Abstract
Staphylococcus aureus (S. aureus) is an opportunistic bacterial pathogen responsible for a diverse spectrum of human diseases, resulting in considerable yearly mortality rates. Due to its rapid acquisition of antibiotic resistance, it becomes increasingly difficult to cure S. aureus infections with conventional antibiotics. Immunotherapy represents a promising alternative strategy to prevent and/or treat the infection. In the present study, passive immunization with polyclonal antibodies targeting three possible S. aureus antigens, Hla, SEB and MntC (termed “SAvac-pcAb”) after challenge with lethal dose of S. aureus resulted in reduced bacterial loads, inflammatory cell infiltration and decreased pathology, and was able to provide nearly complete protection in a murine sepsis model. In vitro studies confirmed the direct interaction of SAvac-pcAb with S. aureus bacteria. Additional studies validated that SAvac-pcAb contained both opsonic and neutralizing antibodies that contributed to its protective efficacy. The former mediated opsonophagocytosis in a neutrophil-dependent manner, while the later inhibited the biological functions of Hla and SEB, two major virulence factors secreted by S. aureus. Critically, we demonstrated that SAvac-pcAb was cross-reactive with different clinical strains of S. aureus. These results confirmed the efficacy for treatment of S. aureus infection by passive immunization as an important therapeutic option.
Staphylococcus aureus (S. aureus) is an opportunistic bacterial pathogen that is responsible for a variety of superficial and invasive infectious diseases in human, including soft tissue infection, bacteremia, endocarditis, pneumonia, sepsis, and general wound infections1. Such infections are associated with considerable morbidity and mortality, both in hospitals and the greater community, thereby posing a major global health challenge2. In addition, the emergence of drug-resistance strains, such as methicillin-resistant S. aureus (MRSA) and vancomycin-resistant S. aureus (VRSA), make it increasingly difficult to cure the infection3.
Immunotherapy represents a promising strategy to prevent S. aureus related infectious diseases4,5. Efforts to develop an effective vaccine against S. aureus infection have been ongoing, with extensive studies currently underway6. A wide variety of proteins from S. aureus were identified as promising candidate antigens, including capsular polysaccharides7, secreted toxins8, and out membrane proteins9. In previous studies, we reported three proteins that exhibited protective immunity against S. aureus infection, including a genetically detoxified staphylococcal alpha-toxin mutant H35L (mHla)10, staphylococcal enterotoxin B mutant L45R/Y89A/Y94A (mSEB)11 and wild-type manganese transport protein C (MntC) (submitted). Active immunization with either of these proteins was able to induce specific antibodies and cellular immune responses, resulting in reduced bacterial loads and inflammation reaction, as well as improved survival time and rate in mice.
However, S. aureus usually causes an acute infection with rapid progression, and 60% of patients with invasive infections die within 7 days of culturing positive for MRSA12, indicating that active immunization is not the best choice for the prevention of such acute infections. Contrastingly, passive immunization is able to provide immediate and effective protection, as previous studies have demonstrated that antibody responses play a major protective role in specific immunity against MRSA13, and passive immunization with antigen specific antibody is able to provide partial protection against S. aureus infections14,15. Thus, in this study, we have systematically evaluated the protective efficacy of passive immunization with rabbit-generated polyclonal antibodies against mHla, mSEB, and MntC (termed “SAvac-pcAb”) in a murine sepsis model, and further investigated the possible mechanisms that might contribute to its protective immunity.
Results
Rabbit-generated pcAbs recognize recombinant proteins and sonicated MRSA252 whole cell lysates with high IgG titer
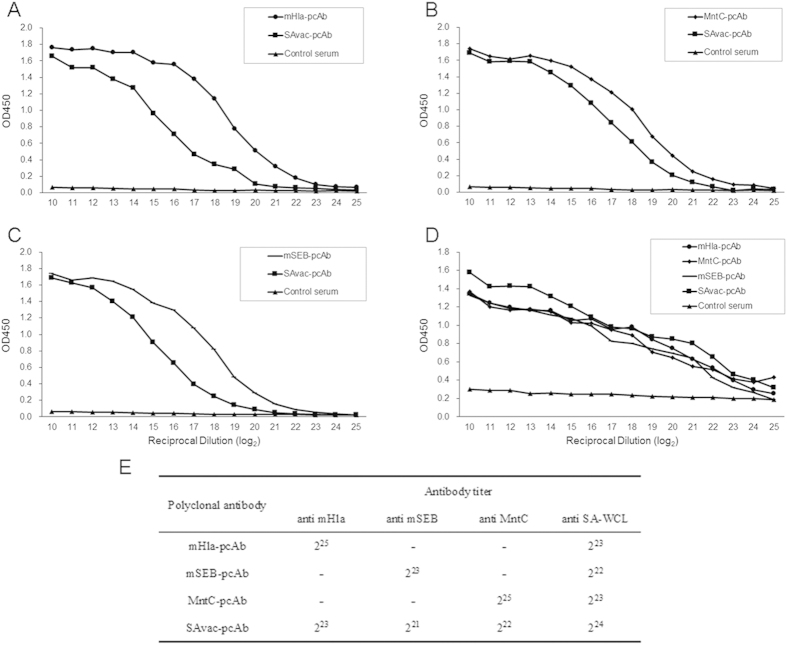
In this study, pcAbs against mHla, mSEB, MntC, and SAvac (named as mHla-pcAb, mSEB-pcAb, MntC-pcAb, and SAvac-pcAb, respectively) were generated in New Zealand white rabbits and purified. These PcAbs were further characterized by the titers of specific IgG antibodies against different recombinant proteins as well as sonicated MRSA252 whole cell lysates (SA-WCL). As shown in Fig. 1, these pcAbs interacted with immunized proteins with high titer, ranging from 221 to 225. Both mHla and MntC exhibited a similar antibody-induction response (225), which was four-fold higher when compared to mSEB (223). Furthermore, SAvac-pcAb was able to react with all the three proteins, with an IgG titer that was four- to eight-fold lower when compared to pcAb against a single protein. More importantly, pcAbs that generated by recombinant proteins were also able to recognize SA-WCL, with a titer range from 222 to 224. SAvac-pcAb exhibited a relatively high titer, as it was raised in rabbits immunized with all three antigens. Taken together, these results suggested that the pcAbs generated in this study were able to recognize S. aureus with high IgG titers in vitro.
Figure 1. Characterization of pcAb generated from rabbits immunized with mHla, mSEB, MntC, and SAvac.
