Abstract
Objectives: Although there is nowadays wide agreement on bacteria being the main etiologic agents of periodontal disease, their sole presence cannot damage periodontal tissues in all subjects. This suggests that an individual response and an adaptation to a certain quantity of bacterial biofilm can occur without the disease progressing and vice versa. Depression, stress and anxiety have not been confirmed yet as risk conditions but, in some observational studies, they have been identified as potential risk factors of periodontal disease. The current study aims at investigating the role which these psychological disorder have in the onset and progression of advanced stage periodontitis.
Materials and methods: The case selection was carried out by means of clinical and radiological periodontal assessment involving a total of 108 subjects, both male and female, aged between 24 and 67. Patients were then divided in two groups of 54 patients each: the first group included patients with severe periodontal disease, the second group was formed by periodontally healthy subjects. Clinical assessment was performed by a sole examiner who selected and divided periodontopathic patients from non-periodontopathic ones. From the current study were excluded: patients with systemic pathologies; smokers; patients taking antidepressant drugs; pregnant women.
Results: For what concerns depression, in the group of periodontopathic patients it was found that the 62.5% of them were depressed, against the 38.86% in the group of periodontally healthy subjects. For the other two psychological conditions taken into consideration, anxiety and stress, it emerged a different percentage of subjects with anxiety in the periodontal group (31.48%) against healthy controls (20.37%).
Conclusions: For each of the psychological variables considered (depression, anxiety, stress), a significant correlation could be observed with periodontal disease, it can be therefore be suggested that the importance these disturbs have in the onset and progress of the dental disease which supports the existing available data in literature.
The innovative aspect of this research was the focus on the assessment of compliance, monitoring the ability of periodontal patients to follow oral hygiene instructions aiming at the improving and keeping their own periodontal condition, even though this takes more time than the control group.
Keywords: Psychopatologic Traits, Adult Chronic Periodontitis
Introduction
Psychosomatics can be defined as that branch of medicine which relates mind to body, emotional and affective world to somatic disorder, trying to highlight and understand the influence exerted by psychic disorders on the body. The connection between disorder and its psychic cause refers back to the holistic vision of human body in which mind and body are strictly intertwined.
Anxiety, stress and depression have not been proved yet as risk factors of the periodontal disease, but some observational studies support this kind of correlation 1,2,3.
A variety of studies, as reported in 2007 by Johnson et al. 4, show that, although it is now well-established that bacteria are the main etiological agents of the periodontal disease, their sole presence does not suffice in producing advanced tissue destruction in all subjects. This suggests that an individual response and an adaptation to a certain quantity of bacterial biofilm can occur without the pathology progressing and vice versa. Environmental risk factors such as smoke and diabetes mellitus can modify not only the host's response, but also the progression, severity and outcome of the periodontal disease. Other factors such as depression, stress and anxiety were not confirmed as absolute risk condition, but in some observational studies they were identified as potential risk factors for periodontal disease. The biological plausibility for this correlation is supported by studies showing that psychosocial conditions such as depression and exposure to stress agents can affect the host's immune response making him/her more susceptible to the development of pathologic conditions affecting periodontal health 5.
The aim of the present study is to investigate the role psychic disorders have in the onset and progression of advanced stage periodontitis; this study also provided for an analysis of psychopathologies like anxiety, stress and depression. It was furthermore carried out a perspective assessment aiming at assessing the compliance to periodontal treatment in patients with depression.
Materials and Methods
Case selection
The main objective of the present study is to assess if in patients with advanced stage periodontal disease, the prevalence of psychopathologies is more relevant than in the healthy population from a periodontal point of view. A further objective of the current research is to compare compliance in a subgroup of periodontopathic patients with moderate/severe depression against non-depressed patients.
For this reason we decided to carry out the investigation on an overall sample including a group of periodontopathic patients and a group (of the same size) of periodontally healthy subjects.
The selection of participants was dependent on clinic and radiological periodontal assessment involving 108 individuals, both male and female, aged between 24 and 67.
All the participants filled in an informed consent form; the Ethics Committee of the Policlinico General Hospital approved this study.
