Abstract
Introduction
Few studies have examined the longitudinal associations of fitness or changes in fitness on the risk of developing dyslipidemias. This study examined the associations of: (1) baseline fitness with 25-year dyslipidemia incidence; and (2) 20-year fitness change on dyslipidemia development in middle age in the Coronary Artery Risk Development in young Adults (CARDIA) study.
Methods
Multivariable Cox proportional hazards regression models were used to test the association of baseline fitness (1985–1986) with dyslipidemia incidence over 25 years (2010–2011) in CARDIA (N=4,898). Modified Poisson regression models were used to examine the association of 20-year change in fitness with dyslipidemia incidence between Years 20 and 25 (n=2,487). Data were analyzed in June 2014 and February 2015.
Results
In adjusted models, the risk of incident low high-density lipoprotein cholesterol (HDL-C), high triglycerides, and high low-density lipoprotein cholesterol (LDL-C) was significantly lower, by 9%, 16%, and 14%, respectively, for each 2.0-minute increase in baseline treadmill endurance. After additional adjustment for baseline trait level, the associations remained significant for incident high triglycerides and high LDL-C in the total population and for incident high triglycerides in both men and women. In race-stratified models, these associations appeared to be limited to whites. In adjusted models, change in fitness did not predict 5-year incidence of dyslipidemias, whereas baseline fitness significantly predicted 5-year incidence of high triglycerides.
Conclusions
Our findings demonstrate the importance of cardiorespiratory fitness in young adulthood as a risk factor for developing dyslipidemias, particularly high triglycerides, during the transition to middle age.
Introduction
A dyslipidemic profile, characterized by low levels of high-density lipoprotein cholesterol (HDL-C) and high levels of triglycerides (TGs) and low-density lipoprotein cholesterol (LDL-C), is strongly associated with an increased risk of cardiovascular disease (CVD) morbidity and mortality.1–6 Strong evidence also indicates that lower levels of cardiorespiratory fitness and decreases in fitness over time are independently associated with increased risk of CVD morbidity and mortality.7–13 In general, fitness levels are positively associated with HDL-C and inversely with non–HDL-C, LDL-C, and TG levels.14–18 However, only a few longitudinal population studies have documented the influence of changes in fitness over time on changes in the lipid profile7,12,19,20 or on the risk of developing dyslipidemias. In a previous investigation of the Coronary Artery Risk Development in young Adults (CARDIA) cohort, 7-year change in fitness was directly related to change in HDL-C, independent of change in body weight, whereas inverse associations between changes in fitness and changes in LDL-C and TGs appeared to be mediated by changes in body weight.21
CARDIA includes objective measurements of fitness at baseline and Year 20, along with lipid variables measured at eight different examinations across a period of 25 years, thus providing a unique opportunity to examine the association of fitness and dyslipidemia during the transition from young adulthood to middle age. Therefore, the purpose of the present study was to examine: (1) the association of baseline fitness with the risk of developing dyslipidemias over 25 years of follow-up; and (2) the association between 20-year changes in fitness level and the incidence of dyslipidemias between Years 20 and 25 in the CARDIA cohort. We hypothesize that lower levels of baseline fitness are associated with higher risk of incident dyslipidemias over 25 years and that larger decreases in fitness over 20 years are associated with higher risk of incident dyslipidemias between Years 20 and 25.
Methods
Study Population
Details of recruitment, study design, and methods of the CARDIA Study have been published elsewhere.22 The initial examination included 5,115 black and white men and women aged 18–30 years recruited to represent proportionate racial, sex, age, and education groups from four U.S. communities: Birmingham, AL; Chicago, IL; Minneapolis, MN; and Oakland, CA. Seven follow-up examinations (Years 2, 5, 7, 10, 15, 20, and 25) have been conducted from the time of initiation of the study in 1985–1986 through Year 25 (2010–2011), with retention rates (% of original cohort) of 91%, 86%, 81%, 79%, 74%, 72%, and 72%, respectively. All participants provided written informed consent, and IRBs from each field center approved the study annually.
Assessment of Fitness Level
Fitness level was measured in eligible participants at baseline and Year 20 by a symptom-limited graded exercise treadmill test using a modified Balke protocol, which consisted of up to nine 2-minute stages of progressively increasing difficulty.23 For the present analysis, exercise test data were determined valid if participants achieved ≥2.0 minutes on the treadmill tests (99.8% met criteria at baseline, 99.2% at Year 20). Baseline and Year 20 fitness was defined as the duration of the symptom-limited exercise treadmill test in minutes at the baseline and Year 20 examinations, respectively. Change in fitness was calculated as Year 20 exercise test duration minus baseline duration.
