Abstract
Abstract. Background: For decades we have understood the risk factors for suicide in the general population but have fallen short in understanding what distinguishes the risk for suicide among patients with serious psychiatric conditions. Aims: This prompted us to investigate risk factors for suicidal behavior among psychiatric inpatients. Method: We reviewed all psychiatric hospital admissions (2008–2011) to a centralized psychiatric hospital in Ontario, Canada. Using multivariable logistic regression we evaluated the association between potential risk factors and lifetime history of suicidal behavior, and constructed a model and clinical risk score to predict a history of this behavior. Results: The final risk prediction model for suicidal behavior among psychiatric patients (n = 2,597) included age (in three categories: 60–69 [OR = 0.74, 95% CI = 0.73–0.76], 70–79 [OR = 0.45, 95% CI = 0.44–0.46], 80+ [OR = 0.31, 95% CI = 0.30–.31]), substance use disorder (OR = 1.30, 95% CI = 1.27–1.32), mood disorder (OR = 1.49, 95% CI = 1.47–1.52), personality disorder (OR = 2.30, 95% CI = 2.25–2.36), psychiatric disorders due to general medical condition (OR = 0.52, 95% CI = 0.50–0.55), and schizophrenia (OR = 0.42, 95% CI = 0.41–0.43). The risk score constructed from the risk prediction model ranges from −9 (lowest risk, 0% predicted probability of suicidal behavior) to +5 (highest risk, 97% predicted probability). Conclusion: Risk estimation may help guide intensive screening and treatment efforts of psychiatric patients with high risk of suicidal behavior.
Keywords: suicidal risk, risk prediction, risk score, psychiatric comorbidity
Evaluation of suicide in the global context places it as one of the leading causes of death among younger populations (DeLeo, Bertolote, & Lester, 2002; Murray et al., 2002). Suicide in conjunction with associated suicidal behavior are potentially underreported (Mann, 2003); there may be 10–20 suicide attempts (SAs) for every completed suicide (Mann, 2003) and prior SA is one of the strongest predictors of eventual suicide completion (Blumenthal, Bell, Neumann, Schuttler, & Vogel, 1989; Teti, Rebok, Rojas, Grendas, & Daray, 2014). Important risk factors for suicide among the general population include burden of physical and psychiatric conditions (Furlanetto & Stefanello, 2011), substance use history, traumatic events, poor social support, marital status, and lower education level (Ekramzadeh et al., 2012). However, the adjusted risk contribution of each factor is unclear and the applicability of these risk factors to psychiatric patients warrants further investigations.
For decades we have understood the risk factors for suicide in the general population but have fallen short in understanding what distinguishes the risk for suicide among patients with serious psychiatric disorders requiring psychiatric admission. This can be a trying task in the field of psychiatry where we manage critically ill patients with multiple psychiatric and physical comorbidities. Although investigations have been conducted to examine the risk factors for suicide among the psychiatric population (Linehan, Goodstein, Nielsen, & Chiles, 1983; Modestin, Zarro, & Waldvogel, 1992; Powell, Geddes, Deeks, Goldacre, & Hawton, 2000; Roy & Draper, 1995; Sharma, Persad, & Kueneman, 1998), they suffered from considerably small samples ranging from 37 to 112 patients. It is also questionable whether the previous evidence was adequately powered to examine the association between multiple psychiatric diagnoses and suicidal behavior in an adjusted analysis. In addition, none of the authors of these works attempted to translate their findings into an adjusted risk score to better predict this suicidal ideation.
Recognizing these shortcomings, it is our collective responsibility to mitigate the risk of suicidal behavior by better identifying the psychiatric and demographic characteristics associated with suicide. This prompted our investigation into the factors predictive of suicidal behavior among patients with serious mental illness. We aimed to identify these factors by constructing a multivariable model for estimating suicidal behavior.
Provided our model is stable and well calibrated, we will also create a risk score for self-harm behavior without intent to die to be distinguished from suicidal behavior, which we define here as intentional self-harm with intent to die. Some evidence suggests different risk factors for SA and nonsuicidal self-injury (Nock et al., 2008; Sokero et al., 2003). Inadequate discrimination between self-injury based on intent to die could pose problems for risk prediction. Thus, our secondary aims included: (1) determining the differences in risk predictors for self-injury based on the patient's intent to die though subgroup analyses and (2) establishing whether the recentness of the behavior (3-month, 1-year, and lifetime history) impacted our results.
Method
This study was approved by the Hamilton Integrated Research Ethics Board (HIREB), study ID 11-3534. We reviewed the charts of men and women aged 18 years or older admitted from 2008 to 2011 to one regional psychiatric hospital located in Hamilton, Ontario, Canada. All patients admitted to this facility were routinely screened for history of suicidal behavior with standardized questions as part of clinical care. The assessment included questions about the most recent self-harm act (included timelines: never, more than 1 year ago, 31 days to 1 year ago, 8–30 days ago, 4–7 days ago, or 3 days ago and less). They were then asked whether or not their self-harm behavior was performed with the intent to die. We defined nonsuicidal self-injury as any acts of self-harm that include any tissue injury without the intent of death based on previously reported definition of self-harm (Kerr, Muehlenkamp, & Turner, 2010) in order to distinguish this behavior from an SA, which is defined as: "self-directed injurious behavior with any intent to die as a result of the behavior"(Centers for Disease Control and Prevention, 2015). We defined SA cases as patients who have made any self-harm act with the intent to die during their lifetime and nonsuicidal self-injury cases as patients who engaged in any self-harming behavior in their lifetime without such intent. We selected controls on the basis of not having any history of self-harm behavior.
The data-extraction forms were designed specifically to ensure the adequate collection of patient information and piloted tested among a single group of nurses to ensure their feasibility. We elected to extract information for variables that would have minimal chance for misclassification such as age, sex, employment, marital status, and source of income. Each variable is explicitly defined in the extraction form, and all variables are well captured by the electronic medical record (EMR) system used within the Hamilton health-care system. The pilot testing phase ensured variables such as income (pension, employment history, welfare) and marital status were available and easily identifiable. The extraction process was successful and led to negligible missing data (< 5%).
