Abstract
A majority of acute pericarditis cases have some degree of myocarditis. Viruses are the common etiological factor of this disease. Corticosteroids are considered for treatment, especially in recurrent models of the disease. In this article, we report the case of a 47-year-old man with myopericarditis who was under daily intra-muscular dexamethasone injection for an unknown reason. This is a unique case of spontaneous myopericarditis under corticosteroid abuse that has not been reported previously.
Keywords: Myopericarditis, Corticosteroids
In the majority of cases, acute pericarditis has some degree of myocarditis because viruses are the common etiological factor for both diseases [1]. History of a febrile syndrome accompanied by pleuritic chest pain, fatigue, and decreased exercise capacity is the most common scenario for this disease. Principle findings on electrocardiogram (ECG) are diffuse ST-elevation (typically concave up) and depression of the PR segment, especially in V5 and V6 leads. High levels of Troponin and CK-MB due to myocardial injury are detected in laboratory findings. Nonsteroidal Anti-inflammatory Drugs (NSAIDs) are the cornerstone of therapy. Besides conventional treatments, colchicine also has positive effects. Due to their anti-inflammatory effects, corticosteroids should be considered in treatment, especially for recurrent models of the disease [2]. Herein, we report a unique spontaneous case of myopericarditis in a patient subjected to corticosteroid therapy.
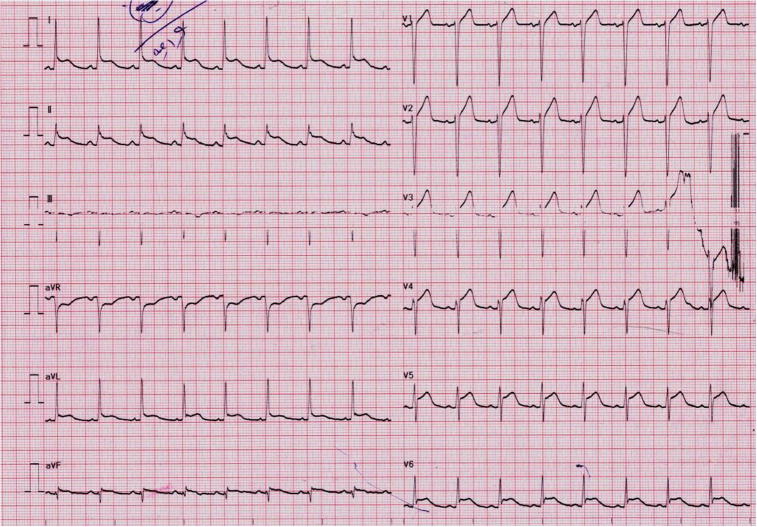
A 47-year-old man presented at the emergency department with acute left hemithorax pain and dyspnea. Bending forward was the only condition which improved his pain. No cardiac risk factor, such as diabetes mellitus, hypertension or smoking were found in his medical history. Over a period of four months, he was self-administering daily intra-muscular dexamethasone injections without physician prescription. Lower extremities had 3+ pitting edema. His electrocardiogram showed diffused ST-elevation in all leads except in V1 and aVR (Fig. 1). Cardiac Troponin I was positive for three times at the ranges of 2.86, 2.68 and 1.89, respectively (normal ⩽0.01). Echocardiography revealed mild to moderate pericardial effusion with lateral and posterior wall hypokinesia. No valvular involvement was seen. Pulmonary artery pressure was about 25 mmHg. Ejection fraction was estimated at 25–30%. Ibuprofen 600 mg three times a day along with heart failure treatment (ACEI/ARB, B-blocker) was started, stress dose of corticosteroid was administered and dexamethasone was tapered. Dramatic response was seen after two days. This patient underwent coronary angiography, and no significant lesion was noted. Workup was performed to rule out secondary causes for myopericarditis. All, including Antinuclear Antibody (ANA), double stranded DNA (dsDNA), Rheumatoid Factor (RF), Cyclic Citrullinated Peptide Antibody (AntiCCP), Perinuclear Anti-Neutrophil Cytoplasmic Antibody (P-ANCA) and Antineutrophil cytoplasmic antibody (C-ANCA), were in normal range or negative. Ferritin level, TFT, serum and urine electrophoresis were also in normal range. PPD test was negative. After two years’ follow up, echocardiography revealed ejection fraction at 35–40%. No recurrence was seen to present day.
