Abstract
Significant left main coronary artery (LMCA) stenosis is not rare and reported 3 to 10% of patients undergoing coronary angiography. Unprotected LMCA intervention is a still clinical challenge and surgery is still going to be a traditional management method in many cardiac centers. With a presentation of drug eluting stent (DES), extensive use of IVUS and skilled operators, number of such interventions increased rapidly which lead to change in recommendation in the guidelines regarding LMCA procedures in the stable angina (Class 2a recommendation for ostial and shaft lesion and class 2b recommendation for distal bifurcation lesion). However, there was not clear consensus about the management of unprotected LMCA lesion associated with acute myocardial infarction (MI) with a LMCA culprit lesion itself or distinct culprit lesion of other major coronary arteries. Surgery could be preferred as an obligatory management strategy even in the high risk patients. With this review, we aimed to demonstrate treatment strategies of LMCA disease associated with acute coronary syndrome, particularly acute myocardial infarction (MI). In addition, we presented a short case series with LMCA lesion and ST elevated acute MI in which culprit lesion placed either in the left anterior descending artery or circumflex artery. We reviewed the current medical literature and propose simple algorithm for management.
Abbreviations: CABG, coronary artery bypass graft; CX, circumflex artery; DES, drug-eluting stent; IVUS, intravascular ultrasonography; LAD, left anterior descending artery; LMCA, left main coronary artery; MI, myocardial infarction; PCI, percutaneous coronary interventions; RCA, right coronary artery; SYNTAX, synergy between percutaneous coronary intervention with TAXUS and cardiac surgery; TIMI, thrombolysis in myocardial infarction
Keywords: Left main coronary artery, Acute coronary syndrome, Surgery, Percutaneous intervention
Introduction
Significant left main coronary artery (LMCA) stenosis is not rare, occurring among a reported 3% to 10% of patients undergoing coronary angiography [1]. Unprotected LMCA intervention remains a clinical challenge. With the advent of drug-eluting stent (DES), extensive use of IVUS and skilled operators, the number of such interventions have increased rapidly, leading to changes in guideline recommendations for LMCA procedures in stable angina (Class 2a recommendation for ostial and shaft lesions and class 2b recommendation for distal bifurcation lesions) [2]. Moreover, isolated LMCA disease with low SYNTAX score (⩽22) was recommended as class 1 indication with the level of evidence of B in the recent revascularization guidelines of European Society of Cardiology. However, there was no clear consensus on unprotected LMCA lesions associated with acute myocardial infarction with culprit lesion of LMCA itself or distinct culprit lesion of other major coronary arteries [3–6].
This review sought to demonstrate the treatment strategies of LMCA disease associated with acute coronary syndromes, particularly acute myocardial infarction (MI). In addition, we present a short case series with an LMCA lesion and ST-elevated acute MI in which the culprit lesion was placed either in the left anterior descending artery (LAD) or circumflex artery (CX). We review the current medical literature and conclude with an algorithm for LMCA lesions associated with acute coronary syndromes.
Current management of left main coronary artery stenosis in stable angina
Surgery is accepted as a traditional and standard treatment of unprotected LMCA disease. Recent data comparing the safety and efficacy of LMCA interventions with DES and coronary artery bypass graft (CABG) surgery showed comparable results in terms of safety and mortality [2]. Long-term mortality rates were also similar. However, percutaneous coronary interventions (PCI) were associated with higher rates of repeat revascularization, whereas CABG was associated with higher stroke rate compared to PCI [7–10]. Patient selection for both strategies is fundamental and may directly impact clinical outcome. For this reason, LMCA disease management should be discussed extensively by the heart team prior to treatment. LMCA lesion >50% with documented ischemia or fractional flow reserve <0.80 for angiographic diameter stenosis between 50% and 70% and more than 70% stenosis of LMCA lesion should be revascularized for prognosis and improved survival. The current guidelines of the European Society of Cardiology on LMCA disease management in stable angina are summarized in Table 1 [11].
Table 1.