From each medical record, we abstracted the details of current psychiatric diagnosis, age, sex, marital status, history of SAs, postal code, and source of income. Source of income included categories such as social assistance, employment, disability insurance, employment insurance, other or no income. Psychiatric diagnoses included mood (any of: depression, dysthymia, or bipolar disorders); schizophrenia; substance use; personality, anxiety, or psychiatric disorder due to general medical condition; and other disorders (any of: childhood/adolescence, cognitive, somatoform, factitious, dissociative, sexual and gender identity, eating, sleep, impulse-control, and adjustment). This report adheres to the STROBE (von Elm et al., 2007) reporting guidelines.
The diagnoses collected for this study were obtained from the clinical record following inpatient assessments and clinical interviews that were conducted by psychiatrists and each diagnosis was assigned by the psychiatrist for the patient based on Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV), diagnostic criteria. Psychiatric diagnoses were determined based on psychiatric assessment performed by Canadian Royal College of Psychiatry board-certified psychiatrists and members of the Department of Psychiatry and Behavioural Neuroscience at McMaster University according to DSM-IV criteria. These diagnoses were the basis for treatment administration during the hospital stay as well as discharge planning and follow-up. Self-harm and suicidal behavior were ascertained in a similar way during clinical interviewing of all patients admitted to the hospital by clinical staff and entered in patients' medical charts to assess their risk of suicide. The clinicians asked the patients specific questions about suicide within the past 30 days prior to admission including questions on whether there was a history of self-harm before admission, how recently the self-harm behavior occurred, if the intent of this behavior was to end one's life, whether family/friends/care-giver/health-care providers expressed concern for the patient ending their life, and whether they had a suicide plan in the past 30 days.
Statistical Analysis
We examined the predictive ability of many risk variables, while simultaneously avoiding statistical overfitting, and aimed to create a simple and easy-to-use model (Babyak, 2004). We relied on a rigorous modeling approach sensible for small datasets (Steyerberg, Eijkemans, Harrell, & Habbema, 2001). We prespecified the following potential predictor variables for inclusion into a single multivariable logistic regression model: age (categorized as 18–24, 25–29, 30–39, 40–49, 50–59, 60–69, 70–79, 80+ years), marital status, sex, source of income, and different psychiatric disorders (substance use, mood, anxiety, personality, psychiatric disorder due to general medical condition, and others). These are the most important predictors of self-harm behavior (either with or without the intent to die) cited in the literature (Ekramzadeh et al., 2012; Furlanetto & Stefanello, 2011; March et al., 2014; Mok, Chan, Cheung, & Yip, 2013; Sokero et al., 2003). We calculated the variance inflation factor (VIF) for the variables in these analyses and prespecified recoding or removing variables that had a VIF greater than 10 (Schroeder, 1990).
We split the dataset randomly into two parts: a derivation set that included 75% of the observations (n = 1,948) and a validation set with 25% (n = 649). In the derivation set, we used all of the prespecified potential predictor variables to construct a single candidate logistic model for predicting risk of lifetime self-harm (either with or without intent to die). We then corrected each predictor's regression coefficient with a shrinkage factor estimated using penalized maximum likelihood estimation (Moons, Donders, Steyerberg, & Harrell, 2004). This method is applied during the modeling approach as opposed to after modeling is complete. Studies have demonstrated that, when compared with uniform shrinkage or no shrinkage at all, this method produces models that have better discrimination and calibration properties when validated in external datasets (Moons et al., 2004). To determine the individual shrinkage factors, we used a trial-and-error approach where we substituted a range of shrinkage factors (0–80) to identify the factor and maximized a modified Akaike's information criterion for each predictor. We then penalized all regression coefficients by their respective shrinkage factors.
Next, we reduced the full model to the fewest predictors that would still provide accurate and reliable prediction. We used the predicted probabilities estimated from the full penalized model as the dependent variable in an ordinary least squares linear regression and included all the same predictors from the full model as the independent variables. We calculated the R2 value (which equals 1). We then removed independent variables one by one from the linear regression and evaluated the impact of their removal on R2. Small decreases in R2 indicate that the removed independent variables have little predictive value. We termed this reduced model "the final model."
We then constructed a risk score by dividing the estimates of the β coefficients from the final model by a common denominator and rounding them to the nearest integer (Moons, Harrell, & Steyerberg, 2002; Sullivan, Massaro, & D'Agostino, 2004). We then estimated the probability of lifetime history self-harm behavior for all possible score totals.
We assessed our score's overall performance in the derivation and validation samples using the Brier score, discrimination using the C statistic (with 95% confidence intervals estimated using the jackknife procedure; Newson, 2006), calibration using plots of observed versus predicted probabilities and the Hosmer–Lemmeshow goodness-of-fit test (Harrell, Lee, & Mark, 1996), and clinical usefulness with decision curve analysis (Vickers & Elkin, 2006). Decision curves allow readers to determine the net benefit of using the model compared with "act-on-all" or "act-on-none" policies across different thresholds of the probability of a self-harm history (Vickers, Cronin, Elkin, & Gonen, 2008).
Finally, we used the full dataset to test the ability of the final model to predict: (1) self-harm behavior in the past 30 days, (2) self-harm behavior in the last year, (3) lifetime self-harm (but not SA), and (4) lifetime SA. We used Stata 12.1 (StataCorp, 2009) and R 3.02 (Team, 2013) with the rms package (Harrell, 2014) for all analyses.
Results
Patient Characteristics
There were 6,803 psychiatric admission records over the study period (2008–2011; see Figure SF1 in Electronic Supplementary Material 1 (249.4KB, pdf) ), representing the clinical history for 2,597 unique patients eligible for study inclusion. Of the eligible patients, 768 (29.6%) reported SA at least once in their lifetime, 196 (7.5%) reported nonsuicidal self-harm, and 1,633 (62.9%) reported no history of self-harm (control). Table 1 summarizes the patient characteristics according to the three groups: SA, self-harm, and control. Some of the diagnostic categories were limited by small sample size, requiring their combination into "other disorders" in the primary regression analyses.