Clinic assessments were performed by a sole examiner who selected and divided periodontopathic patients from non-periodontopathic ones. All the values relative to the different periodontal assessments for each patient were recorded in personal periodontal files. The main periodontal parameters analyzed to evaluate the presence or absence of the disease are:
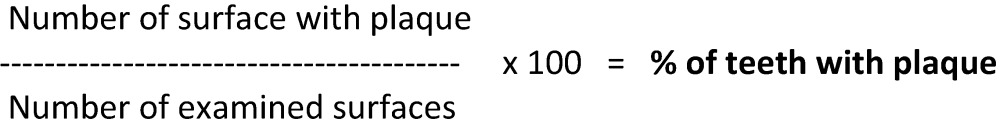
1. circumferential dichotomous indexes as: - GBI, Gingival Bleeding Index (by Ainamo e Bay, 1975) 6; - PCR, Plaque Record Control (by O'Leary et al., 1972) 7.
2. Probing depth, assessed by means of a Williams periodontal probe;
3. interradicular lesions;
4. dental mobility;
5. gingival recession.
Two groups were formed, each composed of 54 patients: the first group included subjects with severe forms of periodontal disease, the second included periodontally healthy subjects.
The advanced stage periodontal disease group was composed of 54 patients (31 women, 23 men) aged between 24 and 67 cared at the Clinic of Periodontology of Dental School at Bari State University. 22 of the 54 patients aged between 24 and 50, the remaining part of the group, between 51 and 67.
The group of periodontally healthy subjects was composed of 54 patients (40 women, 14 men) aged between 24 and 67; 38 out of 54 patients aged between 24 and 43, the remaining part of the sample, between 44 and 67.
Three different psychological tests were administered to each of the 108 patients.
From the study were excluded:
- subjects with systemic pathologies;
- smokers;
- subjects taking antidepressant drugs;
- pregnant women.
The psychological analysis (based on the use of psychometry) in our study was based on the compiling of “self-assessment” scales, filled in by the patient, which were different from the “assessment” scales compiled by the observer whose major constraints are correlated to the interpretation by the latter.
Three tests were administered: Interview for Recent Life Events (o IRLE) by Paykel 8; Sympton Check List (o SCL-90) by Derogatis 9; Beck Depression Inventory (o BDI) by Aaron T. Beck 10.
In order to test the potential correlation between periodontal disease and psychological factors, we performed a specific statistic assessment using the t-Student test.
Results
In the course of the current study two variables were taken into account: periodontal condition (dependent variable) and psychological dimension (independent variable) of the subjects.
In order to establish a correlation between periodontal condition and psychological factors, it seemed necessary to quantify the periodontal variable by means of the attribution of a range of values for each single assessed periodontal parameter [Table 1].
Table 1.
Numerical values assigned to each periodontal parameter analyzed
| Parameter | Clinical evidence | Value attributed |
|---|---|---|
| O' Leary Index or Plaque Control Record (PCR) | 0 | 0 |
| < 10% | 1 | |
| > 10% | 2 | |
| Gingival bleeding index (GBI) | 0 | 0 |
| < 20% | 1 | |
| > 20% | 2 | |
| Probing depth | physiological if ≤ 3mm | equal to the number of mm |
| pathological if > 3mm | equal to the number of mm | |
| Dental mobility | 0 | 0 |
| 1° | 1 | |
| 2° | 3 | |
| 3° | 6 | |
| Furcations | 0 | 0 |
| 1° | 1 | |
| 2° | 2 | |
| 3° | 3 | |
| Recessions | 0 | 0 |
| ≤ 20% | 1 | |
| > 20% | 2 |
During the clinic assessment, in subjects with periodontal disease we recorded the overall values ranging from a minimum of 10 to a maximum of 25, whereas in severe forms of periodontal disease is possible to observe any degree of Plaque Control Record (PCR) and Gingival Bleeding Index (GBI), a sounding depth ≥ 5 mm, the presence of recessions 2mm, the involvement of furcations of different degree and the presence of dental mobility [Table 2].
Table 2.
Parameters and total scores related to periodontal condition of periodontal disease subjects.
| Evaluation | Mean | Standard deviation |
|---|---|---|
| PCR | 1,83 | 0,38 |
| GBI | 1,83 | 0,38 |
| PD | 6,30 | 1,16 |
| DM | 2,43 | 1,68 |
| F | 1,63 | 0,78 |
| CAL | 1,31 | 0,61 |
PCR: Plaque Record Control; GBI: Gingival bleeding index
PD: Probing depth; DM: Dental mobility; F: Furcations; CAL: Recessions
In the group of periodontally healthy subjects, instead, we recorded values ranging from 3 to 7 considering that in the absence of periodontal disease the Plaque Control Record (PCR) is usually ≤ 10% and Gingival Bleeding Index (GBI) is < 20%, the sounding depth never exceeds the physiological 3 mm corresponding to the periodontal biological amplitude and that the presence of recessions, the involvement of furcations or dental mobility cannot be detected [Table 3].