Lipid Measurements
In the present study, fasted lipid measures from baseline and Years 5, 7, 10, 15, 20, and 25 were used for analysis. Total cholesterol and TG levels were measured enzymatically, HDL-C was determined after precipitation with dextran sulfate–magnesium chloride, and LDL-C was calculated by using the Friedewald equation. Detailed descriptions of these methods and the extensive quality control procedures have been published previously.24,25
Definitions of Dyslipidemias
The incidence of three dyslipidemic traits defined using National Cholesterol Evaluation Program (NCEP) Adult Treatment Panel (ATP) III criteria26 were analyzed: low HDL-C, <40 mg/dL; high TGs, ≥200 mg/dL; and high LDL-C, ≥160 mg/dL or self-reported use of lipid-lowering medication. The incidence of dyslipidemia over 25 years was determined after excluding participants with prevalent dyslipidemia at baseline (n=611 with low HDL-C, n=97 with high TGs, n=318 with high LDL-C) and was defined as the first occurrence of dyslipidemia beginning with Year 5, whether the dyslipidemia was maintained or not. The 5-year incidence of dyslipidemia was determined among participants that did not have prevalent dyslipidemia at Year 20 but developed dyslipidemia by the Year 25 examination.
Lipid Medications
A dichotomous variable (yes/no) for lipid medications was created for each examination based on usage of one or more of the following drug classes: statins, ezetimibe, gemfibrozil, and niacin. Lumping together the lipid medications gave similar 25-year incidence rates of high LDL-C as compared to using statins alone, as statin usage accounted for ≥94% of total lipid medication usage across examinations. Furthermore, although statins are recommended in diabetics with a goal of LDL-C <70 mg/dL, we believe very few individuals were misclassified as being dyslipidemic because they were diagnosed as diabetic in the current analysis. The number of participants with diabetes across the exams was relatively low, at 73, 118, 143, 185, 222, and 324 (at Year 5, 7, 10, 15, 20, 25, respectively), with only 1%, 0.8%, 0%, 7%, 22%, and 42% of diabetics taking a statin at these time points. Thus, aside from Year 25 when 42% of diabetics were taking a statin, the use of statins among diabetics was low, as was the overall prevalence of diabetes in the cohort to begin with.
Other Measurements
Age, race, education, cigarette smoking status, alcohol consumption, and medication use (medication bottles were examined by the interviewer) were ascertained by interview at all examinations. Height and weight were measured and BMI was calculated.
Statistical Analysis
Multivariable Cox proportional hazards regression analyses were used to calculate hazard ratios (HRs) and 95% CIs for the association between baseline fitness (continuous variable) and the incidence of dyslipidemia over 25 years of follow-up. Time-to-event in person-years was calculated from the baseline examination until dyslipidemia was ascertained or until the last examination, whichever came first. Before modeling, we tested and confirmed that the proportional hazards assumption was valid using time × baseline fitness interaction terms for each trait (p>0.05). We evaluated the presence of effect modification by race and sex at baseline using multiplicative interaction terms in Cox proportional hazards models. Significant interactions (p<0.05) were found between baseline fitness and sex for incident low HDL-C and between baseline fitness and race for incident high TGs. Thus, results are presented in the total population and stratified by race and sex for all traits.
All models were adjusted for age, examination center, baseline BMI, and the following time-varying covariates (i.e., value at the time of dyslipidemia identification or last follow-up visit): smoking (ever versus never), lipid medication status (yes versus no), education (highest grade/year completed), and alcohol consumption (mL/day) (Model 1). Additional models also adjusted for baseline lipid trait value (Model 2). Models in the total population adjusted for sex and race, whereas models stratified by race or sex did not adjust for the stratified variable. Sex-stratified models in women also adjusted for menopausal status. Adjusting for change in BMI as a time-varying covariate in the models did not change the results, thus we report models without change in BMI. As taking lipid medications is part of the definition of high LDL-C, lipid medication status was not included as a variable in models for incident high LDL-C. For baseline fitness, HRs were calculated per 2.0-minute increase in treadmill time (i.e., per increment in exercise test stage completed). Poisson regression models were used to compare the incidence rates of each dyslipidemia across the following sex-specific quartiles of baseline fitness (in minutes): men, Q1 ≤10.0, 10.0< Q2 <12.0, 12.0< Q3 <13.25, Q4 ≥13.25; women, Q1 ≤6.95, 6.95< Q2 <8.0, 8.0< Q3 <9.7, Q4 ≥9.7.
Modified Poisson regression models27 were used to examine the association of 20-year change in fitness and baseline fitness with the incidence of dyslipidemia between the Year 20 and Year 25 examinations. Owing to the relatively low number of incident cases, we did not stratify the models by sex or race. After testing the univariate association between incident dyslipidemia and 20-year fitness change or baseline fitness, we statistically adjusted for age, race, sex, examination center, smoking status at Year 20, Year 20 lipid medication use (HDL-C and TG models only), Year 20 BMI, and Year 20 lipid level. Chi-square tests were used to test whether the incidence of dyslipidemia between Years 20 and 25 differed between participants above and below the 20-year fitness change median (men, –3.45 minutes; women, –2.55 minutes).
All models were run separately for each dyslipidemic phenotype, thus resulting in differing sample sizes between phenotypes. Statistical significance was determined as p<0.05. Analyses were conducted in June 2014 and February 2015 using SAS, version 9.3.