Table 1. Demographic characteristics of suicide attempt and self-harm cases and controls.
| Total | SA cases | Self-Harm cases | Controls | ||||
|---|---|---|---|---|---|---|---|
| (n = 2,597) | (n = 768) | (n = 196) | (n = 1,633) | ||||
| n | n | %, (M, SD) | n | %, (M, SD) | n | %, (M, SD) | |
| Note. Marital status (1 with partner, 0 without) is dichotomized as either with (married or identified significant partner) or without (never married, widowed, separated, divorced) a significant partner. Other income includes: social assistance, disability insurance, employment insurance, other or no income. Other disorder includes: disorders of childhood/adolescence, cognitive disorders, somatoform disorders, factitious disorders, dissociative disorders, sexual and gender identity disorders, eating disorders, sleep disorders, impulse-control disorders not classified elsewhere, and adjustment disorders. | |||||||
| Mean age in years at last admission | 2,597 | 768 | (46.2, 15.8) | 196 | (42.7, 16.2) | 1,633 | (52, 19.5) |
| Sex | |||||||
| Males | 1,343 | 369 | 47.8 | 77 | 39.3 | 897 | 54.9 |
| Females | 1,254 | 399 | 52.2 | 119 | 60.7 | 736 | 45.1 |
| Marital status | |||||||
| Married | 782 | 229 | 29.8 | 58 | 29.6 | 495 | 30.3 |
| Source of income | |||||||
| Employed | 498 | 176 | 22.9 | 44 | 22.4 | 278 | 17 |
| Pension | 787 | 165 | 21.5 | 46 | 23.5 | 576 | 35.3 |
| Other income | 1,364 | 440 | 57.3 | 109 | 55.6 | 815 | 49.9 |
| DSM-IV diagnoses | |||||||
| Mental disorder due to general medical condition | 52 | 8 | 1 | 2 | 1 | 42 | 2.6 |
| Substance use disorders | 426 | 157 | 20.4 | 44 | 22.4 | 225 | 13.8 |
| Schizophrenia and other psychotic disorders | 736 | 103 | 13.4 | 42 | 21.4 | 591 | 36.2 |
| Mood disorders | 1,410 | 526 | 68.5 | 128 | 65.3 | 756 | 46.3 |
| Anxiety disorders | 211 | 55 | 7.2 | 19 | 9.7 | 137 | 8.4 |
| Personality disorders | 263 | 135 | 17.6 | 27 | 13.8 | 101 | 6.2 |
| Adjustment disorder | 148 | 78 | 10.2 | 11 | 5.6 | 59 | 3.6 |
| Childhood disorder | 47 | 14 | 1.8 | 9 | 4.6 | 24 | 1.5 |
| Delirium disorder | 247 | 16 | 2.1 | 11 | 5.6 | 220 | 13.5 |
| Dissociative disorder | 3 | 1 | 0.13 | 0 | 0 | 2 | 0.1 |
| Eating disorder | 15 | 5 | 0.7 | 2 | 1 | 8 | 0.5 |
| Factitious disorder | 2 | 0 | 0 | 0 | 0 | 2 | 0.1 |
| Impulse disorder | 27 | 10 | 1.3 | 2 | 1 | 15 | 0.9 |
| Sexual and gender disorder | 5 | 1 | 0.13 | 1 | 0.5 | 3 | 0.2 |
| Sleep disorder | 14 | 1 | 0.13 | 0 | 0 | 13 | 0.8 |
| Somatoform disorder | 11 | 3 | 0.4 | 1 | 0.5 | 7 | 0.4 |
| Other disorder | 504 | 126 | 16.4 | 35 | 17.9 | 343 | 21 |
Prediction Mode
Derivation Analysis
Derivation analysis results are summarized in Table 2. The full candidate model included age categories listed in Table 2 in reference to the youngest age group (18–24 years). We identified statistically important categories where risk is significantly different. The final model included age categories: 60–69 (aOR = 0.74, 95% CI = 0.73–0.76), 70–79 (aOR = 0.45, 95% CI = 0.44–0.46), and 80+ (aOR = 0.31, 95% CI = 0.30–0.31). The final model also included psychiatric disorders: substance use (aOR = 1.30, 95% CI = 1.27–1.32), mood (aOR = 1.49, 95% CI = 1.47–1.52), personality (aOR = 2.30, 95% CI = 2.25–2.36), psychiatric disorders due to general medical condition (aOR = 0.52, 95% CI = 0.50–0.55), and schizophrenia (aOR = 0.42, 95% CI = 0.41–0.43).
Table 2. Full candidate predictive and final model results for lifetime history of self-harm (regardless of intent to die).