Table 3.
Parameters and total scores related to periodontal condition of periodontally healthy subjects
| Evaluation | Mean | Standard deviation |
|---|---|---|
| PCR | 1,44 | 0,69 |
| GBI | 0,93 | 0,70 |
| PD | 2,56 | 0,50 |
| DM | - | - |
| F | - | - |
| CAL | - | - |
PCR: Plaque Record Control; GBI: Gingival bleeding index
PD: Probing depth; DM: Dental mobility; F: Furcations; CAL: Recessions
After the analysis of the obtained data, it was possible to evaluate the percentage of patients with depression in both groups.
A significant discrepancy emerged in percentage terms across the two groups [Table A]:
Table A.
Percentage of depression in healthy and periodontopathic patients.
| Absence of depression | Mild depression |
Moderate depression |
Severe depression |
Anxiety | |
|---|---|---|---|---|---|
| Periodontopathic | 37.03% | 33.33% | 18.07% | 11.1% | 31.48% |
| Healthy | 61.10% | 22.20% | 14.81% | 1.85% | 20.37% |
It was then possible to assess if the periodontal condition correlated to the psychological conditions of anxiety and depression by means of linear regression model which enabled the realization of dispersion graphs for a simpler visualization and interpretation of the degree of correlation (i.e. linear dependence) between variables.
It emerged:
- a positive correlation between the periodontal condition of the whole sample of patients and the score obtained on Beck Depression Inventory (BDI) testing the presence or absence of depression;
- a positive correlation between the periodontal condition of the whole sample of patients and the score obtained on Symptom Check List (SCL) testing the presence or absence of anxiety.
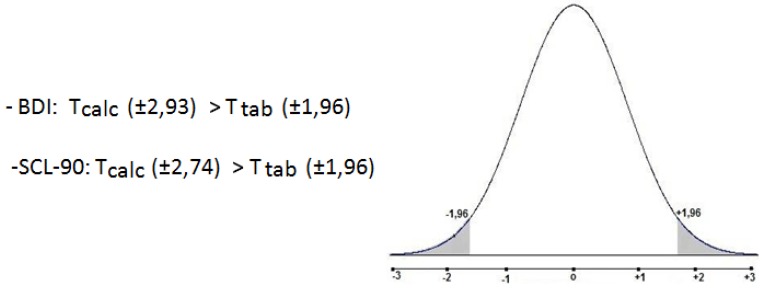
Furthermore, we carried out the comparative statistical analysis by means of the statistic test t-Student which highlighted what follows: [Figure 1]
Figure 1.
Comparative statistic analysis between indexes BDI and SCL-90 using the t-student test.
- a significant difference between the means of BDI obtained in periodontopathic and healthy subjects. The Tcalc (±2,93) resulting from the statistic comparison of the samples results to be higher than T tab (±1,96) calculated according to the number of subjects studied and using specific standard tables and considering a margin for error α/2 = 0.025.
It was therefore possible to accept the alternative hypothesis of the correlation between the two variables. [Table B]
Table B.
BDI averages obtained for periodontal patients and healthy subjects.
| Mean BDI value | Tcalc | T tab | |
|---|---|---|---|
| Periodontopathic | 16.70 | ± 2.93 | ±1.96 |
| Healthy | 11.42 |
Caption: BDI: Beck Depression Inventory by Aaron T. Beck;
Tcalc: calculation of the test statistic;
T tab: researched limit in statistic tables in correspondence of α/2.
- a statistically significant difference between the SCL-90 mean values of both groups (periodontopathic and healthy). The obtained Tcalc (±2.74) differs from T tab (±1.96) [Table C] and it therefore falls within the acceptance area of the alternative hypothesis thus enabling to claim that also in this case, a correlation between the two variables exists.
Table C.
SCL-90 averages obtained for periodontal patients and healthy subjects.
| Mean SLC-90 value | Tcalc | T tab | |
|---|---|---|---|
| Periodontopathic | 0.74 | ± 2.74 | ±1.96 |
| Healthy | 0.46 |
Caption: SCL-90: Symptom Check List di Derogatis;
Tcalc: calculation of the test statistic;
T tab: researched limit in statistic tables in correspondence of α/2.