Results
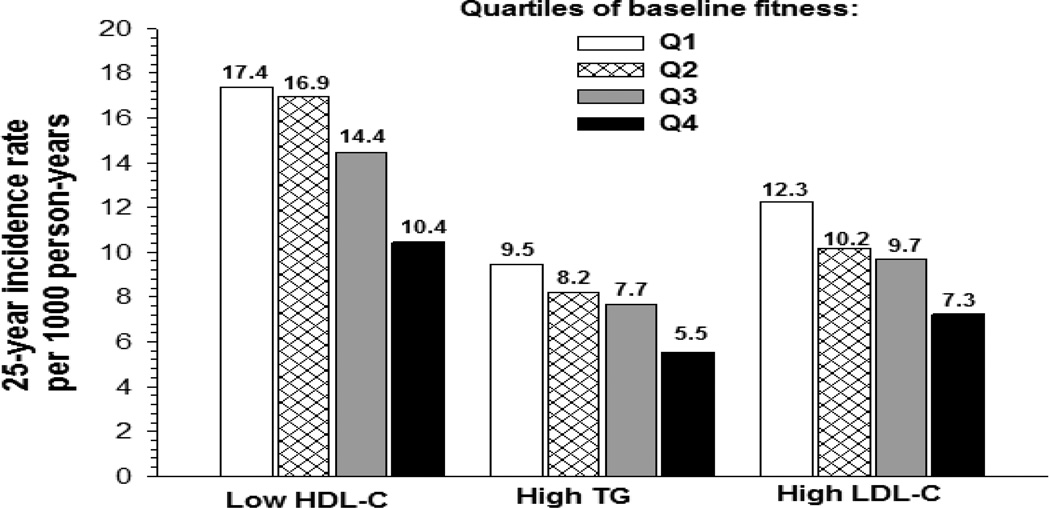
Baseline characteristics of the analytic sample overall and stratified by sex or race are shown in Table 1. Over 25 years, the rate of incident dyslipidemia (per 1,000 person-years) was 14.5 (n=1,096 cases) for low HDL-C, 7.6 (n=711) for high TGs, and 9.7 (n=879) for high LDL-C. The 25-year incidence rates per 1,000 person-years for low HDL-C, high TGs, and high LDL-C were higher in men (24.4, 11.7, 11.8) and whites (15.2, 9.7, 10.2) compared with women (8.4, 4.7, 8.1) and blacks (13.8, 5.6, 9.2), respectively. We found an inverse relationship (p<0.0001 for trend) between the 25-year incidence rate of each dyslipidemic trait and sex-specific quartiles of baseline fitness (Figure 1). The highest quartile of baseline fitness (Q4) had a significantly (p<0.0001) lower incidence rate than the other three quartiles for each dyslipidemic trait.
Table 1.
Baseline Characteristics in the Total Sample and Stratified by Sex or Race
| Total | Women | Men | Blacks | Whites | |
|---|---|---|---|---|---|
| N | 4,898 | 2,654 | 2,244 | 2,507 | 2,391 |
| Age, yrs | 24.8 (3.6) | 24.9 (3.7) | 24.8 (3.6) | 24.3 (3.8) | 25.4 (3.4)b |
| Smoking, % | |||||
| Never | 56.6 | 56.9 | 56.2 | 57.6 | 55.6 |
| Former | 13.2 | 13.8 | 12.4 | 8.8 | 17.7 |
| Current | 30.2 | 29.3 | 31.4 | 33.7 | 26.6 |
| BMI, kg/m2 | 24.4 (4.9) | 24.4 (5.6) | 24.4 (3.9) | 25.2 (5.5) | 23.6 (4.0)b |
| Treadmill test duration, min | 9.8 (2.8) | 8.2 (2.2) | 11.7 (2.3)a | 9.0 (2.8) | 10.7 (2.6)b |
| HDL-C, mg/dL | 53.1 (13.2) | 55.6 (12.9) | 50.2 (12.9)a | 54.5 (13.3) | 51.7 (13.0)b |
| TG, mg/dL | 72.8 (48.0) | 66.5 (36.6) | 80.3 (57.9)a | 66.8 (38.0) | 79.1 (56.0)b |
| LDL-C, mg/dL | 109.1 (31.3) | 108.5 (30.7) | 109.8 (31.9) | 109.6 (32.3) | 108.6 (30.1) |
Data are presented as means (SD) for continuous variables.
p<0.0001 for difference between sexes.
p<0.0001 for difference between races.
Figure 1.
25-year incident rates of dyslipidemias by sex-specific quartiles of baseline fitness in CARDIA. The actual incidence rates for each group are given above the histogram bar. p<0.0001 for trend across quartiles for all four traits.