| Full model | Final model | |
|---|---|---|
| Demographic and clinical characteristics | aOR, [95% CI] | aOR, [95% CI] |
| Note. Exponentiated coefficients; 95% confidence intervals in brackets. Marital status (1 with partner, 0 without) is dichotomized as either with (married or identified significant partner) or without (never married, widowed, separated, divorced) a significant partner. Other income includes: social assistance, disability insurance, employment insurance, other or no income. Other disorders include disorders of childhood/adolescence, cognitive disorders, somatoform disorders, factitious disorders, dissociative disorders, sexual and gender identity disorders, eating disorders, sleep disorders, impulse-control disorders not classified elsewhere, and adjustment disorders. * p ≤ .05. ** p ≤ .01. *** p ≤ .001. + trend p ≤ .10. | ||
| Sex (male) | 0.81* | – |
| [0.67–0.98] | ||
| Marital status | 0.87 | – |
| [0.71–1.08] | ||
| Employed | 0.99 | – |
| [0.75–1.31] | ||
| Other sources of income | 1.05 | – |
| [0.84–1.32] | ||
| Age 18–24 years (reference) | 1 | – |
| [1.00–1.00] | ||
| 25–29 | 1.01 | – |
| [0.69–1.48] | ||
| 30–39 | 1.23 | – |
| [0.89–1.70] | ||
| 40–49 | 1.29 | – |
| [0.95–1.76] | ||
| 50–59 | 1.06 | – |
| [0.78–1.43] | ||
| 60–69 | 0.85 | 0.74** |
| [0.59–1.22] | [0.73–0.76] | |
| 70–79 | 0.51** | 0.45** |
| [0.32–0.83] | [0.44–0.46] | |
| 80+ | 0.34** | 0.31** |
| [0.22–0.55] | [0.30–0.31] | |
| Psychiatric disorder due to general medical condition | 0.52+ | 0.52** |
| [0.25–1.09] | [0.50–0.55] | |
| Substance use disorder | 1.34* | 1.30** |
| [1.04–1.73] | [1.27–1.32] | |
| Schizophrenia | 0.43** | 0.42** |
| [0.32–0.57] | [0.41–0.43] | |
| Mood disorders | 1.53** | 1.49** |
| [1.19–1.96] | [1.47–1.52] | |
| Anxiety disorder | 0.86 | – |
| [0.61–1.22] | ||
| Personality disorders | 2.19** | 2.30** |
| [1.61–2.99] | [2.25–2.36] | |
| Other disorders | 1.09 | – |
| [0.82–1.44] | ||
| Observations | 1,925 | 1,928 |
Self-Harm Behavior Risk Score
The sum of the weights of the final risk score ranges from a minimum of −9 (lowest risk) to a maximum of +5 (highest risk; (see Table 3). A score of 5 corresponds to a 97% predicted probability of self-harm, while a score of −4 or less corresponds to 0% (Table 4).
Table 3. Final risk score for predicting a lifetime history of self-harm with or without intent to die.
| Protective factors | Score | Risk factors | Score |
|---|---|---|---|
| Age 60–69 | −1 | Substance abuse | +1 |
| 70–79 | −3 | Mood disorder | +1 |
| 80+ | −4 | Personality disorder | +3 |
| Schizophrenia | −3 | ||
| General medical disorder | −2 |
Table 4. The predicted probability of a history of self-harm associated with possible total score values.
| Total score | Predicted probability of a history of self-harm | |
|---|---|---|
| Note. Final prediction score and corresponding predicted probabilities of lifetime history of self-harm (regardless of intent to die). | ||
| High risk | 5 | 97% |
| 4 | 91% | |
| 3 | 80% | |
| 2 | 59% | |
| Medium risk | 1 | 35% |
| 0 | 16% | |
| Low risk | −1 | 7% |
| −2 | 3% | |
| −3 | 1% | |
| −4 or lower | 0% |
Performance of the Risk Score
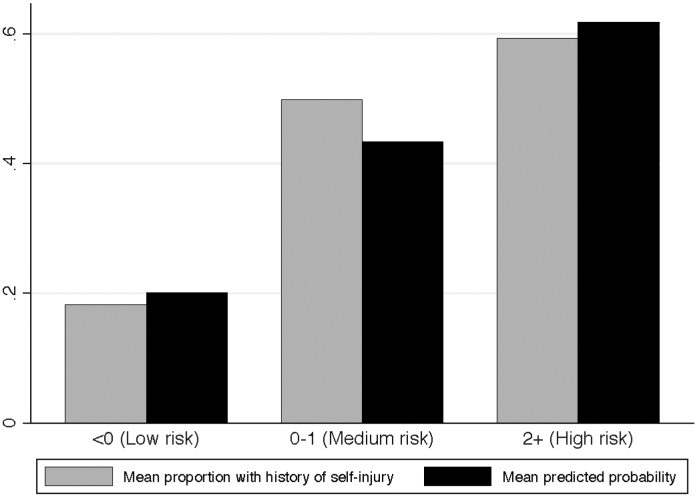
The Hosmer–Lemmeshow goodness-of-fit test was not significant in the derivation or validation sample (p > .05 in both) and the Brier score was .21 and .20 in the derivation and validation samples, respectively. These statistics indicate good agreement between our predicted probabilities and the observed proportion of people with history of self-harm (regardless of intent to die). The C statistic was .70 in the derivation sample (95% CI = .68–.72) and .71 in the validation sample (95% CI = .67–.75) indicating a reasonable ability of the model to discriminate between people with lifetime history of self-harm and those without. Figure 1 shows a close relationship between the observed proportion of people with a history of self-harm and our score's predicted probabilities in the validation set. These performance results remained nearly identical in sensitivity analyses where we used our final score to predict self-harm behavior (with or without intent to die) within the previous year and month. The score also performed identically when tested for predicting self-harm with intent to die. It performed substantially worse (C statistic = .61) for predicting self-harm without intent to die. Thus, we conducted additional analysis to decompose the predictors of suicidal and nonsuicidal self-harm separately. Figure SF2 in Electronic Supplementary Material 2 (72.8KB, pdf) presents the decision curve analysis for the final score tested in the validation sample. After a threshold probability of approximately 17%, using the score offers increasing net benefit compared with a policy of acting on every patient.
Figure 1. Distribution of predicted and observed risk per category of risk score in the validation sample (n = 674).
The results of the subgroup analysis testing the influence of intent to die on the predictors of self-harm using the full candidate model are summarized in Table S1 (see Electronic Supplementary Material 3 (103.4KB, pdf) ). We found no major differences in the trends of our predictors of suicidal and nonsuicidal self-harm behavior. However, the reporting of personality disorder (aOR = 1.06, 95% CI = 0.67–1.66), schizophrenia (aOR = 0.99, 95% CI = 0.60–1.61), anxiety (aOR = 1.09, 95% CI = 0.65–1.81), and psychiatric disorder due to general medical conditions (aOR = 0.62, 95% CI = 0.15–2.62) lost significance in the self-harm without intent to die model. Mood disorders (OR = 1.51, 95% CI = 0.99–2.32) showed a trend among participants reporting self-harm without intent to die. Since these groups (self-harm separated by intent to die) were largely indistinguishable, we built our single model using the combined populations.