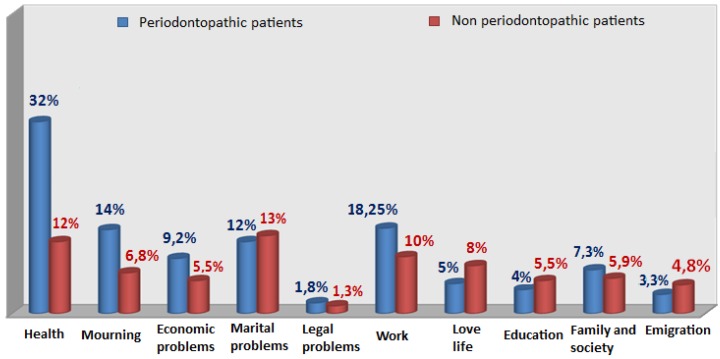
For what concerns stress, the assessment was performed counting, for each subject, the number of stressful life events belonging to the different categories the Paykel stressful life events scale is composed of: health, grief, economic problems, marital problems, legal problems, work, love life, upbringing, family and society, emigration.
From the obtained data we acquired a percentage and realized an explicative histogram of the higher, even though limited, presence of stressful life events in periodontopathic subjects [Figure 2]:
Figure 2.
Percentage of stressful events in the two groups in exam. (Interview for Recent Life Events (IRLE) of Paykel)
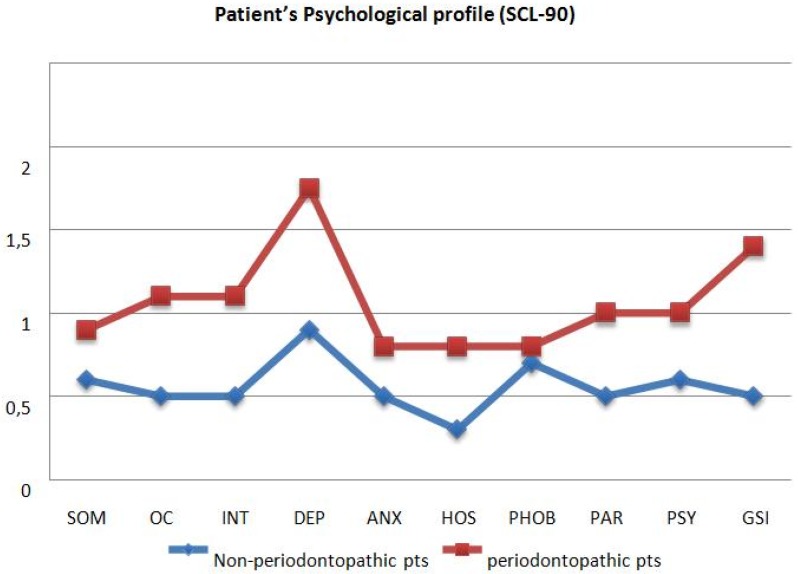
Finally, by entering the values given to each of the questions in SCL-90 in a database, then elaborated with Microsoft Excel, it was possible to outline an overall psychological profile for each examined patient and then, to compare the mean values of the outcomes for both groups. Whereas the discrepancy between groups is evident for what concerns depression, the curve trend of the values for anxiety is less significant. [Figure 3]
Figure 3.
Comparison of the psychological profile between pariodontopathic and non-periodontopathic patients. Caption: SOM: Somatization; OC: Obsessio-Compulsion; INT: interpersonal sensivity; DEP: depression; ANX: Anxiety; HOS: Hostility; PHOB: Phobic Anxiety; PAR: paranoyd idealization; PSY: Psychoticism; GSI: Global Index.
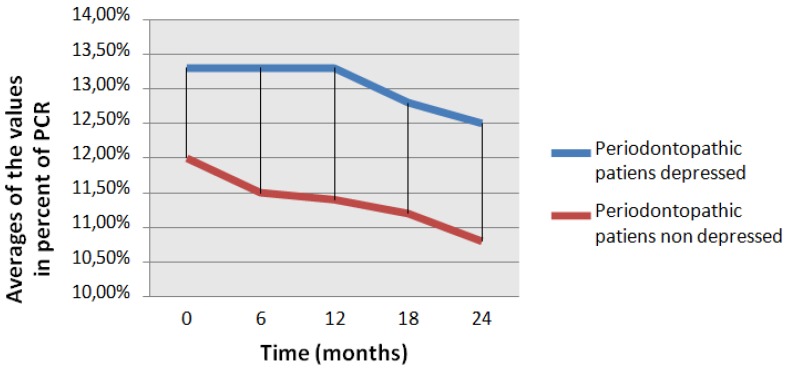
The assessment of the compliance was carried out observing the percentage values over time obtained by the interpretation of Plaque Record Control (PCR):
 |
We calculated the mathematical mean of the values for each time (time 0, six months, twelve months, eighteen months, twenty-four months) of both groups, each composed of 8 periodontopathic patients. [Table D]
Table D.