Baseline fitness was significantly and inversely associated with the incidence of low HDL-C, high TGs, and high LDL-C in the total population in Model 1 (Table 2). For each additional 2.0 minutes of treadmill duration (i.e., each additional stage completed), the risk of incident low HDL-C, high TGs, and high LDL-C was lower by 9%, 16%, and 14%, respectively. These associations were significant in both men and women for high TGs and high LDL-C, whereas the association with low HDL-C was only observed in men. After adjusting for baseline trait value (Model 2), the associations remained significant in the total population for high TGs and high LDL-C and in men and women for high TGs (Table 2). No other dyslipidemias were associated with baseline fitness in either sex in Model 2. The inverse association between baseline fitness and incident dyslipidemia appeared to be limited to whites for all three dyslipidemic traits, regardless of the model (Table 2).
Table 2.
Association of Baseline Fitness With the Development of Dyslipidemias Over 25 Years
| Low HDL-C (<40 mg/dL) |
High TG (≥200 mg/dL) |
High LDL-C (≥160 mg/dL) |
|
|---|---|---|---|
| Baseline treadmill test duration (per 2.0 min increment) |
HR (95% CI) | HR (95% CI) | HR (95% CI) |
| Total Population | N=3,910 (1,081 cases) | N=4,359 (699 cases) | N=4,507 (869 cases) |
| Model 1 | 0.91 (0.86–0.97) | 0.84 (0.77–0.90) | 0.86 (0.80–0.93) |
| Model 2 | 0.98 (0.92–1.04) | 0.88 (0.81–0.95) | 0.92 (0.85–0.99) |
| Men | N=1,678 (693 cases) | N=1,957 (451 cases) | N=1,896 (459 cases) |
| Model 1 | 0.91 (0.84–0.97) | 0.85 (0.77–0.93) | 0.89 (0.81–0.98) |
| Model 2 | 0.96 (0.89–1.04) | 0.88 (0.81–0.98) | 0.94 (0.85–1.04) |
| Women | N=2,222 (386 cases) | N=2,387 (246 cases) | N=2,436 (408 cases) |
| Model 1 | 0.90 (0.80–1.02) | 0.80 (0.69–0.93) | 0.84 (0.74–0.94) |
| Model 2 | 0.98 (0.86–1.11) | 0.82 (0.71–0.96) | 0.90 (0.80–1.02) |
| Blacks | N=1,992 (517 cases) | N=2,180 (254 cases) | N=2,281 (400 cases) |
| Model 1 | 0.95 (0.87–1.04) | 0.88 (0.77–1.002) | 0.90 (0.80–1.007) |
| Model 2 | 0.99 (0.90–1.09) | 0.95 (0.83–1.08) | 0.93 (0.83–1.05) |
| Whites | N=1,918 (564 cases) | N=2,179 (445 cases) | N=2,226 (469 cases) |
| Model 1 | 0.91 (0.84–0.99) | 0.83 (0.75–0.91) | 0.85 (0.77–0.94) |
| Model 2 | 0.98 (0.90–1.07) | 0.86 (0.77–0.95) | 0.92 (0.83–1.02) |
Values are presented as HR (95% CI) per 2.0 min increment in baseline treadmill time. Model 1 adjusted for age, center, baseline BMI, lipid meds, smoking, education, alcohol consumption, and race and/or sex (when appropriate). Model 2 adjusted for Model 1 variables plus baseline trait value (e.g., baseline HDL-C). Both models in women adjusted for menopausal status. Number at risk and number of incident cases is given for each group for each dyslipidemic trait. Boldface indicates statistical significance (p<0.05).
Treadmill duration decreased 2.87±2.0 minutes or 28.0±21.6% between the baseline and Year 20 tests in those with valid lipid measures at both Years 20 and 25 (n=2,487). Baseline fitness (r = −0.42, p<0.0001) was significantly correlated with changes in fitness over 20 years. Between the Year 20 and 25 examinations, the incidence of low HDL-C was 3.0%, high TGs 5.0%, and high LDL-C 12.9%. Although participants who developed dyslipidemia between Years 20 and 25 experienced significantly (p≤0.01) larger adjusted mean 20-year declines in fitness (4%–6%) compared with those who did not (Appendix Figure 1), the 5-year incidence of dyslipidemias did not differ between participants that were above or below the 20-year fitness change median (Appendix Table 1).
Table 3 shows the results from univariate and multivariable Poisson regression models for the association of baseline and 20-year change in fitness with incident dyslipidemia between Years 20 and 25. In unadjusted models (Model 1), 20-year fitness change was significantly associated with incident dyslipidemia, as the risk of incident low HDL-C decreased by 30% and for high LDL-C by 10% for each 2.0-minute (or 1-stage) lesser decline in exercise test duration from baseline to Year 20. In multivariable models (Models 2 and 3), no associations between 20-year fitness change and incident dyslipidemia were found (Table 3). Baseline fitness was significantly associated with the incidence of high TGs between Years 20 and 25 in both multivariable models (Models 2 and 3), with the risk of incident high TGs decreasing by 26%–34% for each additional stage (2.0 minutes) completed during the baseline maximal exercise test (Table 3). Overall, we found that fitness measured at baseline performed as well as or better than 20-year fitness change in terms of associations with incident dyslipidemias between Years 20 and 25.