Discussion
Findings from this study revealed over a third of psychiatric inpatients report a history of self-harm. While the majority of patients reported self-harm with the intent to die, intent did not influence the risk predictors. Younger age, substance use, mood, and personality disorders conferred increased risk for self-harm behavior, while schizophrenia and psychiatric disorder due to general medical condition were associated with lower risk within this sample of psychiatric inpatients. These results suggest the risk factors of self-harm are static and may represent a stable trait not related to timing of the self-harm event within the psychiatric inpatient population.
While over 60% of the high-risk patients reported a lifetime history of self-harm, we observed a 10–20% risk of lifetime self-harm even in patients at the lowest predicted risk category. This reflects the expected yet high baseline prevalence of such behavior in our psychiatric sample. Even this "low" risk is substantial and may justify intensive screening, especially because the overwhelming majority of people with a history of self-harm intended to die.
The similarities of risk factors between patients self-harming and those attempting suicide is an important finding from this paper. Whereas the implications for clinical management of the patient would suggest we prolong patient stay for those attempting suicide, the findings from this study would suggest similar risk factors exist between both patients and should be considered closer. The risk model constructed in this study is not able to directly estimate risk of future self-harm behavior, a cohort study design will be more appropriate, yet infeasible, to predict future self-harm. Clinically, it may be useful for determining whether more intensive screening is appropriate for a patient who reports no history of self-harm behavior but is categorized by the model as likely to be at risk. It can also be used for statistical risk adjustment in observational studies conducted with datasets that do not contain data on history of self-harm, or to construct eligibility criteria for entering high-risk participants into randomized controlled trials.
Uncovering Clinical and Demographic Predictors
Risk factors for suicidal behavior among the general population have been well investigated, where the majority of research has focused on the impact of different psychiatric disorders on suicide and self-harm (Mann, 2003). However, much of the research has been limited in distinguishing the risk for suicide and self-harm among patients with serious psychiatric disorders requiring inpatient treatment. Understanding the factors associated with suicide among the highest risk populations is a difficult task that has yet to be adequately addressed. Here, we have presented the results outlining the clinical and demographic characteristics that assist in predicting suicidal and nonsuicidal self-harm behaviors. These results should not be surprising to the clinical audience, since previous studies have consistently demonstrated a positive association between SAs and psychiatric disorders (Mann, 2003). Beautrais and colleagues report that 90% of people that died by suicide were diagnosed with a psychiatric disorder, including depression, substance use, and borderline personality disorders (Beautrais et al., 1996). Many studies reported a positive link between an increased risk for SA and the diagnosis of major depression (Kosaraju et al., 2015; Teti et al., 2014). In our study we found that mood disorders are significantly associated with history of self-harm behavior. Although depression is a strong predictor of the onset of suicidal thoughts it does not predict further progression toward SA (Nock et al., 2008). Nock et al. suggest that disorders associated with anxiety/agitation and poor impulse control are stronger predictors of SAs (Nock et al., 2008). Stronger associations have been found between SAs and bipolar disorder than with any other psychiatric diagnosis (Zimmerman et al., 2013).
Substance use disorders are also highly prevalent among people with a history of suicidal behavior (Borges et al., 2006; Kausch & McCormick, 2002; Mann et al., 2005; Preuss et al., 2002; Rossow & Amundsen, 1995). Studies show completed suicide is associated with substance use behavior; one study found that out of a total of 248 suicide completers, 16 occurred among patients receiving substance use treatment and the majority (63%) of SAs occurred among patients with alcohol dependence (Kausch & McCormick, 2002). In a study of completed suicide, Kolves et al. found that among 427 suicides, 51% suffered from concurrent alcohol dependence (Kolves, Varnik, Tooding, & Wasserman, 2006).
Studies also report a positive association between borderline personality disorder and SAs (Zimmerman et al., 2013). In the current study we combined all personality disorder categories owing to sample size constraints and found a significant association between any personality disorder and increased risk of suicidal behavior.
In this study, schizophrenia was inversely associated with history of self-harm behavior. Previous studies report that patients with schizophrenia have a higher incidence of suicidal behavior than the general population (Kreyenbuhl, Kelly, & Conley, 2002; Singhal, Ross, Seminog, Hawton, & Goldacre, 2014). Suicide is a major cause of death among patients with schizophrenia (Gomez-Duran, Martin-Fumado, & Hurtado-Ruiz, 2012), yet there are often large differences between these patients and patients with other psychiatric diagnoses. Patients with schizophrenia frequent emergency rooms and health facilities at a higher rate than patients with other psychiatric disorders do (Hansen & Elliott, 1993). This contact with the health-care system may be of particular importance, because chronic disorders that require frequent care offer an opportunity for intervention and prevention of detrimental behavior. Our study was conducted in a psychiatric population. Patients with schizophrenia may be at lower risk of self-injurious behavior compared with others admitted to a psychiatric hospital, but we would not expect this to be true when comparing them with the general population.
Patients with psychiatric disorders due to a general medical condition were less likely to report a history of self-injury. These patients do not carry primary psychiatric diagnoses and their symptomatology is a by-product of other medical problems. Patients with multiple sclerosis, for example, have behavioral manifestations of cognitive and emotional disturbances, which can be interpreted as a psychiatric condition (Mahler, 1992). Other conditions, such as hyperthyroidism and Graves' disease, may present with psychiatric symptoms (Brandt et al., 2013). Owing to their extreme deviation from the normal range of psychiatric pathology, patients identified as having psychiatric disorder due to general medical condition should be considered different from the remainder of the psychiatric population.
We found that among patients with psychiatric disorders, older patients were less likely to report a history of self-harm and this is consistent with previous research (Maniam et al., 2014). Also consistent with the literature, we found that women were at higher risk for self-harm (Beautrais, Wells, McGee, & Oakley Browne, 2006; Kosaraju et al., 2015). Our sensitivity analyses of 30-day and 1-year history of both self-harm and SA found the same risk factors as our primary lifetime history analysis. Future studies exploring suicidal behavioral risk factors may consider including subjects with any history of SA or self-harm since valid conclusions can be drawn across any type of suicidal or self-harm behavior.