Indication for coronary bypass graft surgery vs. percutaneous coronary intervention in the stable angina patients with lesions suitable for both procedures.
| LMCA LESİON | Favours CABG | Favours PCI |
|---|---|---|
| ⁎Left main with SYNTAX score ⩽22 | 1 (Level of evidence – B) | 1 Level of evidence – B) |
| ⁎Left main with SYNTAX score 23–32 | 1 (Level of evidence – B) | 2a (Level of evidence – B) |
| ⁎Left main with SYNTAX score >32 | 1 (Level of evidence – B) | 3 (Level of evidence – B) |
| aLeft main (isolated or 1 VD, ostium/shaft) | 1 (Level of evidence – A) | 2a (Level of evidence – B) |
| aLeft main (isolated or 1 VD, distal bifurcation) | 1 (Level of evidence – A) | 2b (Level of evidence – B) |
| aLeft main + 2 VD or 3 VD, SYNTAX score ⩽32 | 1 (Level of evidence – A) | 2b (Level of evidence – B) |
| aLeft main + 2 VD or 3 VD, SYNTAX score ⩾33 | 1 (Level of evidence – A) | 3 (Level of evidence – B) |
LMCA, Left main coronary artery; CABG, Coronary artery bypass graft; PCI, Percutaneous coronary; VD, Vessel disease; SYNTAX, Synergy between percutaneous coronary intervention with taxus and cardiac surgery.
According to 2014 European Society of Cardiology Guidelines in Myocardial Revascularisation.
According to 2010 European Society of Cardiology Guidelines in Myocardial Revascularisation.
Left main coronary artery stenosis as a culprit lesion in the acute coronary syndromes
In patients with LMCA culprit lesions, the optimal revascularization strategy is not obvious [3–6]. Most patients usually present with hemodynamic instability and cardiogenic shock. Even after successful revascularization, the mortality rate is higher when compared to stable patients [12,13]. Treatment allocation is primarily determined by presentation with thrombolysis in myocardial infarction (TIMI) 0/1 flow. As percutaneous intervention offers an earlier restoration of TIMI flow, PCI could be the obligatory treatment strategy [14–16]. In the case of hemodynamic stability, treatment approach could either be PCI or surgery in parallel with guidelines for stable patients [4].
Multi-vessel disease with higher SYNTAX score (⩾33) could be a major candidate for bypass surgery [17,18], whereas higher operative risk assessed by euroSCORE and higher possibility of complete revascularization may require PCI [19] The following clinical variables were shown as prognostic factors in a LMCA culprit lesion:
-
–
Cardiogenic shock: a strong indicator of mortality [20], and associated with nearly fourfold increment in 30-day mortality (55% vs 15% in non-cardiogenic shock patients) [20]
-
–
ST-elevation MI is associated with higher periprocedural complications and higher six-month mortality compared to non-ST-elevation MI and unstable angina patients [1]
-
–
Initial TIMI 1/0 flow
-
–
Reduced left ventricular ejection fraction
-
–
Older age
-
–
Multi-vessel disease and high SYNTAX score
-
–
Diabetes mellitus.
Cardiogenic shock with isolated LMCA culprit lesion shows relatively better prognosis after successful primary PCI compared to multi-vessel disease. Such patients usually recover earlier from cardiogenic shock; and long-term prognosis is similar to non-cardiogenic shock patients in selected patient groups [21]. PCI should be preferred in the presence of the following clinical features:
-
–
Cardiogenic shock
-
–
Initial TIMI 1/0 flow
-
–
Isolated LMCA culprit lesion
-
–
Poor surgical candidate (high euroSCORE, distal coronary disease unfavorable to CABG or co-morbidity, including chronic obstructive lung disease and renal failure)
-
–
Favorable anatomy providing complete revascularization (low or intermediate SYNTAX score)
-
–
Patients with rudimentary circumflex artery
-
–
Advanced age (octogenarians).
In the following clinical settings with hemodynamic stability and low perioperative risk, CABG is a preferred option:
-
–
Concomitant valvular disease or mechanical complication
-
–
Heavy calcified LMCA disease
-
–
Multi-vessel disease with high SYNTAX score
-
–
Reduced left ventricular function
-
–
Diabetic patients.