Mean values in percentage of terms Plaque Control Record in depressed patients and non-depressed
| Mean values in percentage of terms Plaque Control Record | |||||
|---|---|---|---|---|---|
| Time 0 | 6 months | 12 months | 18 months | 24 months | |
|
Depressed (mild/moderate depression) |
13.30% | 13.30% | 13.30% | 12.8% | 12.5% |
| Non-depressed | 12% | 11.5% | 11.4% | 11.2% | 10.8% |
The trend over time of compliance is graphically represented in Figure 4.
Figure 4.
Compliance of patients with and without depression.
Discussion
Literature contains various studies on animals and man carried out with different methods, both observational and experimental, aiming at assessing the correlation between psychopathologic conditions and periodontal alterations 2,3.
The variety of methods applied in these works 11,12 as well as the frequent absence of a control group or the lack of controlled studies due to confused variables relating to periodontal disease, has so far made it difficult to draw inferences about the real effects of psychosocial factors on the pathogenesis and progression of periodontal disease. The discrepancy of the findings reported in different studies could be explained taking into consideration the different psychometric instruments used to assess the psychological variable. We should bear in mind that, at the present time, there is not any biological marker or any other measurable instrument able to define with reasonable certainty the presence of psychic disorders or their degree of severity 13.
In literature, there are therefore not any definitive data about the impact of these conditions as risk factors for periodontal tissue 5. Still, some studies confirm a positive correlation between the abovementioned psychological variables and periodontal disease, showing convincing links between such pathological conditions 5,14,15,16.
The analysis of the findings relative to the whole group of examined subjects highlighted the possibility of higher psychological alterations in patients with periodontal disease than in the overall population.
For what concerns depression, for instance, in the group of periodontopathic subjects it was found that the percentage of depressed subjects amounted to 62.5% against the 38.86% found in the group of periodontally healthy subjects. Particularly, it was found a high percentage (33.33%) of patients with mild depression in the group of periodontopathic patients against healthy ones (22.20%). Similarly significant was the discrepancy of findings concerning moderate depression (periodontopathic subjects: 18.07%; non-periodontopathic subjects: 14.81%) and severe depression (periodontopathic subjects: 11.10%; non-periodontopathic subjects: 1.85%).
From the statistical analysis it emerged a positive correlation between the periodontal condition in the patient sample and their score on the Beck Depression Inventory (BDI) inferable from the trend of the slanted line (mean value) from left to right and bottom-up. It can be observed that the periodontal variable increase is paralleled by the psychological one, as the periodontal condition deteriorated, the depression test score increased.
The application of the t-Student test highlighted a statistically significant difference between periodontopathic patients and healthy subjects for what concerns the mean values obtained by the evaluation of the Beck Depression Inventory (BDI). The Tcalc (±2,93) value obtained by the statistical comparison of the two samples is higher than the T tab (±1,96). These values were found on the basis of the number of subjects studied and by the use of dedicated standard tables with margin for error α/2 = 0.025. From this we can infer that that it is possible to accept the hypothesis of a correlation between the two variables.
Although a series of hypothesis have been put forward, it is still unclear what the real correlation between periodontal disease and depression is. This is likely to be attributed to both behavioural reasons, since depressed patients tend to neglect oral hygiene and periodic dental check-ups because of their condition determining a decrease in self-care 17, and to neurophysiologic reasons since it has been suggested that these patients show decreased surveillance with consequent increase in tiredness and inactivity. From a neuroendocrine point of view, the correlation between periodontitis and depression has been attributed, for stress as well, to an impaired immune response caused by the hypothalamus-hypophysis- adrenal system.