Table 3.
Association of Baseline Fitness and 20-Year Fitness Change With Incident Dyslipidemias Between Years 20 and 25
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| Low HDL-C (n=61 cases) | N=2,059 | N=2,042 | N=2,042 |
| 20-year fitness change | 0.70 (0.55–0.90) | 0.85 (0.67–1.09) | 0.91 (0.72–1.15) |
| Baseline fitness | 1.11 (0.93–1.33) | 0.83 (0.68–1.02) | 0.97 (0.79–1.19) |
| High TG (n=113 cases) | N=2,269 | N=2,252 | N=2,252 |
| 20-year fitness change | 0.87 (0.75–1.02) | 0.97 (0.83–1.14) | 1.06 (0.90–1.25) |
| Baseline fitness | 0.93 (0.83–1.05) | 0.66 (0.57–0.76) | 0.74 (0.63–0.87) |
| High LDL-C (n=273 cases) | N=2,125 | N=2,110 | N=2,110 |
| 20-year fitness change | 0.90 (0.81–0.995) | 0.96 (0.85–1.08) | 0.95 (0.85–1.07) |
| Baseline fitness | 0.88 (0.81–0.95) | 0.93 (0.82–1.04) | 0.94 (0.84–1.06) |
Data are presented as risk ratio (95% CI) per 2.0 min lesser decline in 20-year fitness change or 2.0 increment in baseline fitness.
Boldface indicates statistical significance (p<0.05).
N, Number at risk; n, number of incident cases
Each model was run individually for each fitness trait. Model 1 = univariate, no adjustments.
Model 2 = covariates included baseline or 20-year fitness change, age, sex, race, examination center, year 20 BMI, year 20 smoking status, and year 20 lipid medication status (HDL-C and TG models only). Model 3 = Model 2 + year 20 lipid trait value (e.g., year 20 HDL-C).
Discussion
We found that higher cardiorespiratory fitness measured in young adulthood was independently associated with reduced risk of developing high TGs during the transition to middle age in both men and women. These findings were independent of baseline TG levels, baseline BMI, BMI at the censored visit (data not shown), and changes in BMI (data not shown), among other covariates, suggesting that fitness may play an important protective role in the development of high TGs. For example, the incidence rate of high TGs over 25 years was 42% lower in the highest quartile of baseline fitness compared with the lowest quartile. Furthermore, baseline fitness level was a significant predictor of incident high TGs between Years 20 and 25, whereas 20-year change in fitness was not. Therefore, our results suggest that cross-sectional measures of fitness appear to be just as valuable in predicting subsequent high TGs at the population level. We found that the association of fitness with incident high TGs differed based on race and sex. The association of baseline fitness with incident high TGs over 25 years appeared to be limited to white participants only, as no significant associations were found in blacks. Hypothesizing about the potential mechanisms underlying these racial differences is difficult given the limitations of the study design and complexity of the phenotypes. In general, blacks tended to have higher BMI and HDL-C and lower TGs and fitness levels than whites. It may be that the beneficial lipid profile yet lower fitness levels of blacks counteract each other and result in a null association between fitness and incident dyslipidemias.
The NCEP ATP III recommends lifestyle changes, including regular physical activity, as part of the initial primary therapy for elevated TGs and low HDL-C, with pharmacologic therapy recommended based primarily on LDL-C levels.26 Furthermore, regular physical activity is recommended for all patients being treated pharmacologically for lipid disorders because it helps to improve the dyslipidemic profile and manage other risk factors. Although several longitudinal studies have shown that more–physically active individuals tend to have a better plasma lipid profile than their inactive counterparts,28–31 these studies primarily relied on self-reported physical activity levels and did not take into account inter-individual variation in fitness levels. Fitness can be measured more precisely than physical activity, and thus may be more clinically useful clinically for the detection of associations with health outcomes. The magnitude of association of fitness with lipid traits has been shown to be stronger than the association of physical activity with these traits,19,32 including a previous report from CARDIA.21 Our results in young and middle-aged adults complement those from the Childhood Determinants of Adult Health Study, a population-based cohort study of Australian children aged 7–15 years at baseline that completed follow-up examinations 20 years later, with both time points including objective fitness assessments.20 The authors found that participants who developed low HDL-C in adulthood had significantly larger decreases in fitness over 20 years compared with those who had normal HDL-C levels at both time points. However, the authors found no association of fitness change with the tracking of TG or LDL-C levels from childhood to adulthood.20 More research is needed in large, diverse cohort studies of both adolescents and adults with multiple objective measures of fitness to determine the associations between fitness and the risk of incident dyslipidemias over time.
Strengths and Limitations
The strengths of our study include extended follow-up, standardized protocols for the assessment of phenotypes and dyslipidemia determination based on measured plasma lipid levels, a large population-based sample balanced by race and sex, and, most importantly, the use of objective measures of fitness at multiple time points. Our study represents the longest observational study of a population-based sample of adults who have objective measures of both fitness and lipid levels.