ELISA was used to determine the titer of antigen-specific IgG for the indicated pcAbs. In brief, 96-well plates were pre-coated with mHla (A), mSEB (B), MntC (C), and sonicated MRSA252 whole cell lysates (SA-WCL) (D). The concentration of purified rabbit-raised antibodies was adjusted to 20 mg/ml and then added to the well by a two-fold serial dilution (210 to 225). The OD450 from each dilution was then determined. Data were presented as the mean from two separate experiments, each individually conducted in triplicate. (E) Presented as the titer of antigen-specific IgG antibody for each pcAb, which was defined as the highest dilution giving an absorbance value of more than twice that of the blank control.
Passive immunization protects mice against lethal challenge of S. aureus
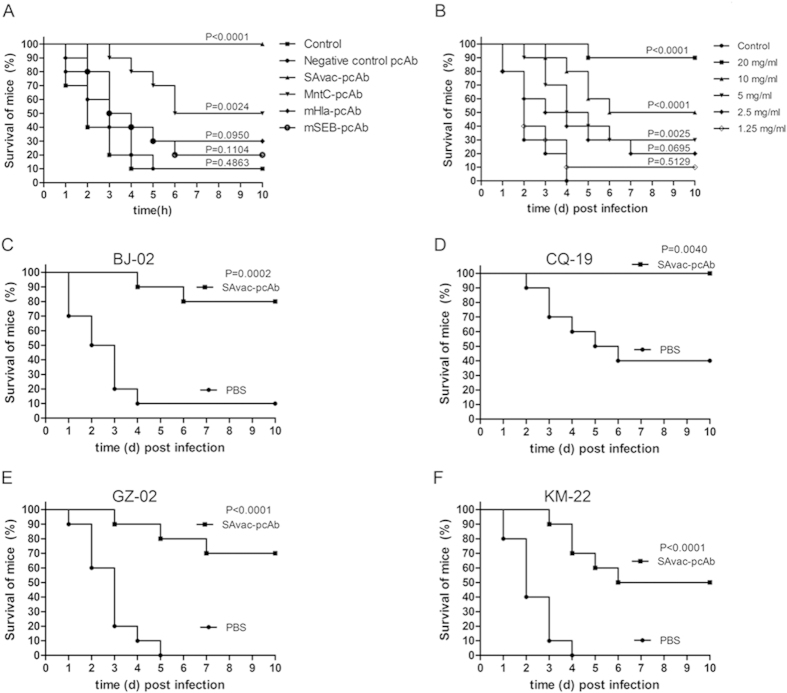
We next examined the protective efficacy of passive immunization with pcAbs generated above in a murine sepsis model. As shown in Fig. 2A, mice (n = 10) immunized with mHla-pcAb, mSEB-pcAb, MntC-pcAb, and SAvac-pcAb all displayed higher survival rates (30%, 20%, 50% and 100%, respectively) as compared to the PBS control group (10% survival). The mice that were passively immunized with SAvac-pcAb exhibited the highest survival rate, which was significantly higher than any other group (P < 0.05), with an ED50 of 7.37 mg/ml as calculated by the survival rates from mice immunized with different concentrations of SAvac-pcAb (Fig. 2B). For the other three experimental groups immunized with antibodies generated using only a single antigen, mice immunized with MntC-pcAb exhibited the highest survival rate when compared to subjects immunized with either mHla-pcAb or mSEB-pcAb. In addition, passive immunization prolonged the survival time of dead mice. In the PBS control group, mice did not survive past 4 days post-infection, Contrastingly, immunized mice exhibited survival times nearly 6 days post-infection. Further, higher survival rate was not observed in mice that were immunized with negative control pcAb compared with mice that were immunized with PBS, indicating that the protection efficacy observed was directly provided by antigen specific pcAbs.
Figure 2. Passive immunization with pcAbs protect mice from lethal S. aureus challenge.
Mice were infected intravenously with 100 μl of a lethal dose of S. aureus. 100 μl of each pcAb (20 mg/ml) was injected intravenously 2 h post infection and the survival rate for each group was monitored for 10 days after the initial infection. (A) Survival rates of mice (n = 10) infected with MRSA252 and passively immunized with different kind of pcAbs, as indicated. (B) Survival rates of mice (n = 10) infected with MRSA252 and passively immunized with different concentration of SAvac-pcAb, as indicated. (C–F) Survival rates of mice (n = 10) infected with different clinical strains of S. aureus and passively immunized with SAvac-pcAb. The differences between vaccinated and PBS control mice were presented as p-value.
As the amino acid sequences of Hla, SEB, and MntC were highly conserved among MRSA252 and different clinical strains (Supplementary Fig. 1–3). We wanted to know if pcAb generated by proteins from MRSA252 could provide protective immunity against challenge with different clinical strains of S. aureus. In this study, 4 clinical strains were chosen from a library that was established by our Lab based on their representation and diversity. The library contains more than 300 clinical isolates of S. aureus collected from different districts of China. The information of the 4 isolates was listed in supplementary table 1. As shown in Fig. 2C–F, all the 4 clinical strains exhibited different pathogenicity and virulence in mice, as indicated by the survival rates in the PBS group. SAvac-pcAb was able to protect 60% to 70% of mice from the clinical isolates challenge when compared to PBS controls. These results strongly indicated that SAvac-pcAb can provide cross-protective efficacy in mice challenged by different clinical strains of S. aureus.