Some studies on depressed patients have shown significant alterations in both humoral immune response and cell response 18,19,20,21. Moreover, according to some studies, in patients with Major Depressive Disorders and Anxiety Disorders it often happens to find bruxism signs 22 and abuse of substances like alcohol and/or smoke where the patients “seek refuge” because of their psychological suffering 23. This leads to a decrease in saliva secretion with consequent higher predisposition to the action of periodontal pathogenic micro-organisms 24.
The elaboration of the psychological profile of each examined patient by means of Scl-90 enabled us to broadly distinguish the two analysed groups; it was found a significant discrepancy between groups, especially for what concerns depression. Other variables (evaluable by means of the administration of the same test) like somatisation, obsession-compulsion, interpersonal sensitivity, hostility, paranoid ideation, psychoticism - except for anxiety and phobic anxiety - result to be less represented in healthy subject than in periodontopathic ones. It is therefore interesting to observe how many other psychic disorders other than those analysed can affect the periodontal condition of the patients; it would be also stimulating to use these data as a starting point for a future study.
For what concerns the other two psychological variables considered in the current study, anxiety and stress, for the former it was possible to apply the same investigation methods used for depression, for the latter a less complex assessment was carried out. It emerged a different percentage of anxious subjects in the periodontopathic group compared to healthy controls. It was estimated a value of 31.48% for the first group and a value of 20.37% for the second group.
These data suggest that the hypothesis of the correlation between the periodontal variable and the psychological one can be confirmed. To support this finding, both the linear regression model, applied to this case, and the statistical analysis performed with the t-Student test may gain importance.
From the linear regression model it was found a positive correlation between the periodontal condition of the whole sample of patients and their score on Symptom Check List (SCL-90) inferable from the trend of the slanted line (mean value) from left to right and bottom-up (see graph at page 73) . From the t-Student test it emerged a statistically significant difference between periodontopathic patients and healthy subjects in the mean values obtained from the assessment of the test on anxiety. The Tcalc (±2,74) value was in fact higher than the Ttab (±1.96) identified on t he basis of the number of subjects studied and using dedicated standard tables with a margin for error α/2 = 0.025. From this it can be inferred that it exists a correlation between the two variables.
The assessment of stress was instead performed counting, for each single subject, the number of stressful events belonging to the different categories composing the Paykel Life Events Scale: health, grief, economic problems, marital problems, legal problems, work, love life, upbringing, family and society, emigration. The percentage of stressful events concerning “health”, “grief”, “economic problems” and “work” was significantly higher in periodontopathic patients than in non-periodontopathic ones. For what concerns “marital problems”, “love life”, “upbringing”, “family and society” and “emigration” the percentages of stressful events are slightly more relevant for non-periodontopathic subjects. For the remaining category (“legal problems”) it was not found a significant discrepancy in the analysed groups.
Finally, only few studies report findings following periodontal treatment in depressed subjects and from them we can infer that in patients with depression and chronic periodontitis, treatment results to be less favourable than in non-depressed subjects 25.
The present study was therefore informed by the assessment over time of the values of plaque index or of compliance, taking into consideration two subgroups of patients composed of 8 periodontopathic patients each, distinguished according to the presence or absence of depression. We examined the 8 subjects which we could carefully monitor over time and who, over about two years, regularly underwent all the periodontal checks and treatments. This psychopathologic condition was preferred to others for various reasons: both for the high percentage of positive scores on BDI which drew the examiner's attention; for the study of literature revealing confused conclusions about the correlation between periodontal disease and depression and for the presence of only few studies about the periodontal treatment in subjects with depression. We found that, despite the starting values of the plaque index being different across the two subgroups (subjects with moderate/severe depression: 13.30%; subjects without depression: 12%), for both groups a certain decrease in the accumulation of plaque over 24 months took place.
Whereas in subjects with depression it could be observed an initial decrease in the plaque index after 12 months of treatment and motivation to oral hygiene, in healthy subjects after only 6 months an improvement of the periodontal condition could be observed 26. This data show a faster learning of oral hygiene measures by subjects without depression, but it does not nonetheless exclude the ability of depressed patients to follow the dentist's advice concerning oral health.
In depressed patients, in particular, a 0.8% decrease in plaque was observed, amounting to 1.2% in healthy subjects.
Although the data obtained in our research were positive, it is of the utmost importance to consider that depression is usually associated with an impaired preventive coping with consequent lack of focus on personal and oral care.