This study also has limitations. We used treadmill test duration as an estimate of fitness instead of direct measurements of maximal oxygen uptake (V̇ O2max). Previous research has demonstrated a strong correlation (r =0.92) between test duration on a symptom-limited test and V̇. O2.33 There was a low incidence of dyslipidemias between Years 20 and 25, giving us limited power to analyze the association of 20-year fitness change with incident dyslipidemia during this time period. Furthermore, it should be noted that low baseline fitness reduced the probability of returning for Year 20 fitness testing, as those who also took the fitness test at Year 20 had significantly higher baseline fitness levels than those that did not.34 This may bias our change in fitness association results toward the null, as one would expect those with poor baseline fitness to be at higher risk of incident dyslipidemias between Years 20 and 25. However, in exploratory analyses using Cox proportional hazards models, we found that participation in the Year 20 treadmill test did not interact with baseline fitness in predicting dyslipidemias over 25 years. Lastly, the observational nature of this study does not allow us to infer causality in the association between fitness and the development of dyslipidemia.
Conclusions
These observations indicate that the measurement of fitness may be an additional and valuable tool for identifying people at increased risk of developing high TGs. They also suggest that facilitating achievement of a higher level of fitness should be an important component of public health prevention and therapeutic strategies designed to improve the lipid profile, which in turn could lower the incidence of high TGs in the population. Thus, public health policies that encourage physical activity and the maintenance of fitness with aging should be promoted.
Supplementary Material
Acknowledgments
The Coronary Artery Risk Development in Young Adults Study (CARDIA) is supported by contracts HHSN268201300025C, HHSN268201300026C, HHSN268201300027C, HHSN268201300028C, HHSN268201300029C, and HHSN268200900041C from the National Heart, Lung, and Blood Institute (NHLBI), the Intramural Research Program of the National Institute on Aging (NIA), and an intra-agency agreement between NIA and NHLBI (AG0005). NHLBI had input into the overall design and conduct of the CARDIA study. The CARDIA Fitness study is supported by R01 HL 078972.
MAS had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. This manuscript has been reviewed by CARDIA for scientific content in order to ensure consistency and accuracy.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
References
- 1.Wilson PW, Garrison RJ, Castelli WP, Feinleib M, McNamara PM, Kannel WB. Prevalence of coronary heart disease in the Framingham Offspring Study: role of lipoprotein cholesterols. Am J Cardiol. 1980;46(4):649–654. doi: 10.1016/0002-9149(80)90516-0. http://dx.doi.org/10.1016/0002-9149(80)90516-0. [DOI] [PubMed] [Google Scholar]
- 2.Gordon DJ, Probstfield JL, Garrison RJ, et al. High-density lipoprotein cholesterol and cardiovascular disease. Four prospective American studies. Circulation. 1989;79(1):8–15. doi: 10.1161/01.cir.79.1.8. http://dx.doi.org/10.1161/01.CIR.79.1.8. [DOI] [PubMed] [Google Scholar]
- 3.Laakso M, Lehto S, Penttilä I, Pyörälä K. Lipids and lipoproteins predicting coronary heart disease mortality and morbidity in patients with non-insulin-dependent diabetes. Circulation. 1993;88(4):1421–1430. doi: 10.1161/01.cir.88.4.1421. http://dx.doi.org/10.1161/01.CIR.88.4.1421. [DOI] [PubMed] [Google Scholar]
- 4.Akerblom JL, Costa R, Luchsinger JA, et al. Relation of plasma lipids to all-cause mortality in Caucasian, African-American and Hispanic elders. Age Ageing. 2008;37(2):207–213. doi: 10.1093/ageing/afn017. http://dx.doi.org/10.1093/ageing/afn017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cui Y, Blumenthal RS, Flaws JA, et al. Non-high-density lipoprotein cholesterol level as a predictor of cardiovascular disease mortality. Arch Intern Med. 2001;161(11):1413–1419. doi: 10.1001/archinte.161.11.1413. http://dx.doi.org/10.1001/archinte.161.11.1413. [DOI] [PubMed] [Google Scholar]