Limitations
The use of retrospectively collected data from patient medical records is a limitation of this study. Data collected from administrative sources are highly susceptible to misclassification, and a recent study examining the misclassification of psychiatric disorders based on the comparison of medical records and administrative data shows moderate agreement for any mental comorbidity (Marrie et al., 2013). While we acknowledge that psychiatric diagnoses are not well collected from the review of general medical records, the collection of data for this study was limited to the medical records of patients admitted to a specialized psychiatric hospital. We are more confident about the collection of diagnosis information from these patients, largely because they require a psychiatric reason for hospital admission. In addition, we provided well-trained nurses with piloted tested data extraction forms, using only variables that would have minimal chance for misclassification in our analyses.
Conclusion
Findings from this study indicate intent to die was not associated with any specific risk factors; in fact any self-harm is increased in younger patients with diagnosed substance use, mood, or personality disorders. Within the psychiatric population, the risk factors of self-harm are static and may represent a stable trait not related to timing of the self-harm event. Retrospective lifetime probabilities of suicidal and nonsuicidal self-harm could be predicted by similar factors, and a model taking into account just a few factors could reliably estimate the probability of either event. Reliable estimation of the risk for these behaviors may help guide intensive screening and prevention efforts.
Electronic Supplementary Material
The electronic supplementary material is available with the online version of the article at http://dx.doi.org/10.1027/0227-5910/a000342
ESM 1. (249.4KB, pdf) Figure SF1. Patient recruitment diagram.
ESM 2. (72.8KB, pdf) Figure SF2. Decision curve analysis (validation sample, n = 674).
ESM 3 (103.4KB, pdf) . Table S1. Subgroup analysis for lifetime history of suicide attempt and lifetime history ofself-harm using full candidate model.
Acknowledgments
This work was supported by the Brain and Behavior Research Foundation Young Investigator Grant (# 19058).
Biographies
Dr. Brittany B. Dennis is a post-doctoral research fellow in the Peter Boris Centre for Addictions Research, St. Joseph's Healthcare Hamilton, and is an MBBS candidate at St. George's University of London, UK. Dr. Dennis holds the Intersections in Mental Health Perspectives and Addiction Research Training Fellowship supported by the Canadian Institutes of Health Research as well as the 2015 David L. Sackett Scholarship from the Department of Clinical Epidemiology and Biostatistics, McMaster University.
Pavel S. Roshanov is an MD candidate at the University of Western Ontario, Canada. He is also completing his doctoral training (PhD) in the Department of Clinical Epidemiology and Biostatistics at McMaster University, Canada. Pavel is supported by an American Society of Nephrology Medical Student Scholar Grant.
Dr. Monica Bawor is a post-doctoral research fellow in the Peter Boris Centre for Addictions Research, St. Joseph's Healthcare Hamilton, and is an MBBS candidate at St. George's University of London, UK. Dr. Bawor holds the Intersections in Mental Health Perspectives and Addiction Research Training Fellowship supported by the Canadian Institutes of Health Research.
Wala ElSheikh is a research assistant at the Population Health Research Institute, Hamilton, ON, Canada.
Sue Garton is a registered nurse working at St. Joseph's Healthcare Hamilton, ON, Canada, specializing in the care of psychiatric patients.
Nichole Hutchinson is a registered nurse working at St. Joseph's Healthcare Hamilton, ON, Canada, specializing in the care of psychiatric patients.
Elisabeth Lordan is a registered nurse working at St. Joseph's Healthcare Hamilton, ON, Canada, specializing in the care of psychiatric patients.
Judith Vair is a registered practical nurse working at St. Joseph's Healthcare Hamilton, ON, Canada, specializing in the care of psychiatric patients.
Heather Sholer is a registered practical nurse working at St. Joseph's Healthcare Hamilton, ON, Canada, specializing in the care of psychiatric patients.
Jane DeJesus is a researcher coordinator at the Population Health Research Institute, Hamilton, ON, Canada.
Sumathy Rangarajan is a program manager at the Population Health Research Institute, Hamilton, ON, Canada. She holds both a Bachelor of Science Degree and a Master of Science Degree from Pune University, India.
Dr. Lehana Thabane is a senior research methodologist with research interests in the development and application of statistical methods health research. Dr. Thabane is a professor and the associate chair of the Department of Clinical Epidemiology and Biostatistics at McMaster University, Canada.
Dr. Zainab Samaan is an associate professor, Department of Psychiatry and Behavioral Neurosciences, and associate faculty, Population Genomics Program, McMaster University, Canada. Dr. Samaan is also a staff psychiatrist, member of the Royal College of Psychiatrists, UK, and a certified academic psychiatrist by the College of Physicians and Surgeons of Ontario, Canada.