In periodontopathic patients, in which some the characteristic features of depression could be found, it would nonetheless be necessary to carry out frequent motivational recalls and oral hygiene training associated with scaling and root-planing sessions. As it is well known, the success of periodontal treatment is dependent on the patient's ability to guarantee an optimal level of oral hygiene: this is in fact the condition sine qua non for the keeping of periodontal health.
Conclusions
The present study was focused on the analysis of the possible correlation between psychological factors and periodontal disease.
The series of findings obtained overtly suggests that the starting hypothesis of correlation can be broadly confirmed.
We found, for each of the psychological variables examined, a significant correlation with periodontal disease which enabled us to confirm the important role these disorders have in the onset and in the progression of the dental pathology supporting the present available data in literature.
The innovative aspect of this research was the focus on the assessment of compliance, observing over time the ability of some periodontopathic patients with depression to follow adequate oral hygiene instruction aimed at the improvement and keeping of their periodontal condition.
The analysis of our data showed that the hypothesis of the existence of a link between psychopathological conditions and periodontal disease has solid ground. However, it is necessary to consider that the limitations of the present work which are mainly imputable to the missed administration of psychological tests after a specific period of time and also to the limited number of subjects belonging to the examined subgroup for the assessment of compliance.
Notwithstanding the abovementioned limitations, the findings of this study confirm, in line with a great deal of data existing in literature, that two seemingly far from each other dimensions such as oral cavity and psychological conditions (depression, anxiety and stress) are indeed closely related.
References
- 1.Gupta OP, Tiwarri OS, Salimeno T Jr, Allen DR. Neuropsychiatric disorders and periodontal disease. Ann Dent. 1993;52(2):28–33. Review. [PubMed] [Google Scholar]
- 2.Monteiro da Silva AM, Oakley DA, Newman HN. et al. Psychosocial factors and adult onset rapidly progressive periodontitis. J Clin Periodontol. 1996 Aug;23(8):789–94. doi: 10.1111/j.1600-051x.1996.tb00611.x. [DOI] [PubMed] [Google Scholar]
- 3.Moss ME, Beck JD, Kaplan BH. et al. Exploratory case-control analysis of psychosocial factors and adult periodontitis. J Periodontol. 1996 Oct;67(10 Suppl):1060–9. doi: 10.1902/jop.1996.67.10s.1060. [DOI] [PubMed] [Google Scholar]
- 4.Johnson NW, Griffiths GS, Wilton JMA. et al. Detection of high-risk groups and individuals for periodontal diseases. Evidence for the existence of high-risk groups and individuals and approaches to their detection. J Clin Periodontol. 1988;15(5):276–82. doi: 10.1111/j.1600-051x.1988.tb01584.x. Review. [DOI] [PubMed] [Google Scholar]
- 5.Peruzzo DC, Benatti BB, Ambrosano GM. et al. A systematic review of stress and psychological factors as possible risk factors for periodontal disease. J Periodontol. 2007;78(8):1491–504. doi: 10.1902/jop.2007.060371. Review. [DOI] [PubMed] [Google Scholar]
- 6.Ainamo J, Bay I. Problems and proposals for recording gingivitis and plaque. Int Dent J. 1975 Dec;25(4):229–35. [PubMed] [Google Scholar]
- 7.O'Leary TJ, Drake RB, Naylor JE. The plaque control record. J Periodontol. 1972 Jan;43(1):38. doi: 10.1902/jop.1972.43.1.38. [DOI] [PubMed] [Google Scholar]
- 8.Paykel ES, Prusoff BA, Uhlenhut EH. Scaling of live events. Arch Gen Psychiatry. 1971 Oct;25(4):340–7. doi: 10.1001/archpsyc.1971.01750160052010. [DOI] [PubMed] [Google Scholar]
- 9.Derogatis L.R, Lipman R.S, Rickels K. The Hopkins Symptom Checklist (HSCL). A self report symptom inventory. Behav Sci. 1974 Jan;19(1):1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- 10.Beck A.T, Steer R.A, Carbin M.G, Psychometric properties of the Beck Depression Inventory. Twenty-five years of evaluation. Clinical Psychology Review. Elsevier, 1 (8): 77-100; 1988. [Google Scholar]