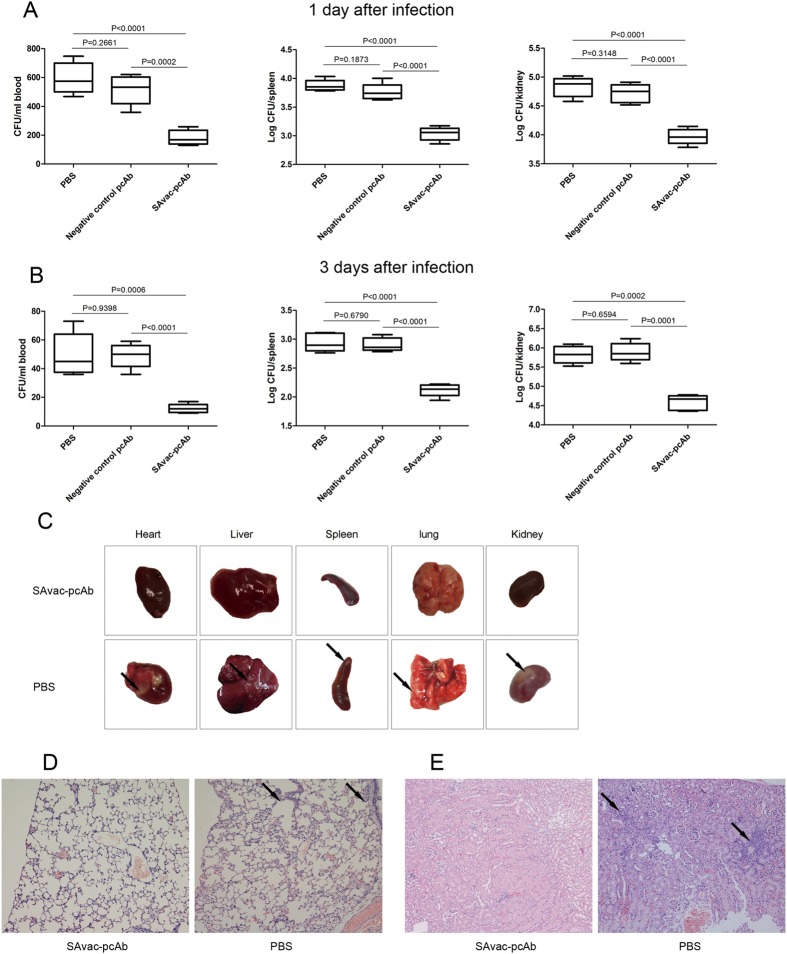
Passive immunization with SAvac-pcAb correlates with reduced bacterial burden and pathology
The blood, spleens, and kidneys from immunized and control mice were harvested and bacterial burden at 1 and 3 days post MRSA252 infection was then evaluated. As shown in Fig. 3A,B, mice that were passively immunized with SAvac-pcAb showed lower bacterial loads of S. aureus in the selected organs than those from PBS controls. This decrease in load was evident at both 1 and 3 days after infection. These results suggested that SAvac-pcAb was able to partially inhibit S. aureus growth and colonization in vivo. Meanwhile, bacterial loads in mice that were passively immunized with negative control pcAb were similar as that immunized with PBS, indicating that antigen specific pcAbs directly correlated with reduced bacterial burden rather than by nonspecific stimulation of immune responses by foreign antibody.
Figure 3. Passive immunization with SAvac-pcAb correlates with reduced bacterial burden and decreased pathology.
(A,B) Bacterial loads in the blood, spleens, and kidneys of mice intravenously immunized with SAvac-pcAb, negative control pcAb and PBS were determined 1 (A) and 3 days (B) after infection with 5 × 108 CFU of MRSA252. Each group includeed 5 mice. Data were presented as box plots, with the median and interquartile ranges as indicated. The differences between vaccinated and control mice were indicated as p-value. (C) Gross pathology of different organs from mice immunized with SAvac-pcAb and PBS with representative figures from 5 mice per group were shown. Arrows indicate typical staphylococcal abscesses in the organs. (D,E) Hematoxylin-eosin-stained kidneys (D) and lung (E) from mice immunized with SAvac-pcAb and PBS. 3 days after infection and immunization, kidneys and lungs were harvested and stained. Representative histopathological sections from 5 mice per group were shown (magnification = 100 X). Arrows indicated inflammatory cell infiltration.
Passive immunization with SAvac-pcAb also reduced the pathology of S. aureus infection. Representative gross pathology of different organs from immunized or PBS control mice were collected and imaged. No significant pathological changes were observed in SAvac-pcAb immunized mice. However, typical staphylococcal abscesses were observed in mice immunized with PBS (Fig. 3C). Consistently, histological analysis showed that mice immunized with SAvac-pcAb exhibited reduced inflammatory cell infiltration, bleeding, and tissue damage when compared to PBS group (Fig. 3D,E). These results further confirmed a protective efficacy of SAvac-pcAb in vivo.
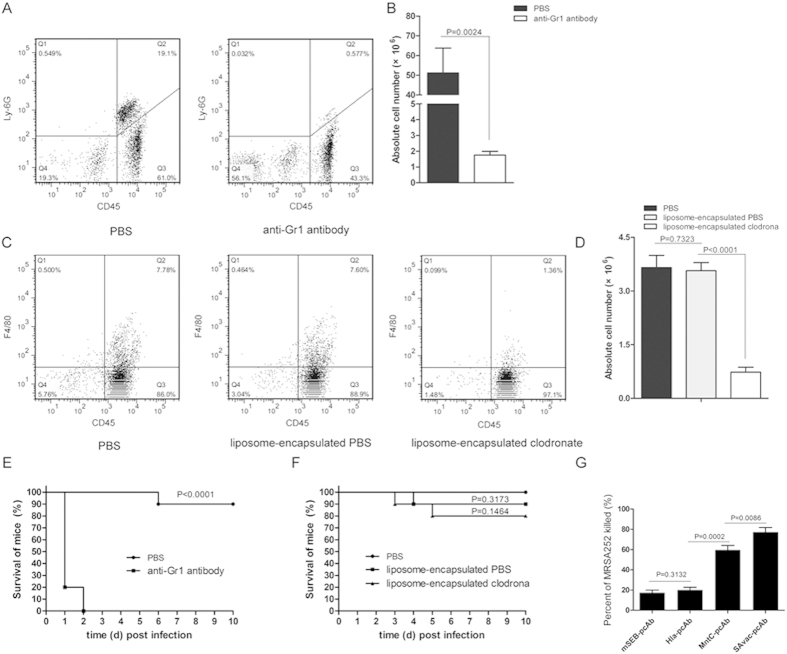
Neutrophils, but not macrophages, are essential for SAvac-pcAb induced protection and are able to kill S. aureus in vitro
Neutrophils and macrophages are the two major types of phagocytes found in peripheral blood that function in antibody-mediated opsonophagocytosis16. Given their importance, we sought to determine which cell type was essential for the SAvac-pcAb mediated protection observed during S. aureus challenge. Neutrophils and macrophages in BALB/c mice were depleted using an anti-Gr1 antibody and liposome-encapsulated clodronate, respectively. As shown in Fig. 4A–D, flow cytometry assay indicated that the absolute number and percentage of neutrophils and macrophages in depleted mice were significantly reduced as compared to control mice, with a deletion rate of 96.6% and 80.0% for neutrophils and macrophages, respectively.
Figure 4. Neutrophils are involved in SAvac-pcAb induced protection against lethal S. aureus challenge.