- 6.Jacobs DR, Jr, Mebane IL, Bangdiwala SI, Criqui MH, Tyroler HA. High density lipoprotein cholesterol as a predictor of cardiovascular disease mortality in men and women: the follow-up study of the Lipid Research Clinics Prevalence Study. Am J Epidemiol. 1990;131(1):32–47. doi: 10.1093/oxfordjournals.aje.a115483. [DOI] [PubMed] [Google Scholar]
- 7.Blair SN, Cooper KH, Gibbons LW, Gettman LR, Lewis S, Goodyear N. Changes in coronary heart disease risk factors associated with increased treadmill time in 753 men. Am J Epidemiol. 1983;118(3):352–359. doi: 10.1093/oxfordjournals.aje.a113642. [DOI] [PubMed] [Google Scholar]
- 8.Blair SN, Kohl HW, 3rd, Barlow CE, Paffenbarger RS, Jr, Gibbons LW, Macera CA. Changes in physical fitness and all-cause mortality. A prospective study of healthy and unhealthy men. JAMA. 1995;273(14):1093–1098. http://dx.doi.org/10.1001/jama.1995.03520380029031. [PubMed] [Google Scholar]
- 9.Carnethon MR, Sternfeld B, Schreiner PJ, et al. Association of 20-year changes in cardiorespiratory fitness with incident type 2 diabetes: the coronary artery risk development in young adults (CARDIA) fitness study. Diabetes Care. 2009;32(7):1284–1288. doi: 10.2337/dc08-1971. http://dx.doi.org/10.2337/dc08-1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Erikssen G, Liestol K, Bjornholt J, Thaulow E, Sandvik L, Erikssen J. Changes in physical fitness and changes in mortality. Lancet. 1998;352(9130):759–762. doi: 10.1016/S0140-6736(98)02268-5. http://dx.doi.org/10.1016/S0140-6736(98)02268-5. [DOI] [PubMed] [Google Scholar]
- 11.Kokkinos P, Myers J, Faselis C, et al. Exercise capacity and mortality in older men: a 20-year follow-up study. Circulation. 2010;122(8):790–797. doi: 10.1161/CIRCULATIONAHA.110.938852. http://dx.doi.org/10.1161/CIRCULATIONAHA.110.938852. [DOI] [PubMed] [Google Scholar]
- 12.Carnethon MR, Gidding SS, Nehgme R, Sidney S, Jacobs DR, Jr, Liu K. Cardiorespiratory fitness in young adulthood and the development of cardiovascular disease risk factors. JAMA. 2003;290(23):3092–3100. doi: 10.1001/jama.290.23.3092. http://dx.doi.org/10.1001/jama.290.23.3092. [DOI] [PubMed] [Google Scholar]
- 13.Blair SN, Kohl HW, 3rd, Paffenbarger RS, Jr, Clark DG, Cooper KH, Gibbons LW. Physical fitness and all-cause mortality. A prospective study of healthy men and women. JAMA. 1989;262(17):2395–2401. doi: 10.1001/jama.262.17.2395. http://dx.doi.org/10.1001/jama.1989.03430170057028. [DOI] [PubMed] [Google Scholar]
- 14.Marrugat J, Elosua R, Covas MI, Molina L, Rubies-Prat J. Amount and intensity of physical activity, physical fitness, and serum lipids in men. The MARATHOM Investigators. Am J Epidemiol. 1996;143(6):562–569. doi: 10.1093/oxfordjournals.aje.a008786. http://dx.doi.org/10.1093/oxfordjournals.aje.a008786. [DOI] [PubMed] [Google Scholar]
- 15.Gibbons LW, Blair SN, Cooper KH, Smith M. Association between coronary heart disease risk factors and physical fitness in healthy adult women. Circulation. 1983;67(5):977–983. doi: 10.1161/01.cir.67.5.977. http://dx.doi.org/10.1161/01.CIR.67.5.977. [DOI] [PubMed] [Google Scholar]
- 16.Grundy SM, Barlow CE, Farrell SW, Vega GL, Haskell WL. Cardiorespiratory fitness and metabolic risk. Am J Cardiol. 2012;109(7):988–993. doi: 10.1016/j.amjcard.2011.11.031. http://dx.doi.org/10.1016/j.amjcard.2011.11.031. [DOI] [PubMed] [Google Scholar]
- 17.O'Donovan G, Kearney E, Sherwood R, Hillsdon M. Fatness, fitness, and cardiometabolic risk factors in middle-aged white men. Metabolism. 2012;61(2):213–220. doi: 10.1016/j.metabol.2011.06.009. http://dx.doi.org/10.1016/j.metabol.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 18.Farrell SW, Finley CE, Grundy SM. Cardiorespiratory Fitness, LDL Cholesterol, and CHD Mortality in Men. Med Sci Sports Exerc. 2012;44(11):2132–2137. doi: 10.1249/MSS.0b013e31826524be. http://dx.doi.org/10.1249/MSS.0b013e31826524be. [DOI] [PubMed] [Google Scholar]
- 19.Andersen LB, Haraldsdottir J. Tracking of cardiovascular disease risk factors including maximal oxygen uptake and physical activity from late teenage to adulthood. An 8-year follow-up study. J Intern Med. 1993;234(3):309–315. doi: 10.1111/j.1365-2796.1993.tb00748.x. http://dx.doi.org/10.1111/j.1365-2796.1993.tb00748.x. [DOI] [PubMed] [Google Scholar]