- 11.Mengel R, Bacher M, Flores-de-Jacoby L. Interactions between stress, interleukin-1ß, interleukin-6 and cortisol in periodontally diseased patients. J Clin Periodontol. 2002 Nov;29(11):1012–22. doi: 10.1034/j.1600-051x.2002.291106.x. [DOI] [PubMed] [Google Scholar]
- 12.Merchant AT, Pitiphat W, Ahmed B. et al. A prospective study of social support, anger expression and risk of periodontitis in men. J Am Dent Assoc. 2003 Dec;134(12):1591–6. doi: 10.14219/jada.archive.2003.0104. [DOI] [PubMed] [Google Scholar]
- 13.Menezes PR, Nascimento AF. Validation and reliability of evaluation scales in psychiatry (in Portuguese) In: Gorenstein C, Andrade LHSG, Zuardi AW, editors. Clinical Evaluation Scales in Psychiatry and Psychopharmacology, 1st ed, vol 2. Sao Paulo: Lemos; 2000. pp. 23–28. [Google Scholar]
- 14.Hilgert JB, Hugo FN, Bandeira DR. et al. Stress, cortisol, and periodontitis in a population aged 50 years and over. J Dent Res. 2006 Apr;85(4):324–8. doi: 10.1177/154405910608500408. [DOI] [PubMed] [Google Scholar]
- 15.Ng SK, Keung Leung W. A community study on the relationship between stress, coping, affective dispositions and periodontal attachment loss. Community Dent Oral Epidemiol. 2006 Aug;34(4):252–66. doi: 10.1111/j.1600-0528.2006.00282.x. [DOI] [PubMed] [Google Scholar]
- 16.Rosania AE, Low KG, McCormick CM. et al. Stress, depression, cortisol, and periodontal disease. J Periodontol. 2009 Feb;80(2):260–6. doi: 10.1902/jop.2009.080334. [DOI] [PubMed] [Google Scholar]
- 17.Monteiro da Silva A.M, Newman H.N.O. Psychosocial factors in inflammatory periodontal diseases. A review. J Clin Periodontol. 1995 Jul;22(7):516–26. doi: 10.1111/j.1600-051x.1995.tb00799.x. [DOI] [PubMed] [Google Scholar]
- 18.Lorenz T, van Anders S. Interactions of sexual activity, gender, and depression with immunity. J Sex Med. 2014 Apr;11(4):966–79. doi: 10.1111/jsm.12111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maes M, Meltzer H.Y, Scharpe S. et al. Relationships between lower plasma L-tryptophan levels and immune-inflammatory variables in depression. Psychiatry Res. 1993 Nov;49(2):151–65. doi: 10.1016/0165-1781(93)90102-m. [DOI] [PubMed] [Google Scholar]
- 20.Maes M, Meltzer H.Y, Stevens W. et al. Natural killer cell activity in major depression: relation to circulating natural killer cells, cellular indices of the immune response and depressive phenomenology. Prog Neuropsychopharmacol Biol Psychiatry. 1994 Jul;18(4):717–30. doi: 10.1016/0278-5846(94)90079-5. [DOI] [PubMed] [Google Scholar]
- 21.Maes M. Evidence for an immune response in major depression: a review and hypothesis. Prog Neuropsychopharmacol Biol Psychiatry. 1995 Jan;19(1):11–38. doi: 10.1016/0278-5846(94)00101-m. [DOI] [PubMed] [Google Scholar]
- 22.Corsalini M, Di Venere D, Pettini F. et al. Temporomandibular disorders in burning mouth syndrome patients: an observational study. Int J Med Sci. 2013 Oct 29;10(12):1784–9. doi: 10.7150/ijms.6327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Di Venere D, Corsalini M, Stefanachi G. et al. Quality of life in fibromyalgia patients with craniomandibular disorders. Open Dent J. 2015 Jan 30;9:9–14. doi: 10.2174/1874210601509010009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Friedlander AH, Mahler ME. Major depressive disorder Psychopathology, medical management and dental implications. J Am Dent Assoc. 2001 May;132(5):629–38. doi: 10.14219/jada.archive.2001.0240. [DOI] [PubMed] [Google Scholar]
- 25.Vettore MV, Leao AT, Monteiro Da Silva AM. et al. The relationship of stress and anxiety with chronic periodontitis. J Clin Periodontol. 2003 May;30(5):394–402. doi: 10.1034/j.1600-051x.2003.10271.x. [DOI] [PubMed] [Google Scholar]
- 26.Ballini A, Scattarella A, Crincoli V. et al. Surgical treatment of gingival overgrowth with 10 years of follow-up. Head Face Med. 2010 Aug 12;6:19. doi: 10.1186/1746-160X-6-19. [DOI] [PMC free article] [PubMed] [Google Scholar]