(A,B) Neutrophils in BALB/c mice (n = 5) were depleted using anti-Gr1 antibody as previously described. Flow cytometry assay indicated that the percentage (A) and absolute number (B) of neutrophils in depleted mice were significantly reduced when compared to PBS-treated group. (C,D) Macrophages in BALB/c mice were depleted with liposome-encapsulated clodronate, flow cytometry assay indicated that percentage (C) and absolute numbers (D) of macrophages in the liposome-encapsulated clodronate group were significantly reduced when compared to liposome-encapsulated PBS, whereas the latter exhibited no difference when compared to PBS controls. (E,F) Survival rates of neutrophil (E) and macrophage (F) depleted or control mice (n = 10) were infected with MRSA252 and passively immunized with SAvac-pcAb. The differences between vaccinated and control mice were presented as p-value. (G) Opsonophagocytic killing assay, MRSA252 was incubated in the presence of isolated 4 × 105 HL-60 cells and pcAb in the presence of infant rabbit complement for 2 h at 37 °C, and plated on agar medium and incubated for 24 h before measuring bacterial survival as determined by CFU. The percentage of killing was calculated to determine killing activity. Data shown were means ± standard deviation (SD) derived from three independent experiments. The differences between each group were presented as p-value.
After MRSA252 challenge and subsequent passive immunization with SAvac-pcAb, all neutrophil-depleted mice (n = 10) died within two days. This was significantly different from those in the PBS control group (10%, P < 0.0001) (Fig. 4C), contrastingly, macrophage-depleted mice showed no difference in survival rates when compared to either PBS or liposome-encapsulated PBS group (Fig. 4D). These results indicated that neutrophils were critical in SAvac-pcAb mediated protection against S. aureus infection.
We then carried out an in vitro opsonophagocytic killing assay to confirm the protective role of neutrophils. In the presence of differentiated HL-60 cells and rabbit serum complement, all 4 pcAbs exhibited increased opsonophagocytic activity for MRSA252. SAvac-pcAb was able to effectively kill more than 70% of the bacteria, which was significantly higher than the other 3 pcAbs. In addition, MntC-pcAb exhibited a higher opsonophagocytic activity as compared to either mHla-pcAb or mSEB-pcAb. No differences were observed between the latter two (Fig. 4E). These results indicated (i) SAvac-pcAb was able to kill MRSA252 cells efficiently in vitro and (ii) MntC-specific IgG might be the major antibody involved in neutrophil-dependent, opsonophagocytic killing.
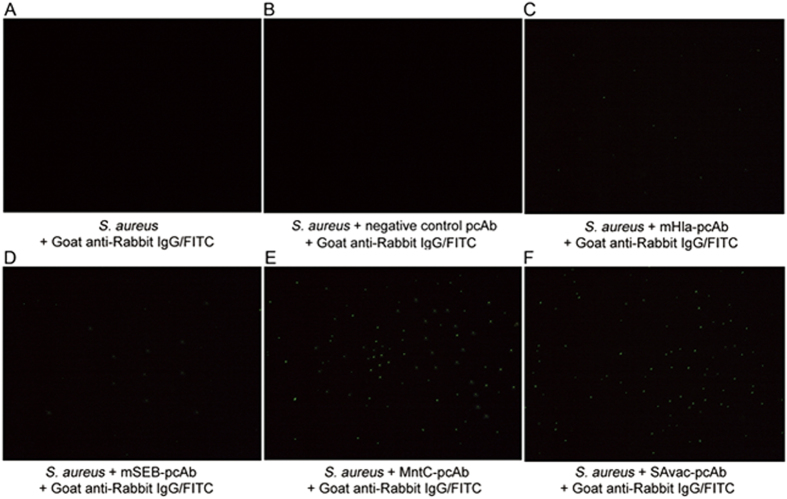
pcAbs are able to directly recognize MRSA252 in vitro
Since all the antigens used to generate pcAb in this study were surface exposed (MntC) or secreted (SEB and Hla) proteins, we wondered if specific antibodies generated by these antigens could directly recognize S. aureus in vitro. In this study, indirect immunofluorescence assay was carried out to validate the interaction between pcAb and MRSA252. The results clearly indicated that no immunofluorescence was detected in the absence of antigen specific pcAbs (Fig. 5A,B), whereas positive indirect immunofluorescence signals indicated the binding of four kinds of pcAb with MRSA252 (Fig. 5C–F). An increase in fluorescence signal intensity was observed in MntC-pcAb when compared to the mHla-pcAb and mSEB-pcAb group, this could be explained by the fact that MntC is a surface exposed protein while the other two are secreted toxins, and this result was consistent with our previous result that MntC-pcAb exhibited higher opsonophagocytic activity when compared to mHla-pcAb or mSEB-pcAb. Meanwhile, the fluorescence signal intensity was similar in SAvac-pcAb and MntC-pcAb group (Fig. 5E,F). Collectively, these results indicated that all pcAbs generated in this study were able to bind MRSA252 in vitro and MntC-pcAb was the most important antibody involved, and the binding of pcAbs with MRSA252 may essential in clearing and controlling the infection.
Figure 5. pcAbs are able to directly recognize MRSA252 in vitro.
Indirect immunofluorescence was conducted to confirm the binding of pcAb to MRSA252 in vitro. No immunofluorescence was detected in the absence of pcAb (A,B). Positive, indirect immunofluorescence signals indicated binding of different pcAb, as indicated, with MRSA252 (C–F). This study was performed twice, with similar results.
pcAbs inhibit the biological function of Hla and SEB in vitro
Hla functions as a hemolysin and is an important virulence factor in S. aureus17. We therefore examined the inhibitory efficacy of mHla-pcAb and SAvac-pcAb on hemolysis of rabbit erythrocyte by Hla. As shown in Fig. 6A, 10 μg of Hla exhibited similar hemolytic activity as compared to the positive control group (1% Triton X-100). In contrast, incubation of mHla-pcAb or SAvac-pcAb with Hla resulted in a dose-dependent inhibition of hemolytic activity. Further, no significant differences in hemolysis activity were observed when Hla was incubated with 1 mg of mHla-pcAb or SAvac-pcAb as compared to the negative control group, indicating that 1 mg of these antibodies was sufficient to completely inhibit the hemolytic activity of 10 μg Hla, which might be essential in SAvac-pcAb mediated protection during S. aureus infection.
Figure 6. pcAb inhibits the biological function of Hla and SEB in vitro.