Left main coronary artery stenosis as a non-culprit lesion in acute coronary syndromes
Concurrent LMCA and non-LMCA PCI has worse outcomes than isolated LMCA PCI [14]. Thus, it is logical to postpone LMCA revascularization if the culprit lesion is located in the right coronary artery (RCA). However, PCI of culprit lesion located either in LAD or CX in the presence of significant LMCA lesion is a hazardous clinical issue and may necessitate concurrent LMCA intervention. Short and long-term data on simultaneous PCI of LMCA and non-LMCA culprit vessel are not well-defined.
Short case series
Herein we describe our short case series and discuss treatment strategies. The cases described here were collected at the International Medicine Hospital of Kosovo. We performed 10 cases of ST-elevated MI with significant LMCA stenosis. Among them, five culprit lesions were located in LAD, two in CX and three in the RCA. We did not perform LMCA interventions with a culprit lesion of RCA in the same session. We initially performed three primary PCIs of RCAs, and we postponed LMCA interventions for elective procedures. In patients with culprit lesions located in the left coronary system, our primary goal was to open culprit lesions initially and then after myocardial salvation; and finally to perform LMCA intervention. In one patient with LAD lesion, LMCA stenosis was over the 95% which necessitated initial LMCA intervention. In all procedures, we used DES and LMCA intervention performed without IVUS support. We could not use IVUS due to affordability. Only one case pertained to distal LMCA bifurcation lesion; the rest were either ostial or shaft lesions. The mean euroSCORE value was 13.0. All patients were discharged without in-hospital complications, and control examinations at six months were uneventful.
This short series may indicate the feasibility of concurrent LMCA and non-LMCA culprit vessel interventions in selected patients. In the presence of the following clinical features, PCI may be the preferred option:
-
–
Cardiogenic shock
-
–
Critical LMCA stenosis which complicates secure PCI of culprit lesion placed either in LAD or CX
-
–
Isolated LMCA ostial and/or shaft lesion accompany culprit lesion.
-
–
Elderly with favorable anatomy providing complete revascularization if elective procedure is not possible (patient demands)
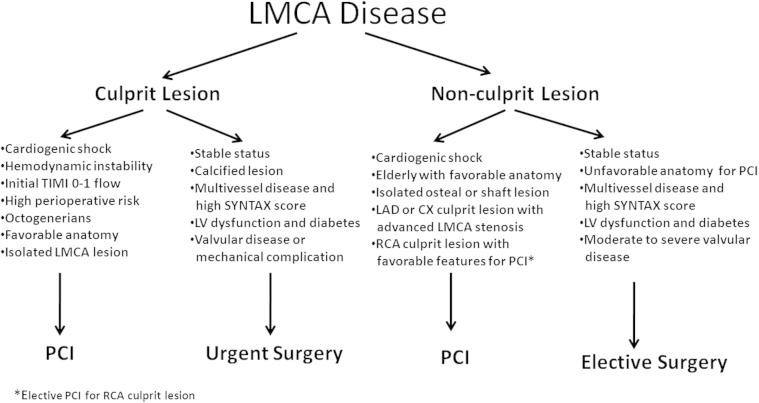
In stable patients with moderately stenotic distal LMCA lesion, target vessels should be revascularized initially, and elective LMCA assessment and intervention should be scheduled after a certain period of time. A systematic algorithm for LMCA disease in patients with acute coronary syndrome is summarized in Fig. 1.
Figure 1.
A systematic algorithm for LMCA disease in patients with acute coronary syndrome.
Conclusion
In the setting of acute coronary syndromes, percutaneous intervention of unprotected LMCA lesions can be performed with reliable results in selected patients. Cardiogenic shock and hemodynamic instability are obligatory indications for PCI, although associated major adverse cardiac events are more frequent. Surgery can be selected for stable patients with multi-vessel diseases and/or higher SYNTAX score. Concurrent LMCA and non-LMCA culprit vessel intervention can also be performed securely with good long-term results in selected patients.
Acknowledgements
The authors report no conflict of interest regarding this work. This work was not supported by any company.
Disclosure: Authors have nothing to disclose with regard to commercial support.