References
- Babyak M. A. (2004). What you see may not be what you get: A brief, nontechnical introduction to overfitting in regression-type models. Psychosomatic Medicine, (3), 411–421. [DOI] [PubMed] [Google Scholar]
- Beautrais A. L., Joyce P. R., Mulder R. T., Fergusson D. M., Deavoll B. J., & Nightingale S. K. (1996). Prevalence and comorbidity of mental disorders in persons making serious suicide attempts: A case-control study. American Journal of Psychiatry, (8), 1009–1014. [DOI] [PubMed] [Google Scholar]
- Beautrais A. L., Wells J. E., McGee M. A., & Oakley Browne M. A. (2006). Suicidal behaviour in Te Rau Hinengaro: The New Zealand Mental Health Survey. The Australian and New Zealand Journal of Psychiatry, (10), 896–904 10.1111/j.1440-1614.2006.01909.x [DOI] [PubMed] [Google Scholar]
- Blumenthal S., Bell V., Neumann N. U., Schuttler R., & Vogel R. (1989). Mortality and rate of suicide of first admission psychiatric patients. A 5-year follow-up of a prospective longitudinal study. Psychopathology, (1), 50–56. [DOI] [PubMed] [Google Scholar]
- Borges G., Angst J., Nock M. K., Ruscio A. M., Walters E. E., & Kessler R. C. (2006). A risk index for 12-month suicide attempts in the National Comorbidity Survey Replication (NCS-R). Psychological Medicine, (12), 1747–1757 10.1017/s0033291706008786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandt F., Thvilum M., Almind D., Christensen K., Green A., Hegedus L., & Brix T. H. (2013). Hyperthyroidism and psychiatric morbidity. Evidence from a Danish nation-wide register study. European Journal of Endocrinology, , 341–348 10.1530/eje-13-0708 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2015). Definitions: Self-directed violence. Injury prevention and control: Division of violence. Retrieved from http://www.cdc.gov/violenceprevention/suicide/definitions.html
- DeLeo D., Bertolote J., & Lester D. (2002). Self-directed violence In Krug E. G., Dahlberg L. L., Mercy J. A., Zwi A. B., & Lozano R. (Eds.), World report on violence and health (pp. 183–240). Geneva, Switzerland: World Health Organization. [Google Scholar]
- Ekramzadeh S., Javadpour A., Draper B., Mani A., Withall A., & Sahraian A. (2012). Prevalence and correlates of suicidal thought and self-destructive behavior among an elderly hospital population in Iran. International Psychogeriatrics, (9), 1402–1408 10.1017/s1041610212000245 [DOI] [PubMed] [Google Scholar]
- Furlanetto L. M., & Stefanello B. (2011). Suicidal ideation in medical inpatients: Psychosocial and clinical correlates. General Hospital Psychiatry, (6), 572–578 10.1016/j.genhosppsych.2011.08.002 [DOI] [PubMed] [Google Scholar]
- Gomez-Duran E. L., Martin-Fumado C., & Hurtado-Ruiz G. (2012). Clinical and epidemiological aspects of suicide in patients with schizophrenia. Actas Españolas Psiquiatria, (6), 333–345. [PubMed] [Google Scholar]
- Hansen T. E., & Elliott K. D. (1993). Frequent psychiatric visitors to a Veterans Affairs medical center emergency care unit. Hospital and Community Psychiatry, (4), 372–375. [DOI] [PubMed] [Google Scholar]
- Harrell F. E. (2014). rms: Regression modeling strategies R package (version 4.1-1). Retrieved from http://CRAN.R-project.org/package=rms
- Harrell F. E., Jr., Lee K. L., & Mark. D. B. (1996). Multivariable prognostic models: Issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Statistics in Medicine, (4), 361–387. [DOI] [PubMed] [Google Scholar]
- Kausch O., & McCormick R. A. (2002). Suicide prevalence in chemical dependency programs: Preliminary data from a national sample, and an examination of risk factors. Journal of Substance Abuse Treatment, (2), 97–102. [DOI] [PubMed] [Google Scholar]
- Kerr P. L., Muehlenkamp J. J., & Turner J. M. (2010). Nonsuicidal self-injury: A review of current research for family medicine and primary care physicians. Journal of the American Board of Family Medicine, (2), 240–259 10.3122/jabfm.2010.02.090110 [DOI] [PubMed] [Google Scholar]
- Kolves K., Varnik A., Tooding L. M., & Wasserman D. (2006). The role of alcohol in suicide: A case-control psychological autopsy study. Psychological Medicine, (7), 923–930 10.1017/s0033291706007707 [DOI] [PubMed] [Google Scholar]
- Kosaraju S. K., Vadlamani L. N., Mohammed Bashir M. S., Kalasapati L. K., Rao G. L., & Rao G. P. (2015). Risk factors for suicidal attempts among lower socioeconomic rural population of telangana region. Indian Journal of Psychological Medicine, (1), 30–35 10.4103/0253-7176.150813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreyenbuhl J. A., Kelly D. L., & Conley R. R. (2002). Circumstances of suicide among individuals with schizophrenia. Schizophrenia Research, (2–3), 253–261. [DOI] [PubMed] [Google Scholar]
- Linehan M. M., Goodstein J. L., Nielsen S. L., & Chiles J. A. (1983). Reasons for staying alive when you are thinking of killing yourself: The reasons for living inventory. Journal of Consulting and Clinical Psychology, (2), 276–286. [DOI] [PubMed] [Google Scholar]
- Mahler M. E. (1992). Behavioral manifestations associated with multiple sclerosis. The Psychiatric Clinics of North America, (2), 427–438. [PubMed] [Google Scholar]
- Maniam T., Marhani M., Firdaus M., Kadir A. B., Mazni M. J., Azizul A., … Noor Ani A. (2014). Risk factors for suicidal ideation, plans and attempts in Malaysia – results of an epidemiological survey. Comprehensive Psychiatry, (Suppl. 1), S121–125 10.1016/j.comppsych.2013.08.004 [DOI] [PubMed] [Google Scholar]
- Mann J. J. (2003). Neurobiology of suicidal behaviour. Nature Reviews Neuroscience, (10), 819–828 10.1038/nrn1220 [DOI] [PubMed] [Google Scholar]
- Mann J. J., Apter A., Bertolote J., Beautrais A., Currier D., Haas A., … Hendin H. (2005). Suicide prevention strategies: A systematic review. JAMA, (16), 2064–2074 10.1001/jama.294.16.2064 [DOI] [PubMed] [Google Scholar]
- March J., Sareen J., Gawaziuk J. P., Doupe M., Chateau D., Hoppensack M., … Logsetty S. (2014). Increased suicidal activity following major trauma: A population-based study. The Journal of Trauma and Acute Care Surgery, (1), 180–184 10.1097/TA.0b013e3182a900bc [DOI] [PubMed] [Google Scholar]