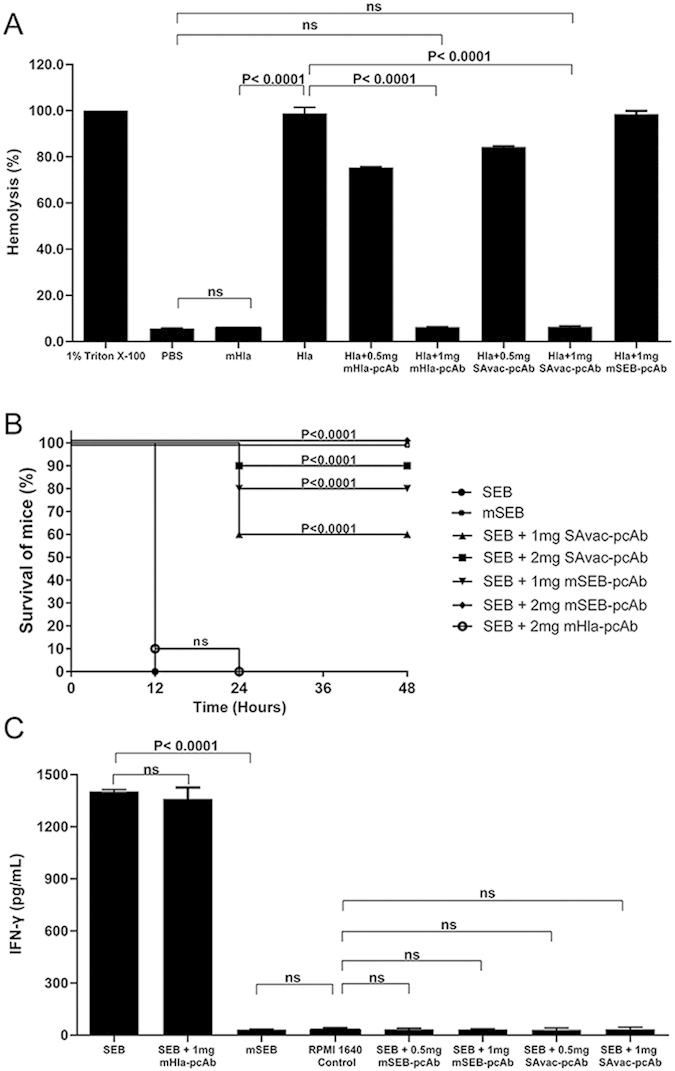
(A) Hemolytic activity assay, 1% rabbit erythrocytes diluted with PBS were incubated at 37 °C for 30 min with mHla, Hla, or Hla pre-incubated with mHla-pcAb or SAvac-pcAb, as indicated. The supernatant was then isolated by centrifugation and the hemolytic activity was determined by the release of hemoglobin, measured spectrophotometrically at 540 nm and presented as % hemolysis of the positive control (Triton X-100). Experiments were conducted in triplicate and data were presented as mean values ± standard deviation (SD). (B) Intestinal toxin activity assay, mice were injected i.p. with D-Galactosamine (200 mg/mL) followed by an intramuscular injection with the indicated concentrations of SEB, mSEB, PBS, or SEB incubated with mSEB-pcAb and SAvac-pcAb for 30 min prior to the start of the study. Survival was monitored for 40 h after the challenge and mHla-pcAb was used as a control, the differences between each group were presented as p-value. (C) IFN-γ production assay. Pig splenic leukocytes were isolated and cultured in the presence of the indicated concentrations of wild type SEB or mSEB. After 40 h of culture, supernatants were taken and ELISA was used to determine IFN-γ secretion. mHla-pcAb was used as control and data were presented as mean values ± standard deviation (SD). Experiments were conducted in triplicate.
Intestinal toxin activity is the most important biological function of SEB and it is directly involved in the pathogenicity of S. aureus18. We evaluated the impact of mSEB-pcAb and SAvac-pcAb on intestinal toxin activity of wild type SEB. After sensitizing with D-Galactosamine, all mice that were challenged with wild type SEB (25 μg) died within 24 h. In contrast, no death was observed in those subjects challenged with 0.2 mg of mSEB. In addition, incubation of SEB with either mSEB-pcAb or SAvac-pcAb significantly increased the survival rate in a dose dependent manner (Fig. 6B). These results confirm that SAvac-pcAb was able to inhibit the intestinal toxin activity of SEB efficiently.
SEB is also a super-antigen that is capable of robustly increasing IFN-γ production by mononuclear leukocytes19. As such, we determined the impact of mSEB-pcAb and SAvac-pcAb on SEB-mediated IFN-γ production by swine mononuclear leukocytes. As shown in Fig. 6C, compared to negative control, 10 μg of SEB significantly increased the secretion of IFN-γ (P < 0.0001), while the same amount of mSEB showed no difference. Furthermore, incubation of SEB with 0.5 or 1 mg of mSEB-pcAb or SAvac-pcAb resulted in a dramatic reduction of IFN-γ production. This was significantly different compared to SEB injection alone (P < 0.0001). These observations confirmed the inhibitory role of anti-mSEB antibody on the super-antigen activity of SEB.
Discussion
Passive immunization has long been used as an effective treatment option for either bacterial or viral infectious diseases20,21,22,23. Typically, three categories of antibodies were used for passive immunization, including (i) monoclonal antibody or its genetically modified derivatives24,25, (ii) Homologous or heterologous serum containing pcAb26, and (iii) IgG purified from pcAb (pcAb-IgG)20,27. In this study, pcAb-IgG was used for the treatment of S. aureus infection, as most of extra serum components that may inducing side effects were removed before immunization, it was safer than the other two categories of antibodies and exhibit higher specificity.
The efficacy of pcAb-IgG relies in large part on antigens used for the generation of pcAb. The protective efficacy of three antigens chosen in this study has been studied elsewhere8,10,11,15. Hla is a major virulence factor in S. aureus and is lethal to rodents and rabbits28, vaccination against Hla protects mice from lethal S. aureus pneumonia29. SEB is a S. aureus exotoxins and is directly associated with staphylococcal Toxic Shock Syndrome (TSS)30, SEB-specific monoclonal antibodies is able to partially protect against TSS18 and S. aureus infection31. MntC, a lipoprotein that is involved in the uptake of manganese ions32, is a highly conserved cell surface protein that elicits protective immunity against S. aureus33. Thus, all of the three chosen proteins are either key virulence factors of S. aureus or directly involved in bacterial metabolism, this range of antigens allows us the possibility of greatest infection control by blocking the biological function of these targets.