References
- 1.Puricel S., Adorjan P., Oberhänsli M., Stauffer J.C., Moschovitis A., Vogel R. Clinical outcomes after PCI for acute coronary syndrome in unprotected left main coronary artery disease: insights from the Swiss Acute Left Main Coronary Vessel Percutaneous Management (SALVage) study. EuroIntervention. 2011;7(6):697–704. doi: 10.4244/EIJV7I6A112. [DOI] [PubMed] [Google Scholar]
- 2.Fajadet J., Chieffo A. Current management of left main coronary artery disease. Eur Heart J. 2012;33(1):36b–50b. doi: 10.1093/eurheartj/ehr426. [DOI] [PubMed] [Google Scholar]
- 3.Gagnor A., Tomassini F., Romagnoli E., Infantino V., Rosa Brusin M.C., Maria C. Percutaneous left main coronary disease treatment without on-site surgery back-up in patients with acute coronary syndromes: immediate and 2-year outcomes. Catheter Cardiovasc Interv. 2012;79(6):979–987. doi: 10.1002/ccd.23225. [DOI] [PubMed] [Google Scholar]
- 4.Lee M.S., Sillano D., Latib A., Chieffo A., Zoccai G.B., Bhatia R. Multicenter international registry of unprotected left main coronary artery percutaneous coronary intervention with drug-eluting stents in patients with myocardial infarction. Catheter Cardiovasc Interv. 2009;73(1):15–21. doi: 10.1002/ccd.21712. [DOI] [PubMed] [Google Scholar]
- 5.Claver E., Curós A., López-Ayerbe J., Serra J., Mauri J., Fernández-Nofrerias E. Clinical predictors of left main coronary artery disease in high-risk patients with a first episode of non-ST-segment elevation acute coronary syndrome [Article in Spanish] Rev Esp Cardiol. 2006;59(8):794–800. [PubMed] [Google Scholar]
- 6.Lee M.S., Bokhoor P., Park S.J., Kim Y.H., Stone G.W., Sheiban I. Unprotected left main coronary disease and ST-segment elevation myocardial infarction: a contemporary review and argument for percutaneous coronary intervention. JACC Cardiovasc Interv. 2010;3(8):791–795. doi: 10.1016/j.jcin.2010.06.005. [DOI] [PubMed] [Google Scholar]
- 7.Park D.W., Kim Y.H., Yun S.C., Lee J.Y., Kim W.J., Kang S.J. Long-term outcomes after stenting versus coronary artery bypass grafting for unprotected left main coronary artery disease: 10-year results of bare-metal stents and 5-year results of drug-eluting stents from the ASAN-MAIN (ASAN Medical Center-Left MAIN Revascularization) Registry. J Am Coll Cardiol. 2010;56(17):1366–1375. doi: 10.1016/j.jacc.2010.03.097. [DOI] [PubMed] [Google Scholar]
- 8.Kubo S., Kadota K., Shimada T., Ozaki M., Ichinohe T., Eguchi H. Seven-year clinical outcomes of unprotected left main coronary artery stenting with drug-eluting stent and bare-metal stent. Circ J. 2013;77(10):2497–2504. doi: 10.1253/circj.cj-13-0032. [DOI] [PubMed] [Google Scholar]
- 9.Ferrante G., Presbitero P., Valgimigli M., Morice M.C., Pagnotta P., Belli G. Percutaneous coronary intervention versus bypass surgery for left main coronary artery disease: a meta-analysis of randomised trials. EuroIntervention. 2011;7(6):738–746. doi: 10.4244/EIJV7I6A117. [DOI] [PubMed] [Google Scholar]
- 10.Ali M., Hanley A., McAdam B., O’Hanlon R., Gumbrielle T., Sheahan R. Long-term clinical outcomes after unprotected left main coronary artery stenting in an all-comers patient population. Catheter Cardiovasc Interv. 2013;82(4):E411–E418. doi: 10.1002/ccd.24861. [DOI] [PubMed] [Google Scholar]
- 11.Task Force Members, Montalescot G., Sechtem U., Achenbach S., Andreotti F., Arden C. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J. 2013;34(38):2949–3003. doi: 10.1093/eurheartj/eht296. [DOI] [PubMed] [Google Scholar]