- 20.Magnussen CG, Thomson R, Cleland VJ, Ukoumunne OC, Dwyer T, Venn A. Factors affecting the stability of blood lipid and lipoprotein levels from youth to adulthood: evidence from the Childhood Determinants of Adult Health Study. Arch Pediatr Adolesc Med. 2011;165(1):68–76. doi: 10.1001/archpediatrics.2010.246. http://dx.doi.org/10.1001/archpediatrics.2010.246. [DOI] [PubMed] [Google Scholar]
- 21.Sternfeld B, Sidney S, Jacobs DR, Jr, Sadler MC, Haskell WL, Schreiner PJ. Seven-year changes in physical fitness, physical activity, and lipid profile in the CARDIA study. Coronary Artery Risk Development in Young Adults. Ann Epidemiol. 1999;9(1):25–33. doi: 10.1016/s1047-2797(98)00030-1. http://dx.doi.org/10.1016/S1047-2797(98)00030-1. [DOI] [PubMed] [Google Scholar]
- 22.Friedman GD, Cutter GR, Donahue RP, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41(11):1105–1116. doi: 10.1016/0895-4356(88)90080-7. http://dx.doi.org/10.1016/0895-4356(88)90080-7. [DOI] [PubMed] [Google Scholar]
- 23.Sidney S, Haskell WL, Crow R, et al. Symptom-limited graded treadmill exercise testing in young adults in the CARDIA study. Med Sci Sports Exerc. 1992;24(2):177–183. http://dx.doi.org/10.1249/00005768-199202000-00004. [PubMed] [Google Scholar]
- 24.Bild DE, Jacobs DR, Liu K, et al. Seven-year trends in plasma low-density-lipoprotein-cholesterol in young adults: the CARDIA Study. Ann Epidemiol. 1996;6(3):235–245. doi: 10.1016/1047-2797(96)00005-1. http://dx.doi.org/10.1016/1047-2797(96)00005-1. [DOI] [PubMed] [Google Scholar]
- 25.Donahue RP, Jacobs DR, Sidney S, Wagenknecht LE, Albers JJ, Hulley SB. Distribution of lipoproteins and apolipoproteins in young adults The CARDIA Study. Arteriosclerosis. 1989;9(5):656–664. doi: 10.1161/01.atv.9.5.656. http://dx.doi.org/10.1161/01.ATV.9.5.656. [DOI] [PubMed] [Google Scholar]
- 26.National Cholesterol Education Program. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–3421. [PubMed] [Google Scholar]
- 27.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. http://dx.doi.org/10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 28.Monda KL, Ballantyne CM, North KE. Longitudinal impact of physical activity on lipid profiles in middle-aged adults: the Atherosclerosis Risk in Communities Study. J Lipid Res. 2009;50(8):1685–1691. doi: 10.1194/jlr.P900029-JLR200. http://dx.doi.org/10.1194/jlr.P900029-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Twisk JW, Kemper HC, Mellenbergh GJ, van Mechelen W, Post GB. Relation between the longitudinal development of lipoprotein levels and lifestyle parameters during adolescence and young adulthood. Ann Epidemiol. 1996;6(3):246–256. doi: 10.1016/1047-2797(96)00003-8. http://dx.doi.org/10.1016/1047-2797(96)00003-8. [DOI] [PubMed] [Google Scholar]
- 30.Raitakari OT, Porkka KV, Taimela S, Telama R, Rasanen L, Viikari JS. Effects of persistent physical activity and inactivity on coronary risk factors in children and young adults. The Cardiovascular Risk in Young Finns Study. Am J Epidemiol. 1994;140(3):195–205. doi: 10.1093/oxfordjournals.aje.a117239. [DOI] [PubMed] [Google Scholar]
- 31.Young DR, Haskell WL, Jatulis DE, Fortmann SP. Associations between changes in physical activity and risk factors for coronary heart disease in a community-based sample of men and women: the Stanford Five-City Project. Am J Epidemiol. 1993;138(4):205–216. doi: 10.1093/oxfordjournals.aje.a116849. http://dx.doi.org/10.1249/00005768-199305001-00419. [DOI] [PubMed] [Google Scholar]
- 32.Dvorak RV, Tchernof A, Starling RD, Ades PA, DiPietro L, Poehlman ET. Respiratory Fitness, Free Living Physical Activity, and Cardiovascular Disease Risk in Older Individuals: A Doubly Labeled Water Study. J Clin Endocrinol Metab. 2000;85(3):957–963. doi: 10.1210/jcem.85.3.6432. http://dx.doi.org/10.1210/jc.85.3.957. [DOI] [PubMed] [Google Scholar]
- 33.Pollock ML, Bohannon RL, Cooper KH, et al. A comparative analysis of four protocols for maximal treadmill stress testing. Am Heart J. 1976;92(1):39–46. doi: 10.1016/s0002-8703(76)80401-2. http://dx.doi.org/10.1016/S0002-8703(76)80401-2. [DOI] [PubMed] [Google Scholar]
- 34.Zhu N, Suarez-Lopez JR, Sidney S, et al. Longitudinal examination of age-predicted symptom-limited exercise maximum HR. Med Sci Sports Exerc. 2010;42(8):1519–1527. doi: 10.1249/MSS.0b013e3181cf8242. http://dx.doi.org/10.1249/MSS.0b013e3181cf8242. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.