Antibodies function in various ways, as some can directly neutralize pathogens or secrete toxins, whereas others can evoke potent antibody-dependent cell-mediated cytotoxicity or complement dependent cytotoxicity34. As validated in both in vitro and in vivo studies, the efficacy of SAvac-pcAb lies in four features. (i) The antibody induced by MntC significantly promoted the ability of neutrophils in opsonophagocytic killing of S. aureus. (ii) SEB-specific neutralizing antibody functionally inhibited the intestinal toxin activity and super-antigen activity of the protein, thus preventing both TSS and cytokine storm, which were essential in death caused by S. aureus infection35. (iii) Hla specific antibody was able to block the hemolytic activity of Hla. (iv) SAvac-pcAb was induced by combined immunization and was able to simultaneously target multiple pathogenic pathways of S. aureus. As indicated in our results, an antibody induced by just one antigen provideed only partial protection (<50%), whereas combined immunization with SAvac-pcAb significantly enhanced overall protective efficacy (>90%).
Two categories of peripheral cells, neutrophils and macrophages, are the major cell types that function in antibody-mediated opsonophagocytosis. Li et al36 reported that Sao-induced antibodies significantly promoted the ability of porcine neutrophils in opsonophagocytic killing of S. suis, whereas a separate research group proposed that macrophages were essential for the killing of group B streptococci by opsonic antibody36. In our study, both in vitro and in vivo results emphasized the importance of neutrophils in the SAvac-pcAb mediated killing of S. aureus. However, the mechanism by which cell type is involved in antibody-mediated opsonophagocytic killing remains unclear, but likely includes many factors such as the subtype of the antibody.
Taken together, the results obtained in the present study demonstrated that therapeutic use of SAvac-pcAb resulting in reduced bacterial loads and improved protection in a sepsis model of lethal S. aureus infection. Antibody-mediated opsonophagocytosis by neutrophils, in combination with neutralizing activity against Hla and SEB, were essential for the high protective efficacy we observed. Since S. aureus has posed therapeutic challenges world-wide, and some strains become resistant to nearly all front-line antibiotics, our results provided the basis for an alternative therapeutic strategy for the treatment of S. aureus infection by pcAb-mediated immunotherapy.
Methods
Ethics statement
All animal care and use protocols in this study were performed in accordance with the Regulations for the Administration of Affairs Concerning Experimental Animals approved by the State Council of People's Republic of China. All animal experiments in this study were approved by the Animal Ethical and Experimental Committee of the Third Military Medical University (Chongqing, Permit No. 2011-04) in accordance with their rules and regulations. All surgery was performed under sodium pentobarbital anesthesia, and all efforts were made to minimize suffering.
Plasmids, proteins, bacterial strains, and culture method
Plasmids containing the sequence encoding wild type (Hla, SEB and MntC) and mutated (mHla, mSEB) proteins were constructed and maintained in our lab. Proteins were expressed and purified as described previously10,11,37. The S. aureus standard strain MRSA252 was purchased from ATCC (Manassas, VA, USA). Clinical strains of 4 S. aureus isolates were collected from 4 hospitals in different districts of China (Supplementary Table 1). Bacterial strains were cultured in tryptic soy broth, washed and diluted with sterile PBS to an appropriate cell concentration determined spectrophotometrically at 600 nm (OD600).
Production, purification, and characterization of pcAb
pcAbs were generated in New Zealand white rabbits based on a previously published method38. The IgG antibodies in the serum from antigen immunized or unimmunized rabbits were purified by affinity chromatography with a protein A column (GE, USA), followed by desalting with PBS, the concentration of each pcAb was determined by the BCA method39 and adjusted to a final concentration of 20 mg/ml. The titer of the antigen-specific IgG antibodies in each pcAb was determined by ELISA using Maxisorp microtiter plates that had been previously coated with each recombinant protein (400 ng/well) or SA-WCL (1 μg/well). The antibody titer was defined as the highest dilution with an absorbance value (OD450) of more than twice the blank control.
Immunization and bacterial challenge
Six- to eight-week-old female BALB/c mice were randomized into each group (n = 10), and infected intravenously with 100 μl of either a lethal dose of MRSA252 (1 × 109 CFU per mouse) or one of the 4 clinical strains (3 × 109 CFU per mouse). 2 h after infection, mice were passively immunized intravenously with 100 μl of each pcAb (2 mg) or the same volume of PBS for control subjects. The survival rates for all mice were monitored for 10 days after infection. To determine the ED50 of SAvac-pcAb, it was diluted to 5 different concentrations at 2-fold serial dilution and used for passive immunization. The ED50 was calculated by the Bliss method according to the survival rates for each group using SPSS13.0.
Bacterial burden and histopathological analysis
Mice were infected with 5 × 108 CFU of MRSA252 followed by passive immunization with 2 mg of SAvac-pcAb, 2 mg of negative control pcAb or the same volume of PBS. The blood, spleens, and kidneys were harvested and assessed for bacterial colonization at 1 and 3 days after infection. To calculate the bacterial number in each of the organs, organ homogenates were prepared in PBS and plated at 10-fold serial dilutions on tryptic soy agar. The colonies were quantified after 24 h of incubation at 37 °C. Histopathological analysis was conducted on day 14 after infection. Organs were fixed with 10% phosphate-buffered formalin and embedded in paraffin. Four-micrometer-thick sections were prepared and stained with hematoxylin and eosin (H&E) for microscopic examination.
Depletion of neutrophils and macrophages
To deplete neutrophils, mice were injected intraperitoneally (i.p.) with either 200 μg of anti-Gr1 antibody (volume of 100 μl, clone RB6-8C5, BioXCell, USA) or a control injection of the same volume of PBS 24 hours prior to the start of the study. Injections continued every other day throughout the duration of the study. To deplete macrophages, mice were injected intravenously with 100 μl of liposome-encapsulated clodronate (FormuMax Scientific, USA) 24 hours prior to the start of the study, PBS and liposome-encapsulated PBS were used as negative control.