- 12.Sim D.S., Ahn Y., Jeong M.H., Kim Y.J., Chae S.C., Hong T.J. Clinical outcome of unprotected left main coronary artery disease in patients with acute myocardial infarction. Int Heart J. 2013;54(4):185–191. doi: 10.1536/ihj.54.185. [DOI] [PubMed] [Google Scholar]
- 13.Pappalardo A., Mamas M.A., Imola F., Ramazzotti V., Manzoli A., Prati F. Percutaneous coronary intervention of unprotected left main coronary artery disease as culprit lesion in patients with acute myocardial infarction. JACC Cardiovasc Interv. 2011;4(6):618–626. doi: 10.1016/j.jcin.2011.02.016. [DOI] [PubMed] [Google Scholar]
- 14.Pedrazzini G.B., Radovanovic D., Vassalli G., Sürder D., Moccetti T., Eberli F. Primary percutaneous coronary intervention for unprotected left main disease in patients with acute ST-segment elevation myocardial infarction the AMIS (Acute Myocardial Infarction in Switzerland) plus registry experience. JACC Cardiovasc Interv. 2011;4(6):627–633. doi: 10.1016/j.jcin.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 15.Abdelmalak H.D., Omar H.R., Mangar D., Camporesi E.M. Unprotected left main coronary stenting as alternative therapy to coronary bypass surgery in high surgical risk acute coronary syndrome patients. Ther Adv Cardiovasc Dis. 2013;7(4):214–223. doi: 10.1177/1753944713488637. [DOI] [PubMed] [Google Scholar]
- 16.Alam M., Huang H.D., Shahzad S.A., Kar B., Virani S.S., Rogers P.A. Percutaneous coronary intervention vs. coronary artery bypass graft surgery for unprotected left main coronary artery disease in the drug-eluting stents era – an aggregate data meta-analysis of 11,148 patients. Circ J. 2013;77(2):372–382. doi: 10.1253/circj.cj-12-0747. [DOI] [PubMed] [Google Scholar]
- 17.Sadowski M., Gutkowski W., Janion-Sadowska A., Gąsior M., Gierlotka M., Janion M. Acute myocardial infarction due to left main coronary artery disease: a large multicenter national registry. Cardiol J. 2013;20(2):190–196. doi: 10.5603/CJ.2013.0033. [DOI] [PubMed] [Google Scholar]
- 18.Zhao C., Wang X., Wu X., Cui L. Early and long-term outcomes after percutaneous coronary intervention of unprotected left main coronary disease with drug-eluting stents in patients with non-ST-elevation acute coronary syndrome. Can J Cardiol. 2011;27(6):743–748. doi: 10.1016/j.cjca.2011.05.010. [DOI] [PubMed] [Google Scholar]
- 19.Grundeken M.J., Vis M.M., Beijk M.A., Kikkert W.J., Damman P., Kloek J.J. Clinical outcomes after percutaneous or surgical revascularisation of unprotected left main coronary artery-related acute myocardial infarction: a single-centre experience. Heart. 2013;99(10):690–699. doi: 10.1136/heartjnl-2012-303402. [DOI] [PubMed] [Google Scholar]
- 20.Vis M.M., Beijk M.A., Grundeken M.J., Baan J., Jr., Koch K.T., Wykrzykowska J.J. A systematic review and meta-analysis on primary percutaneous coronary intervention of an unprotected left main coronary artery culprit lesion in the setting of acute myocardial infarction. JACC Cardiovasc Interv. 2013;6(4):317–324. doi: 10.1016/j.jcin.2012.10.020. [DOI] [PubMed] [Google Scholar]
- 21.Mehta R.H., Lopes R.D., Ballotta A., Frigiola A., Sketch M.H., Jr, Bossone E. Percutaneous coronary intervention or coronary artery bypass surgery for cardiogenic shock and multivessel coronary artery disease? Am Heart J. 2010;159(1):141–147. doi: 10.1016/j.ahj.2009.10.035. [DOI] [PubMed] [Google Scholar]