non‐steroidal anti‐inflammatory drugs given by different routes in acute and chronic pain: a qualitative systematic review. Acta Anaesthesiol Scand. 1998;42(1):71–9. doi: 10.1111/j.1399-6576.1998.tb05083.x. [DOI] [PubMed] [Google Scholar]
- 8.Cevik E, Cinar O, Salman N, et al. Comparing the efficacy of intravenous tenoxicam, lornoxicam, and dexketoprofen trometamol for the treatment of renal colic. Am J Emerg Med. 2012;30(8):1486–90. doi: 10.1016/j.ajem.2011.12.010. [DOI] [PubMed] [Google Scholar]
- 9.Hemrika D, Bossuyt P. Ketorolac versus morphine for severe pain. Trial. 1997;350:774–9. [Google Scholar]
- 10.Schröder W, Vry J, Tzschentke TM, Jahnel U, Christoph T. Differential contribution of opioid and noradrenergic mechanisms of tapentadol in rat models of nociceptive and neuropathic pain. Eur J Pain. 2010;14(8):814–21. doi: 10.1016/j.ejpain.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 11.Bomholt SF, Mikkelsen JD, Blackburn-Munro G. Antinociceptive effects of the antidepressants amitriptyline, duloxetine, mirtazapine and citalopram in animal models of acute, persistent and neuropathic pain. Neuropharmacology. 2005;48(2):252–63. doi: 10.1016/j.neuropharm.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 12.O'Connor A, Schug SA, Cardwell H. A comparison of the efficacy and safety of morphine and pethidine as analgesia for suspected renal colic in the emergency setting. J Accid Emerg Med. 2000;17(4):261–4. doi: 10.1136/emj.17.4.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tartau L. The effects of citalopram and escitalopram in visceral pain and behavioral models in mice: experimental researches. Eur J Pain. 2009;13:S56. [Google Scholar]
- 14.Reinhart DJ. Minimising the adverse effects of ketorolac. Drug Saf. 2000;22(6):487–97. doi: 10.2165/00002018-200022060-00007. [DOI] [PubMed] [Google Scholar]
- 15.Rafieian-Kopaei M, Gray AM, Spencer PS, Sewell RD. Contrasting actions of acute or chronic paroxetine and fluvoxamine on morphine withdrawal-induced place conditioning. Eur J Pharmacol. 1995;275(2):185–9. doi: 10.1016/0014-2999(94)00770-8. [DOI] [PubMed] [Google Scholar]
- 16.Sacerdote P, Brini A, Mantegazza P, Panerai AE. A role for serotonin and beta-endorphin in the analgesia induced by some tricyclic antidepressant drugs. Pharmacol Biochem Behav. 1987;26(1):153–8. doi: 10.1016/0091-3057(87)90548-x. [DOI] [PubMed] [Google Scholar]
- 17.Campo JV, Perel J, Lucas A, et al. Citalopram treatment of pediatric recurrent abdominal pain and comorbid internal-izing disorders: an exploratory study. J Am Acad Child Adolesc Psychiatry. 2004;43(10):1234–42. doi: 10.1097/01.chi.0000136563.31709.b0. [DOI] [PubMed] [Google Scholar]
- 18.Aragona M, Bancheri L, Perinelli D, et al. Randomized double‐blind comparison of serotonergic (Citalopram) versus noradrenergic (Reboxetine) reuptake inhibitors in outpatients with somatoform, DSM‐IV‐TR pain disorder. European Journal of Pain. 2005;9(1):33–8. doi: 10.1016/j.ejpain.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 19.Brown CS, Franks AS, Wan J, Ling FW. Citalopram in the treatment of women with chronic pelvic pain: an open-label trial. J Reprod Med. 2008;53(3):191–5. [PubMed] [Google Scholar]
- 20.Qinying C, Zhixiong T, Jinwei W. Therapeutic effects of citalopram on alleviating pain of peripheral neuropathy in type 2 diabetic patients. Med J Chin PLA. 2008;3:32–8. [Google Scholar]
- 21.Jensen MP, Smith DG, Ehde DM, Robinsin LR. Pain site and the effects of amputation pain: further clarification of the meaning of mild, moderate, and severe pain. Pain. 2001;91(3):317–22. doi: 10.1016/S0304-3959(00)00459-0. [DOI] [PubMed] [Google Scholar]
- 22.Farrar JT, Portenoy RK, Berlin JA, Kinman JL, Strom BL. Defining the clinically important difference in pain outcome measures. Pain. 2000;88(3):287–94. doi: 10.1016/S0304-3959(00)00339-0. [DOI] [PubMed] [Google Scholar]