Opsonophagocytic killing assay
The method used has been previously described by Burton and Nahm40. Briefly, HL-60 cells (ATCC, CCL-240) were differentiated into granulocyte-like cells with the addition of 100 mM N’,N dimethylformamide (Sagon, China) to the growth medium for 4 days. The assay was performed in 96-well plates, with each well containing the following: 4 × 105 HL60 cells, 103 CFU of MRSA252, 100 μg of each pcAb, and 1% infant rabbit serum as a complement source in a total volume of 80 μl. After incubation at 37 °C for 2 h, samples were plated on agar medium. The opsonophagocytic killing effect was defined as a reduction in CFU after overnight growth compared with the negative control group.
Flow cytometry
In 96-well, U-bottom plates, 1 × 106 erythrocyte-depleted cells in PBS and 2% FBS were added for a total volume of 100 μl. For the detection of macrophages in mouse spleens, single cell suspensions were stained with PE/Cy7 anti-mouse CD45 and APC anti-mouse F4/80. For the detection of neutrophils in mouse blood, cells were stained with PE/Cy7 anti-mouse CD45 and APC/cy7 anti-mouse Ly-6G (Biolegend, Inc., USA). Samples were then analyzed using BD FACSArray softwareTM on a BD FACSArray flow cytometer (BD Biosciences).
Indirect immunofluorescence
Indirect immunofluorescence was carried out based on a method established by us previously41.
Hemolytic activity assay
0.9 ml of rabbit erythrocyte suspension in PBS (1%) was mixed with 100 μl of Hla, mHla, and Hla that had been incubated with different concentrations of mHla-pcAb or SAvac-pcAb 30 min prior to the start of the study. An equal volume of 1% Triton X-100 and PBS were used as positive and negative controls, respectively. After a 30 min incubation at 37 °C, the mixtures were centrifuged at 400 × g for 10 min. The hemolytic activity was determined by the release of hemoglobin, measured spectrophotometrically at 540 nm and presented as % hemolysis of the positive control (Triton X-100).
Intestinal toxin activity assay
six- to eight-week-old female BALB/c mice were injected i.p. with 100 μl of D-Galactosamine (200 mg/ml) followed by an intramuscular injection of 100 μl of SEB (0.25 mg/ml), mSEB (2 mg/ml), or SEB (0.25 mg/ml) that had been incubated with 1 mg or 2 mg of mSEB-pcAb or SAvac-pcAb 30 min prior to the start of the study. mHla-pcAb was used as negative control. Survival was monitored for 40 h after injection.
IFN-γ production assay
Mononuclear leukocytes isolated from the spleen tissue of a healthy pig were counted and plated at 5 × 105 per well (100 μl) before incubation with RPMI 1640 medium (Gibco, Beijing, China) supplemented with 10% fetal calf serum (Gibco, USA), then 100 μl of SEB, mSEB, or SEB (0.1 mg/ml) that had been incubated 30 min prior to the start of the study with 0.5 or 1 mg of mSEB-pcAb or SAvac-pcAb were added to each well. Culture supernatants were harvested 40 h later, and porcine IFN-γ production was quantified using by ELISA. mHla-pcAb was used as the negative control.
Statistical analyses
Data were presented as mean ± standard deviation (SD). Means were compared using the two-tailed Student’s t-test. Mantel-Cox Log-rank analysis was utilized to determine differences in survival times. P < 0.05 was considered statistically significant.
Additional Information
How to cite this article: Zhang, J. et al. Protective Efficacy and Mechanism of Passive Immunization with Polyclonal Antibodies in a Sepsis Model of Staphylococcus aureus Infection. Sci. Rep. 5, 15553; doi: 10.1038/srep15553 (2015).
Supplementary Material
Acknowledgments
We thank Yongjun Ji, Daohua Mou and Yi Qin for their assistance in animal experiment.
Footnotes
Author Contributions J.Z. and F.Y. conducted the experiments, wrote the main manuscript text and prepared the figures and tables, X.Z., H.J., C.R. and C.C. helped to conducted the experiments, Y.D. and Y.Z. contributed to writing the manuscript and supervised the project. Q.Z. and H.Z. conceived the experiments and helped with the discussion of results and manuscript refinement. All authors reviewed the manuscript.
References
- Foster T. J., Geoghegan J. A., Ganesh V. K. & Hook M. Adhesion, invasion and evasion: the many functions of the surface proteins of Staphylococcus aureus. Nat Rev Microbiol 12, 49–62, (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kouyos R., Klein E. & Grenfell B. Hospital-community interactions foster coexistence between methicillin-resistant strains of Staphylococcus aureus. PLoS pathogens 9, e1003134 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arias C. A. & Murray B. E. Antibiotic-resistant bugs in the 21st century—a clinical super-challenge. N Engl J Med 360, 439–443 (2009). [DOI] [PubMed] [Google Scholar]
- Schaffer A. C. & Lee J. C. Vaccination and passive immunisation against Staphylococcus aureus. Int J Antimicrob Agents 32 Suppl 1, S71–78 (2008). [DOI] [PubMed] [Google Scholar]
- Shinefield H. R. & Black S. Prospects for active and passive immunization against Staphylococcus aureus. Pediatr Infect Dis J 25, 167–168 (2006). [DOI] [PubMed] [Google Scholar]
- Salgado-Pabon W. & Schlievert P. M. Models matter: the search for an effective Staphylococcus aureus vaccine. Nat Rev Microbiol 12, 585–591 (2014). [DOI] [PubMed] [Google Scholar]
- Maira-Litran T., Kropec A., Goldmann D. A. & Pier G. B. Comparative opsonic and protective activities of Staphylococcus aureus conjugate vaccines containing native or deacetylated Staphylococcal Poly-N-acetyl-beta-(1-6)-glucosamine. Infect Immun 73, 6752–6762 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy A. D. et al. Targeting of alpha-hemolysin by active or passive immunization decreases severity of USA300 skin infection in a mouse model. J Infect Dis 202, 1050–1058 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuklin N. A. et al. A novel Staphylococcus aureus vaccine: iron surface determinant B induces rapid antibody responses in rhesus macaques and specific increased survival in a murine S. aureus sepsis model. Infect Immun 74, 2215–2223 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuo Q. F. et al. Evaluation of the protective immunity of a novel subunit fusion vaccine in a murine model of systemic MRSA infection. PLoS One 8, e81212, (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Z. et al. Fine-mapping of immunodominant linear B-cell epitopes of the Staphylococcus aureus SEB antigen using short overlapping peptides. PLoS One 9, e90445 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bean H. D., Zhu J., Sengle J. C. & Hill J. E. Identifying methicillin-resistant Staphylococcus aureus (MRSA) lung infections in mice via breath analysis using secondary electrospray ionization-mass spectrometry (SESI-MS). J Breath Res 8, 041001 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birch H. Antibodies could lead to MRSA vaccine. Chem World 8, 21–21 (2011). [Google Scholar]