Figure 1.
Diffused ST-elevation in a patient with acute chest pain.
The past decades have seen steroids being utilized for the prevention of myopericarditis relapse. The main mechanism is not well understood but it seems that immune modulation and suppression induced by corticosteroids play a crucial role [3]. In NSAID-resistant patients and in relapsing cases, corticosteroids should be considered. Recent recommendations limit the role of corticosteroids due to the lack of clinical evidence regarding medium and long-term benefits [4]. The use of corticosteroid therapy for recurring pericarditis is supported solely by a retrospective study [3]. Some studies have demonstrated that high dose corticosteroid not only leads to major side effects, but also to hospitalization and recurrent pericarditis. As corticosteroids promote viral replication, they have been reported as independent risk factors for further recurrences in the first episode or after two or more recurrences [5]. In our case, all secondary reasons for myopericarditis were assessed, and no specific etiology was found. Coronary angiography revealed normal findings. With echocardiography, and electrocardiographic and cardiac injury markers, myopericarditis was the first diagnosis for our patient. As our patient was under dexamethasone for four months, we expected that in a previously healthy individual under dexamethasone, pericarditis would occur in a subtle form or would not occur due to anti-inflammatory effects. It seems that corticosteroids are not an effective therapy for acute myopericarditis or may be an etiology for myopericarditis. Also corticosteroids can be considered an exacerbating agent in this case. When the immune response is suppressed by dexamethasone, cardiotropic viruses involve the pericardium and myocardium by direct cytolytic or cytotoxic effects. Abnormal immune response triggered by the viruses or corticosteroids in the presence of a predisposing genetic background is the main mechanism of myocardial damage in the absence of a viral genome. After cessation of corticosteroid over two years, no recurrence was seen in our patient. This article is congruent with other studies against corticosteroid efficacy in myopericarditis. Although viral agents could not be ruled out, it seems that dexamethasone is an etiologic or exacerbating agent in our case. We recommend that corticosteroids be omitted from myopericarditis treatment lists. Nevertheless, larger controlled trials are needed to investigate the role of dexamethasone in acute myopericarditis.
Disclosure: Author has nothing to disclose with regard to commercial support.
Footnotes
Peer review under responsibility of King Saud University.
References
- 1.Maisch B., Seferović P.M., Ristić A.D., Erbel R., Rienmüller R., Adler Y. Guidelines on the diagnosis and management of pericardial diseases executive summary; the task force on the diagnosis and management of pericardial diseases of the European Society of Cardiology. Eur Heart J. 2004;25(7):587–610. doi: 10.1016/j.ehj.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 2.Lange R.A., Hillis L.D. Clinical practice. Acute pericarditis. N Engl J Med. 2004;351(21):2195–2202. doi: 10.1056/NEJMcp041997. [DOI] [PubMed] [Google Scholar]
- 3.Marcolongo R., Russo R., Laveder F., Noventa F., Agostini C. Immunosuppressive therapy prevents recurrent pericarditis. J Am Coll Cardiol. 1995;26(5):1276–1279. doi: 10.1016/0735-1097(95)00302-9. [DOI] [PubMed] [Google Scholar]
- 4.Farand P., Bonenfant F., Belley-Côté E.P., Tzouannis N. Acute and recurring pericarditis: more colchicine, less corticosteroids. World J Cardiol. 2010;2(12):403–407. doi: 10.4330/wjc.v2.i12.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Artom G., Koren-Morag N., Spodick D.H., Brucato A., Guindo J., Bayes-de-Luna A. Pretreatment with corticosteroids attenuates the efficacy of colchicine in preventing recurrent pericarditis: a multi-centre all-case analysis. Eur Heart J. 2005;26(7):723–727. doi: 10.1093/eurheartj/ehi197. [DOI] [PubMed] [Google Scholar]