- Marrie R. A., Fisk J. D., Yu B. N., Leung S., Elliott L., Caetano P., … Patten S. B. (2013). Mental comorbidity and multiple sclerosis: validating administrative data to support population-based surveillance. BMC Neurology, , 16. 10.1186/1471-2377-13-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modestin J., Zarro I., & Waldvogel D. (1992). A study of suicide in schizophrenic in-patients. British Journal of Psychiatry, , 398–401. [DOI] [PubMed] [Google Scholar]
- Mok C. C., Chan K. L., Cheung E. F., & Yip P. S. (2013). Suicidal ideation in patients with systemic lupus erythematosus: Incidence and risk factors. Rheumatology (Oxford), , 714–721 10.1093/rheumatology/ket404 [DOI] [PubMed] [Google Scholar]
- Moons K. G., Donders A. R., Steyerberg E. W., & Harrell F. E. (2004). Penalized maximum likelihood estimation to directly adjust diagnostic and prognostic prediction models for overoptimism: A clinical example. Journal of Clinical Epidemiology, (12), 1262–1270 10.1016/j.jclinepi.2004.01.020 [DOI] [PubMed] [Google Scholar]
- Moons K. G., Harrell F. E., & Steyerberg E. W. (2002). Should scoring rules be based on odds ratios or regression coefficients? Journal of Clinical Epidemiology, (10), 1054–1055. [DOI] [PubMed] [Google Scholar]
- Murray C., Lopez A., Rodgers A., Vaughan P., Prentice T., Edejer T. T., … Lowe J. (2002). Quantifying selected major risks to health In Campanini B. (Ed.), The world health report 2002 – Reducing risks, promoting healthy life (p. 80). Geneva, Switzerland: World Health Organization. [Google Scholar]
- Newson R. (2006). Efficient calculation of jackknife confidence intervals for rank statistics. Journal of Statistical Software, , 1–10. [Google Scholar]
- Nock M. K., Borges G., Bromet E. J., Cha C. B., Kessler R. C., & Lee S. (2008). Suicide and suicidal behavior. Epidemiologic Review, , 133–154 10.1093/epirev/mxn002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell J., Geddes J., Deeks J., Goldacre M., & Hawton K. (2000). Suicide in psychiatric hospital in-patients. Risk factors and their predictive power. British Journal of Psychiatry, , 266–272. [DOI] [PubMed] [Google Scholar]
- Preuss U. W., Schuckit M. A., Smith T. L., Danko G. P., Buckman K., Bierut L., … Reich T. (2002). Comparison of 3190 alcohol-dependent individuals with and without suicide attempts. Alcoholism, Clinical and Experimental Research, (4), 471–477. [PubMed] [Google Scholar]
- Rossow I., & Amundsen A. (1995). Alcohol abuse and suicide: A 40-year prospective study of Norwegian conscripts. Addiction, (5), 685–691. [DOI] [PubMed] [Google Scholar]
- Roy A., & Draper R. (1995). Suicide among psychiatric hospital in-patients. Psychological Medicine, (1), 199–202. [DOI] [PubMed] [Google Scholar]
- Schroeder M. A. (1990). Diagnosing and dealing with multicollinearity. Western Journal of Nursing Research, (2), 175–184; discussion 184–177. [DOI] [PubMed] [Google Scholar]
- Sharma V., Persad E., & Kueneman K. (1998). A closer look at inpatient suicide. Journal of Affective Disorders, (1–3), 123–129. [DOI] [PubMed] [Google Scholar]
- Singhal A., Ross J., Seminog O., Hawton K., & Goldacre M. J. (2014). Risk of self-harm and suicide in people with specific psychiatric and physical disorders: Comparisons between disorders using English national record linkage. Journal of the Royal Society of Medicine, (5), 194–204 10.1177/0141076814522033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sokero T. P., Melartin T. K., Rytsala H. J., Leskela U. S., Lestela-Mielonen P. S., & Isometsa E. T. (2003). Suicidal ideation and attempts among psychiatric patients with major depressive disorder. Journal of Clinical Psychiatry, (9), 1094–1100. [DOI] [PubMed] [Google Scholar]
- Stata Statistical Software (Release 12) [Computer software] College Station, TX: StataCorp LP. [Google Scholar]
- Steyerberg E. W., Eijkemans M. J., Harrell F. E. Jr., & Habbema J. D. (2001). Prognostic modeling with logistic regression analysis: In search of a sensible strategy in small data sets. Medical Decision Making, (1), 45–56. [DOI] [PubMed] [Google Scholar]
- Sullivan L. M., Massaro J. M., & D'Agostino R. B. Sr. (2004). Presentation of multivariate data for clinical use: The Framingham Study risk score functions. Statistics in Medicine, (10), 1631–1660 10.1002/sim.1742 [DOI] [PubMed] [Google Scholar]
- Team R. C. (2013). R: A language and environment for statistical computing [Computer software] Vienna, Austria: R Foundation for Statistical Computing; Retrieved from http://www.R-project.org/. [Google Scholar]
- Teti G. L., Rebok F., Rojas S. M., Grendas L., & Daray F. M. (2014). Systematic review of risk factors for suicide and suicide attempt among psychiatric patients in Latin America and Caribbean. Revista Panamericana De Salud Publica, (2), 124–133. [PubMed] [Google Scholar]
- Vickers A. J., Cronin A. M., Elkin E. B., & Gonen M. (2008). Extensions to decision curve analysis, a novel method for evaluating diagnostic tests, prediction models and molecular markers. BMC Medical Informatics and Decision Making, , 53. 10.1186/1472-6947-8-53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vickers A. J., & Elkin E. B. (2006). Decision curve analysis: A novel method for evaluating prediction models. Medical Decision Making, (6), 565–574 10.1177/0272989x06295361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Elm E., Altman D. G., Egger M., Pocock S. J., Gotzsche P. C., & Vandenbroucke J. P. (2007). The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet, (9596), 1453–1457 10.1016/s0140-6736(07)61602-x [DOI] [PubMed] [Google Scholar]
- Zimmerman M., Martinez J., Young D., Chelminski I., Morgan T. A., & Dalrymple K. (2013). Comorbid bipolar disorder and borderline personality disorder and history of suicide attempts. Journal of Personality Disorders, , 358–364 10.1521/pedi_2013_27_122 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The electronic supplementary material is available with the online version of the article at http://dx.doi.org/10.1027/0227-5910/a000342
ESM 1. (249.4KB, pdf) Figure SF1. Patient recruitment diagram.
ESM 2. (72.8KB, pdf) Figure SF2. Decision curve analysis (validation sample, n = 674).
ESM 3 (103.4KB, pdf) . Table S1. Subgroup analysis for lifetime history of suicide attempt and lifetime history ofself-harm using full candidate model.