- Pastar I. et al. Interactions of methicillin resistant Staphylococcus aureus USA300 and Pseudomonas aeruginosa in polymicrobial wound infection. PLoS One 8, e56846 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson A. S. et al. Staphylococcus aureus manganese transport protein C is a highly conserved cell surface protein that elicits protective immunity against S. aureus and Staphylococcus epidermidis. J Infect Dis 205, 1688–1696 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor M. B., Phillips M. & Easmon C. S. Opsonophagocytosis of Pneumocystis carinii. J Med Microbiol 36, 223–228 (1992). [DOI] [PubMed] [Google Scholar]
- Thay B., Wai S. N. & Oscarsson J. Staphylococcus aureus alpha-toxin-dependent induction of host cell death by membrane-derived vesicles. PLoS One 8, e54661 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karauzum H. et al. Synthetic human monoclonal antibodies toward staphylococcal enterotoxin B (SEB) protective against toxic shock syndrome. J Biol Chem 287, 25203–2521 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inskeep T. K. et al. Oral vaccine formulations stimulate mucosal and systemic antibody responses against staphylococcal enterotoxin B in a piglet model. Clin Vaccine Immunol 17, 1163–1169 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sholukh A. M. et al. Passive immunization of macaques with polyclonal anti-SHIV IgG against a heterologous tier 2 SHIV: outcome depends on IgG dose. Retrovirology 11, 8 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mizrahi A., Collignon A. & Pechine S. Passive and active immunization strategies against Clostridium difficile infections: State of the art. Anaerobe 30, 210–219 (2014). [DOI] [PubMed] [Google Scholar]
- Itoh Y. et al. Protective efficacy of passive immunization with monoclonal antibodies in animal models of H5N1 highly pathogenic avian influenza virus infection. PLoS Pathog 10, e1004192 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varrone J. J., Li D., Daiss J. L. & Schwarz E. M. Anti-Glucosaminidase Monoclonal Antibodies as a Passive Immunization for Methicillin-Resistant Staphylococcus aureus (MRSA) Orthopaedic Infections. Bonekey Osteovision 8, 187–194 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li P. C. et al. Development of a humanized antibody with high therapeutic potential against dengue virus type 2. PLoS Negl Trop Dis 6, e1636 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pokorny N. J., Boulter-Bitzer J. I., Hall J. C., Trevors J. T. & Lee H. Inhibition of Cryptosporidium parvum infection of a mammalian cell culture by recombinant scFv antibodies. Antonie Van Leeuwenhoek 94, 353–364 (2008). [DOI] [PubMed] [Google Scholar]
- Aaberge I. S., Hvalbye B. & Lovik M. Enhancement of Streptococcus pneumoniae serotype 6B infection in mice after passive immunization with human serum. Microb Pathog 21, 125–137 (1996). [DOI] [PubMed] [Google Scholar]
- Kiraly J., Vareckova E., Mucha V. & Kostolansky F. Evaluation of anti-influenza efficiency of polyclonal IgG antibodies specific to the ectodomain of M2 protein of influenza A virus by passive immunization of mice. Acta Virol 55, 261–265 (2011). [DOI] [PubMed] [Google Scholar]
- Yarovinsky T. O., Monick M. M., Husmann M. & Hunninghake G. W. Interferons increase cell resistance to Staphylococcal alpha-toxin. Infect Immun 76, 571–577 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bubeck Wardenburg J., Bae T., Otto M., Deleo F. R. & Schneewind O. Poring over pores: alpha-hemolysin and Panton-Valentine leukocidin in Staphylococcus aureus pneumonia. Nat Med 13, 1405–1406 (2007). [DOI] [PubMed] [Google Scholar]
- Kashiwada T. et al. Staphylococcal enterotoxin B toxic shock syndrome induced by community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA). Intern Med 51, 3085–3088 (2012). [DOI] [PubMed] [Google Scholar]
- Varshney A. K. et al. Humanized staphylococcal enterotoxin B (SEB)-specific monoclonal antibodies protect from SEB intoxication and Staphylococcus aureus infections alone or as adjunctive therapy with vancomycin. J Infect Dis 210, 973–981 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horsburgh M. J. et al. MntR modulates expression of the PerR regulon and superoxide resistance in Staphylococcus aureus through control of manganese uptake. Mol Microbiol 44, 1269–1286 (2002). [DOI] [PubMed] [Google Scholar]
- Anderson A. S. et al. Staphylococcus aureus manganese transport protein C is a highly conserved cell surface protein that elicits protective immunity against S. aureus and Staphylococcus epidermidis. J Infect Dis 205, 1688–1696 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalenik B., Sawicka R., Gora-Sochacka A. & Sirko A. Influenza prevention and treatment by passive immunization. Acta Biochim Pol 61, 573–587 (2014). [PubMed] [Google Scholar]
- Zhang Y. et al. Kinase suppressor of Ras-1 protects against pulmonary Pseudomonas aeruginosa infections. Nat Med 17, 341–346 (2011). [DOI] [PubMed] [Google Scholar]
- Li Y. et al. Immunization with recombinant Sao protein confers protection against Streptococcus suis infection. Clin Vaccine Immunol 14, 937–943 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gribenko A. et al. Three-dimensional structure and biophysical characterization of Staphylococcus aureus cell surface antigen-manganese transporter MntC. J Mol Biol 425, 3429–3445 (2013). [DOI] [PubMed] [Google Scholar]
- Jinyong Z. et al. Fusion expression and immunogenicity of Bordetella pertussis PTS1-FHA protein: implications for the vaccine development. Mol Biol Rep 38, 1957–1963 (2011). [DOI] [PubMed] [Google Scholar]
- Walker J. M. The bicinchoninic acid (BCA) assay for protein quantitation. Methods Mol Biol 32, 5–8, (1994). [DOI] [PubMed] [Google Scholar]
- Burton R. L. & Nahm M. H. Development of a fourfold multiplexed opsonophagocytosis assay for pneumococcal antibodies against additional serotypes and discovery of serological subtypes in Streptococcus pneumoniae serotype 20. Clin Vaccine Immunol 19, 835–841 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang F. et al. Specific humoral immune response induced by propionibacterium acnes can prevent Actinobacillus pleuropneumoniae infection in mice. Clin Vaccine Immunol 21, 407–416 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.